Congenital Heart Defects
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Coarctation of the Aorta Interrupted Aortic Arch
T HE P EDIATRIC C ARDIAC S URGERY I NQUEST R EPORT Coarctation of the aorta In the normal heart, blood flows to the body through the aorta, which connects to the left ven- tricle and arches over the top of the heart.In coarc- tation of the aorta,the aorta is pinched (in medical terms, coarcted) at a point somewhere along its length. This pinching restricts blood flow from the heart to the rest of the body. Often, the baby also has other heart defects, such as a narrowing of the aortic arch (in medical terms,transverse aortic arch hypoplasia). Usually no symptoms are apparent at birth, but can develop within a week of birth with the closure of the ductus arteriosus. The possible conse- Diagram 2.9 Coarctation of the aorta quences of this condition are poor feeding, an 1 – pinched or coarcted aorta enlarged heart, an enlarged liver and congestive Flow patterns are normal but are reduced below the coarctation. Blood pressure is increased in ves- heart failure. Blood pressure also increases above sels leaving the aorta above the coarctation. The the constriction. broken white arrow indicates diminished blood flow through the aorta. Timing of surgery depends on the degree of coarctation. Surgery may be delayed with mild coarctation (which sometimes is not detected until adoles- cence). However, if a baby develops congestive heart failure or high blood pressure, early surgery is usually required. A baby with severe coarctation should have early surgery to prevent long-term high blood pres- sure. The coarctation can be repaired in a number of ways without opening the heart.The surgeon can remove the narrowed part of the aorta and sew the ends together, thereby creating an anastomosis. -

Cardiovascular Magnetic Resonance Pocket Guide
Series Editors Bernhard A. Herzog John P. Greenwood Sven Plein Cardiovascular Magnetic Resonance Congenital Heart Disease Pocket Guide Bernhard A. Herzog Ananth Kidambi George Ballard First Edition 2014 Congenital Pocket Guide Tetralogy / Foreword Pulmonary Atresia Standard Views TGA Difficult Scans Single Ventricle Sequential Ebstein Anomaly Segmental Analysis Coronary Artery Shunts Anomalies AV Disease / References Aortic Coarctation Terminology Series Editors Authors Bernhard A. Herzog Bernhard A. Herzog John P. Greenwood Ananth Kidambi Sven Plein George Ballard Foreword The role of cardiovascular magnetic resonance (CMR) in evaluating the adult population with congenital heart disease continues to expand. This pocket guide aims to provide a day-to-day companion for those new to congenital CMR and for those looking for a quick reference guide in routine practice. The booklet gives an overview of the most common abnormalities and interventions as well as post-operative complications. It also provides typical scan protocols, key issues and a guide for reporting for each topic. Bernhard A. Herzog Ananth Kidambi George Ballard The Cardiovascular Magnetic Resonance Pocket Guide represents the views of the ESC Working Group on Cardiovascular Magnetic Resonance and was arrived at after careful consideration of the available evidence at the time it was written. Health professionals are encouraged to take it fully into account when exercising their clinical judgment. This pocket guide does not, however, override the individual responsibility of health professionals to make appropriate decisions in the circumstances of the individual patients, in consultation with that patient and, where appropriate and necessary, the patient's guardian or carer. It is also the health professional's responsibility to verify the applicable rules and regulations applicable to drugs and devices at the time of prescription. -
How to Recognize a Suspected Cardiac Defect in the Neonate
Neonatal Nursing Education Brief: How to Recognize a Suspected Cardiac Defect in the Neonate https://www.seattlechildrens.org/healthcare- professionals/education/continuing-medical-nursing-education/neonatal- nursing-education-briefs/ Cardiac defects are commonly seen and are the leading cause of death in the neonate. Prompt suspicion and recognition of congenital heart defects can improve outcomes. An ECHO is not needed to make a diagnosis. Cardiac defects, congenital heart defects, NICU, cardiac assessment How to Recognize a Suspected Cardiac Defect in the Neonate Purpose and Goal: CNEP # 2092 • Understand the signs of congenital heart defects in the neonate. • Learn to recognize and detect heart defects in the neonate. None of the planners, faculty or content specialists has any conflict of interest or will be presenting any off-label product use. This presentation has no commercial support or sponsorship, nor is it co-sponsored. Requirements for successful completion: • Successfully complete the post-test • Complete the evaluation form Date • December 2018 – December 2020 Learning Objectives • Describe the risk factors for congenital heart defects. • Describe the clinical features of suspected heart defects. • Identify 2 approaches for recognizing congenital heart defects. Introduction • Congenital heart defects may be seen at birth • They are the most common congenital defect • They are the leading cause of neonatal death • Many neonates present with symptoms at birth • Some may present after discharge • Early recognition of CHD -
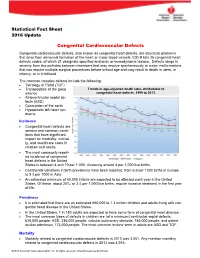
Congenital Cardiovascular Defects
Statistical Fact Sheet 2016 Update Congenital Cardiovascular Defects Congenital cardiovascular defects, also known as congenital heart defects, are structural problems that arise from abnormal formation of the heart or major blood vessels. ICD-9 lists 25 congenital heart defects codes, of which 21 designate specified anatomic or hemodynamic lesions. Defects range in severity from tiny pinholes between chambers that may resolve spontaneously to major malformations that can require multiple surgical procedures before school age and may result in death in utero, in infancy, or in childhood. The common complex defects include the following: Tetralogy of Fallot (TOF) Transposition of the great Trends in age-adjusted death rates attributable to arteries congenital heart defects, 1999 to 2013. Atrioventricular septal de- fects (ASD) Coarctation of the aorta Hypoplastic left heart syn- drome Incidence Congenital heart defects are serious and common condi- tions that have significant impact on morbidity, mortali- ty, and healthcare costs in children and adults. The most commonly report- ed incidence of congenital heart defects in the United States is between 4 and 10 per 1,000, clustering around 8 per 1,000 live births. Continental variations in birth prevalence have been reported, from 6.9 per 1000 births in Europe to 9.3 per 1000 in Asia. An estimated minimum of 40,000 infants are expected to be affected each year in the United States. Of these, about 25%, or 2.4 per 1,000 live births, require invasive treatment in the first year of life. Prevalence It is estimated that there are an estimated 650,000 to 1.3 million children and adults living with con- genital heart disease in the United States. -

