Summer Reception
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Francis Crick in Molecular Biology
2019 Asia-Pacific Conference on Emerging Technologies and Engineering (ACETE 2019) Francis Crick in Molecular Biology Sun Yongping College of Physic and Electronic Information, Inner Mongolia Normal University, Hohhot, China Keywords: Crick, DNA, Protein, Genetic Codes, Molecular Biology Abstract: This article is a tribute to Francis crick, a biophysicist who passed away on July 28, 2004. Francis crick, James Watson and Maurice Wilkins were jointly awarded the 1962 Nobel Prize for physiology or medicine for discovering the molecular structure of nucleic acids and its significance for information transfer in living material. It is pointed out that the diverse background and unique sensitivity of crick to science enabled him to have great insights into frontier research. He had a special capacity for prudent and logical thinking, which contributed so much to the development of molecular biology. Based on Francis crick’s academic achievements in molecular biology and by virtue of internal history approaches such as concept analysis and literature research, this paper is aimed at revealing the historical contributions of crick in a condensed way and to commemorate his work. 1. Introduction Francis crick (figure 1) was born on June 8, 1916 as an English citizen, and he left the world, aged 88. With lifelong devotion to scientific research, crick is credited as one of the central figures in the molecular revolution that swept through biology in the latter half of the twentieth century [1]. Keen on seeking after and tackling the profound problems, he developed a passion for biology although crick did research in physics at the beginning of his scientific life [2,3]. -

HUMAN GENE MAPPING WORKSHOPS C.1973–C.1991
HUMAN GENE MAPPING WORKSHOPS c.1973–c.1991 The transcript of a Witness Seminar held by the History of Modern Biomedicine Research Group, Queen Mary University of London, on 25 March 2014 Edited by E M Jones and E M Tansey Volume 54 2015 ©The Trustee of the Wellcome Trust, London, 2015 First published by Queen Mary University of London, 2015 The History of Modern Biomedicine Research Group is funded by the Wellcome Trust, which is a registered charity, no. 210183. ISBN 978 1 91019 5031 All volumes are freely available online at www.histmodbiomed.org Please cite as: Jones E M, Tansey E M. (eds) (2015) Human Gene Mapping Workshops c.1973–c.1991. Wellcome Witnesses to Contemporary Medicine, vol. 54. London: Queen Mary University of London. CONTENTS What is a Witness Seminar? v Acknowledgements E M Tansey and E M Jones vii Illustrations and credits ix Abbreviations and ancillary guides xi Introduction Professor Peter Goodfellow xiii Transcript Edited by E M Jones and E M Tansey 1 Appendix 1 Photographs of participants at HGM1, Yale; ‘New Haven Conference 1973: First International Workshop on Human Gene Mapping’ 90 Appendix 2 Photograph of (EMBO) workshop on ‘Cell Hybridization and Somatic Cell Genetics’, 1973 96 Biographical notes 99 References 109 Index 129 Witness Seminars: Meetings and publications 141 WHAT IS A WITNESS SEMINAR? The Witness Seminar is a specialized form of oral history, where several individuals associated with a particular set of circumstances or events are invited to meet together to discuss, debate, and agree or disagree about their memories. The meeting is recorded, transcribed, and edited for publication. -

Strategic Plan 2011-2016
Strategic Plan 2011-2016 Wellcome Trust Sanger Institute Strategic Plan 2011-2016 Mission The Wellcome Trust Sanger Institute uses genome sequences to advance understanding of the biology of humans and pathogens in order to improve human health. -i- Wellcome Trust Sanger Institute Strategic Plan 2011-2016 - ii - Wellcome Trust Sanger Institute Strategic Plan 2011-2016 CONTENTS Foreword ....................................................................................................................................1 Overview .....................................................................................................................................2 1. History and philosophy ............................................................................................................ 5 2. Organisation of the science ..................................................................................................... 5 3. Developments in the scientific portfolio ................................................................................... 7 4. Summary of the Scientific Programmes 2011 – 2016 .............................................................. 8 4.1 Cancer Genetics and Genomics ................................................................................ 8 4.2 Human Genetics ...................................................................................................... 10 4.3 Pathogen Variation .................................................................................................. 13 4.4 Malaria -

Copyright & Risk: Scoping the Wellcome Digital Library Project
CREATe Working Paper No.10 (December 2013) Copyright & Risk: Scoping the Wellcome Digital Library Project Victoria Stobo University of Glasgow Glasgow [email protected] with Prof. Ronan Deazley Dr. Ian G. Anderson University of Glasgow University of Glasgow Glasgow Glasgow [email protected] [email protected] Publication Details: This report constitutes the major deliverable from CREATe’s Work Package 1B.1, entitled Archives, Digitisation and Copyright. HTTP Identifier: http://www.create.ac.uk/publications/wp000010 This work was supported by the RCUK funded Centre for Copyright and New Business Models in the Creative Economy (CREATe), AHRC Grant Number AH/K000179/1. Acknowledgments The staff of the Copyright and Risk: Scoping the Wellcome Digital Library Project would like to thank the Wellcome Library for their generosity in allowing CREATe access to the Codebreakers Project and the Wellcome Digital Library team. Particular thanks to Sue Davies for organising the interviews at the Wellcome Library which form the basis of this report, and to those who gave up their time to speak to the RA: Simon Chaplin, Christy Henshaw, Caroline Herbert, Jenny Haynes, Toni Hardy, Chris Bird and Rada Vlatkovic; the information we gathered is much appreciated. Especial thanks are due to Caroline Herbert for providing much of the data this report is based on; and also to Caroline (again), Christy and Sue for their comments on the draft. Thanks also to the staff at the third party archives, contributors to Codebreakers and patient interview participants: Lesley Richmond and Sam Maddra at Glasgow University Archive Services; Allen Packwood, Natalie Adams and Andrew Riley at Churchill Archives Centre; Patricia Methven and Geoff Browell at King’s College London Archives and Information Management; Mila Pollock and John Zarillo at Cold Spring Harbour Laboratory Library and Archives; and Gill Furlong, Katy Makin and Steve Wright at University College London Special Collections. -

Human Genetics 1990–2009
Portfolio Review Human Genetics 1990–2009 June 2010 Acknowledgements The Wellcome Trust would like to thank the many people who generously gave up their time to participate in this review. The project was led by Liz Allen, Michael Dunn and Claire Vaughan. Key input and support was provided by Dave Carr, Kevin Dolby, Audrey Duncanson, Katherine Littler, Suzi Morris, Annie Sanderson and Jo Scott (landscaping analysis), and Lois Reynolds and Tilli Tansey (Wellcome Trust Expert Group). We also would like to thank David Lynn for his ongoing support to the review. The views expressed in this report are those of the Wellcome Trust project team – drawing on the evidence compiled during the review. We are indebted to the independent Expert Group, who were pivotal in providing the assessments of the Wellcome Trust’s role in supporting human genetics and have informed ‘our’ speculations for the future. Finally, we would like to thank Professor Francis Collins, who provided valuable input to the development of the timelines. The Wellcome Trust is a charity registered in England and Wales, no. 210183. Contents Acknowledgements 2 Overview and key findings 4 Landmarks in human genetics 6 1. Introduction and background 8 2. Human genetics research: the global research landscape 9 2.1 Human genetics publication output: 1989–2008 10 3. Looking back: the Wellcome Trust and human genetics 14 3.1 Building research capacity and infrastructure 14 3.1.1 Wellcome Trust Sanger Institute (WTSI) 15 3.1.2 Wellcome Trust Centre for Human Genetics 15 3.1.3 Collaborations, consortia and partnerships 16 3.1.4 Research resources and data 16 3.2 Advancing knowledge and making discoveries 17 3.3 Advancing knowledge and making discoveries: within the field of human genetics 18 3.4 Advancing knowledge and making discoveries: beyond the field of human genetics – ‘ripple’ effects 19 Case studies 22 4. -