Tricuspid Atresia Associated with Common Arterial Trunk and 22Q11 Chromosome Deletion
Archivos de Cardiología de México Volumen Número Octubre-Diciembre Volume 73 Number 4 October-December 2003 Artículo: Tricuspid atresia associated with common arterial trunk and 22q11 chromosome deletion Derechos reservados, Copyright © 2003 Instituto Nacional de Cardiología Ignacio Chávez Otras secciones de Others sections in este sitio: this web site: ☞ Índice de este número ☞ Contents of this number ☞ Más revistas ☞ More journals ☞ Búsqueda ☞ Search edigraphic.com 271 COMUNICACIONES BREVES Tricuspid atresia associated with common arterial trunk and 22q11 chromosome deletion Carlos Alva,* Felipe David,* Martha Hernández,* Rubén Argüero,** José Ortegón,* Arturo Martínez,* Diana López,* Santiago Jiménez,* Agustín Sánchez* Summary Resumen The case of a four-months old male with coexist- ATRESIA TRICUSPÍDEA Y TRONCO ARTERIOSO COMÚN ent tricuspid atresia and common arterial trunk is presented. The diagnois was made by cardiac Se presenta el caso de un paciente masculino catheterization and selective angiocardiography. de cuatro meses de edad con atresia tricuspí- Clinical considerations are discussed and the dea asociada a tronco arterial común. El diag- review of the available literature reveals this pa- nóstico se corroboró con cateterismo cardíaco y tient to be the tenth case reported of this very angiocardiografía selectiva. Se analiza la expre- unusual association of cardiovascular defects, sión clínica de esta excepcional asociación y se and the first with positive deletion of the 22q11 hace una revisión de la literatura. Este es el dé- chromosome. cimo caso publicado con esta inusual asociación de lesiones cardíacas y el primero con deleción del cromosoma 22q11. (Arch Cardiol Mex 2003; 73:271-274). Key words: Tricuspid atresia and common arterial trunk. -

Tricuspid Valve Guideline
Tricuspid Valve What the Nurse Caring for a Patient with Congenital Heart Disease Needs to Know Lindsey Justice, DNP, RN, CPNP-AC, Nurse Practitioner, Cardiac Intensive Care Unit, Cincinnati Children’s Hospital Medical Center Justine Mize, MSN, RN, CCRN, CPN, Professional Practice Specialist, Cardiac Intensive Care Unit, Children’s National Health System, Washington, DC Louise Callow, MSN, RN, CPNP, Nurse Practitioner, Pediatric Cardiac Surgery, University of Michigan, CS Mott Children’s Hospital, Ann Arbor, Michigan Mary Rummell, MN, RN, CPNP, CNS, FAHA Clinical Nurse Specialist, Pediatric Cardiology/Cardiac Services, Oregon Health & Science University (Retired) Embryology Occurrence: o Defects of cardiac valves are the most common subtype of cardiac malformations o Account for 25% to 30% of all congenital heart defects o Most costly and relevant CHD o Wise spectrum of congenital defects in tricuspid valve Development of the heart valves occurs during the fourth to eighth weeks of gestation- after tubular heart looping o Walls of the tubular heart consist of an outer lining of myocardium and an inner lining of endocardial cells o Cardiac jelly, extensive extracellular matrix (ECM), separates the two layers o Cardiac jelly expands to form cardiac cushions at the sites of future valves . Outflow track (OT) valves = aortic and pulmonic valves Final valves derived from endothelial-mesenchymal cells with neural crest cells from the brachial arches Valves (Semilunar) have 3 equal cusp-shaped leaflets Aortic valve incorporates coronary arteries . Atrioventricular (AV) valves = mitral and tricuspid Final valves derived entirely from endocardial cushion tissue Leaflet formed without a cusp Two leaflets associated with left ventricle (mitral) Three leaflets associated with right ventricle (tricuspid) Coordinated by complex interplay of: o Genetics o Signaling pathways that regulate cell apoptosis and proliferation o Environmental factors 1 . -

Congenital Heart Disease Parent FAQ
Congenital Heart Disease Parent FAQ achd.stanfordchildrens.org | achd.stanfordhealthcare.org About Congenital Heart Disease What is congenital heart disease? Congenital heart disease, also called congenital heart defect (CHD), is a heart problem that a baby is born with. When the heart forms in the womb, it develops incorrectly and does not work properly, which changes how the blood flows through the heart. What causes congenital heart defects? In most cases, there is no clear cause. It can be linked to something out of the ordinary happening during gestation, including a viral infection or exposure to environmental factors. Or, it may be linked to a single gene defect or chromosome abnormalities. How common is CHD in the United States among children? Congenital heart defects are the most common birth defects in children in the United States. Approximately 1 in 100 babies are born with a heart defect. What are the most common types of congenital heart defects in children? In general, CHDs disrupt the flow of blood in the heart as it passes to the lungs or to the body. The most common congenital heart defects are abnormalities in the heart valves or a hole between the chambers of the heart (ventricles). Examples include ventricular septal defect (VSD), atrial septal defect (ASD), and bicuspid aortic valve. At the Betty Irene Moore Children’s Heart Center at Stanford Children’s Health, we are known across the nation and world for treating some of the most complex congenital heart defects with outstanding outcomes. Congenital Heart Disease Parent FAQ | 2 Is CHD preventable? In some cases, it could be preventable. -

Pulmonary-Atresia-Mapcas-Pavsdmapcas.Pdf
Normal Heart © 2012 The Children’s Heart Clinic NOTES: Children’s Heart Clinic, P.A., 2530 Chicago Avenue S, Ste 500, Minneapolis, MN 55404 West Metro: 612-813-8800 * East Metro: 651-220-8800 * Toll Free: 1-800-938-0301 * Fax: 612-813-8825 Children’s Minnesota, 2525 Chicago Avenue S, Minneapolis, MN 55404 West Metro: 612-813-6000 * East Metro: 651-220-6000 © 2012 The Children’s Heart Clinic Reviewed March 2019 Pulmonary Atresia, Ventricular Septal Defect and Major Aortopulmonary Collateral Arteries (PA/VSD/MAPCAs) Pulmonary atresia (PA), ventricular septal defect (VSD) and major aortopulmonary collateral arteries (MAPCAs) is a rare type of congenital heart defect, also referred to as Tetralogy of Fallot with PA/MAPCAs. Tetralogy of Fallot (TOF) is the most common cyanotic heart defect and occurs in 5-10% of all children with congenital heart disease. The classic description of TOF includes four cardiac abnormalities: overriding aorta, right ventricular hypertrophy (RVH), large perimembranous ventricular septal defect (VSD), and right ventricular outflow tract obstruction (RVOTO). About 20% of patients with TOF have PA at the infundibular or valvar level, which results in severe right ventricular outflow tract obstruction. PA means that the pulmonary valve is closed and not developed. When PA occurs, blood can not flow through the pulmonary arteries to the lungs. Instead, the child is dependent on a patent ductus arteriosus (PDA) or multiple systemic collateral vessels (MAPCAs) to deliver blood to the lungs for oxygenation. These MAPCAs usually arise from the de- scending aorta and subclavian arteries. Commonly, the pulmonary arteries are abnormal, with hypoplastic (small and underdeveloped) central and branch pulmonary arteries and/ or non-confluent central pulmonary arteries. -

Prenatal Diagnosis, Associated Findings and Postnatal Outcome Of
J. Perinat. Med. 2019; 47(3): 354–364 Ingo Gottschalka,*, Judith S. Abela, Tina Menzel, Ulrike Herberg, Johannes Breuer, Ulrich Gembruch, Annegret Geipel, Konrad Brockmeier, Christoph Berg and Brigitte Strizek Prenatal diagnosis, associated findings and postnatal outcome of fetuses with double outlet right ventricle (DORV) in a single center https://doi.org/10.1515/jpm-2018-0316 anomalies, 30 (66.7%) had extracardiac anomalies and 13 Received September 18, 2018; accepted November 26, 2018; (28.9%) had chromosomal or syndromal anomalies. Due previously published online December 20, 2018 to their complex additional anomalies, five (11.1%) of our Abstract 45 fetuses had multiple malformations and were highly suspicious for non-chromosomal genetic syndromes, Objective: To assess the spectrum of associated anoma- although molecular diagnosis could not be provided. Dis- lies, the intrauterine course, postnatal outcome and orders of laterality occurred in 10 (22.2%) fetuses. There management of fetuses with double outlet right ventricle were 17 terminations of pregnancy (37.8%), two (4.4%) (DORV). intrauterine and seven (15.6%) postnatal deaths. Nineteen Methods: All cases of DORV diagnosed prenatally over a of 22 (86.4%) live-born children with an intention to treat period of 8 years were retrospectively collected in a single were alive at last follow-up. The mean follow-up among tertiary referral center. All additional prenatal findings survivors was 32 months (range, 2–72). Of 21 children who were assessed and correlated with the outcome. The accu- had already undergone postnatal surgery, eight (38.1%) racy of prenatal diagnosis was assessed. achieved biventricular repair and 13 (61.9%) received Results: Forty-six cases of DORV were diagnosed pre- univentricular palliation. -

Tricuspid Atresia
Br Heart J: first published as 10.1136/hrt.18.4.499 on 1 October 1956. Downloaded from TRICUSPID ATRESIA BY JAMES W. BROWN, DONALD HEATH,* THOMAS L. MORRIS, AND WILLIAM WHITAKER From the Regional Cardiovascular Centre, City General Hospital, and the University Department of Medicine, The Royal Hospital, Sheffield Received August 28, 1955 * Tricuspid atresia is an uncommon form of cardiovascular malformation which occurred as the primary lesion 16 times in Abbott's (1936) 1000 cases of congenital heart disease and in 5 per cent of 670 of Campbell's (1953) patients with cyanotic congenital heart disease. Although isolated cases, such as Hedinger's (1915) patient who was 56, have been described in adult life, most of the patients with this rare anomaly have been reported in infancy or early childhood: 9 of the 15 cases of Astley et al. (1953) were 2 years of age or under and the oldest was 11 years. The features of 8 patients with tricuspid atresia, 7 of whom were 3 years or over, and of one patient with congenital tricuspid stenosis, aged 13, are described in the present communication, where the clinical manifestations of the disease in older patients and its diagnosis by special investigation are discussed. In four of the patients who died (Cases 2, 3, 5, and 8) an account is given of the pathological findings which are considered in relation to survival. In two of these (Cases 2 and 8) a histological examinationi of the small pulmonary vessels was made and the abnormal appearances found in Case 2 are described. -

Transcatheter Device Closure of Atrial Septal Defect in Dextrocardia with Situs Inversus Totalis
Case Report Nepalese Heart Journal 2019; Vol 16(1), 51-53 Transcatheter device closure of atrial septal defect in dextrocardia with situs inversus totalis Kiran Prasad Acharya1, Chandra Mani Adhikari1, Aarjan Khanal2, Sachin Dhungel1, Amrit Bogati1, Manish Shrestha3, Deewakar Sharma1 1 Department of Cardiology, Shahid Gangalal National Heart Centre, Kathmandu, Nepal 2 Department of Internal Medicine, Kathmandu Medical College, Kathmandu,Nepal 3 Department of Pediatric Cardiology, Shahid Gangalal National Heart Centre, Kathmandu, Nepal Corresponding Author: Chandra Mani Adhikari Department of Cardiology Shahid Gangalal National Heart Centre Kathmandu, Nepal Email: [email protected] Cite this article as: Acharya K P, Adhikari C M, Khanal A, et al. Transcatheter device closure of atrial septal defect in dextrocardia with situs inversus totalis. Nepalese Heart Journal 2019; Vol 16(1), 51-53 Received date: 17th February 2019 Accepted date: 16th April 2019 Abstract Only few cases of Device closure of atrial septal defect in dextrocardia with situs inversus totalis has been reported previously. We present a case of a 36 years old male, who had secundum type of atrial septal defect in dextrocardia with situs inversus totalis. ASD device closure was successfully done. However, we encountered few technical difficulties in this case which are discussed in this case review. Keywords: atrial septal defect; dextrocardia; transcatheter device closure, DOI: https://doi.org/10.3126/njh.v16i1.23901 Introduction There are only two case reported of closure of secundum An atrial septal defect (ASD) is an opening in the atrial ASD associated in patients with dextrocardia and situs inversus septum, excluding a patent foramen ovale.1 ASD is a common totalis. -

Double Outlet Right Ventricle (DORV)
Double outlet right ventricle (DORV) Vita Zīdere, MD FRCP Consultant Paediatric and Fetal Cardiologist • Complex lesion, represents 3 % of CHD seen in fetus • Both Great Arteries arise completely or predominantly from the morphological right ventricle • Associates with increased NT, genetic and extracardiac anomalies • Double outlet right ventricle is a spectrum of abnormalities • almost always has a VSD • heterogeneous with respect to size and position of VSD and relationship of GA • individual anatomy dictates surgical approach and outcome • It poses a number of challenges • Definition • Anatomic Variability (incl. normal or abnormal AV connections) • Surgical options DORV TOF type DORV “Simple” DORV Complex DORV Always VSD: Unbalanced Ventricles AVSD (often RAI or LAI) subaortic, MV atresia subpulmonary or uncommitted; Coarctation, IAA +/-PS Discordant AV connections Criss-cross heart Normal atrial situs Patent, concordant AV connections DORV Overriding aorta Both GA (parallel) from RV “50 % rule” Subpulmonary, subaortic or uncommitted VSD TOF type DORV Anatomical repair- Repair depends from GA relationship with VSD VSD closure & PS release LV to Ao baffle ASO with baffling VSD to neo-Ao Rarely BV repair is unfeasible L G Price 2004 G Price • True override is independent of septal axis • postnatally is assessed relative to chord of circle in short axis* *BR Wilcox, AC Cook, RH Anderson. Surgical anatomy of the heart,2004 Double Outlet Right ventricle v. Tetralogy of Fallot L L R R • Perimembranous VSD, overriding aorta • Pulmonary artery