Going Digital at the Wellcome Library: the Evolution of Digital Imaging and Innovation
DOI: 10.2352/issn.2168-3204.2016.1.0.33 Going Digital at the Wellcome Library: The Evolution of Digital Imaging and Innovation Danae Dracht; Wayne State University; Detroit, Michigan/USA Abstract materials for a new library.2 He focused his energy on collecting This report focuses specifically on practices within the items specifically related to medical history such as alchemy, 3 Wellcome Library and Archives in London, United Kingdom, and witchcraft, anthropology and ethnography. Wellcome intended to what the Library is doing to promote and maintain its hybrid use his independent wealth to amass his expanding medical history collections, both analog and digital. To remain a thriving and collection into a library and museum for public accessibility. While relevant information agency in a time when the value of brick-and- he did not live to see his vision properly through, by a series of mortar institutions are constantly questioned, the Wellcome continuous improvements, the Wellcome Library is now an online Library has worked to develop methods worth sharing to other open-access platform featuring cover-to-cover books, video and institutions who are striving to preserve cultural and artistic audio, entire archive collections and manuscripts, paintings, prints, 4 heritage around the world. In light of its creativity and innovation, drawings, photographs, and ephemera. the Wellcome Library warrants further discussion, especially in Although the twentieth century brought substantial changes countries outside the UK. for the Wellcome Library, the twenty-first century continues to bring significant transformations as Wellcome becomes a hybrid Introduction library featuring both the physical building with analogue information and its digital Doppelganger in a technologically “Pessimism of the intellect, optimism of the will.” advanced environment. -

Science Today, History Tomorrow
COMMENT earthquakes, tsunamis and extreme weather. RIMES is innovative but its funding is limited, making it difficult to maintain the cadre of scientists necessary to tackle specific problems. Inadequate funding also hinders the essential updat- ing of forecast modules as satellite and global forecast systems change. M. ARGLES/GUARDIAN NEWS & MEDIA M. ARGLES/GUARDIAN GLOBAL PARTNERSHIPS Partnerships that bridge the gap between the global forecasters and the user com- munity need to be established in other regions to address a range of weather hazards. The plan and type of group that forms the bridge will depend on the type of hazard being addressed. But the aim of each team is the same: to produce hazard- forecast modules based on the global fore- casts and to use them to provide warnings for the region. The team will also be responsible for updating the modules as systems and technologies change. Such partnerships can be aided by sustained funding from intergovern- mental organizations, such as the United Nations, the World Bank and USAID. My research group estimates that the cost of extended 10–15-day forecasts for south and east Asia for a wide range of hydrometeorological hazards (includ- ing slow-rise monsoon floods, droughts and tropical cyclones) is relatively small: perhaps $2 million to $3 million per year. Asia and Africa stand on the thresh- old of great economic advancement and can build resilience through the effective use of longer-range weather forecasts10. Faced with possible climate change, soci- eties that learn to cope with and mitigate hazards now will be most adept at dealing with more frequent and intense hazards in the future. -

Sir Henry Hallet Dale∗ (1875–1968)
GENERAL ARTICLE Sir Henry Hallet Dale∗ (1875–1968) Andrew Wickens Sir Henry Hallet Dale can undisputedly be accoladed as one of the greatest British pharmacologists of the twentieth cen- tury. His work was pivotal in laying down the principles of chemical neurotransmission. This article gives some account of Dale’s life and his most important discoveries, including the identification of acetylcholine as a neurotransmitter in the autonomic and somatic nervous systems. Andrew Wickens was a lecturer in Neuroscience at Introduction the University of Central Lancashire for over 25 years. The concept of chemical neurotransmission at the synapse is one His History of the Brain won of the fundamental keystones on which neuroscience is built. In- the best textbook of the year award by the British deed, without the knowledge of chemical neurotransmission, it Psychological Society in 2016. would be impossible to understand how the nervous system, including the brain, operates. Sir Henry Dale’s identification of acetylcholine as a neurotransmitter at several sites in the pe- ripheral nervous system11, including the synapse between the pre- The peripheral nervous sys- ganglionic and post-ganglionic fibres of the sympathetic system2; tem is composed of (1) the au- the post-ganglionic parasympathetic synapse; and the neuromus- tonomic nervous system which has sympathetic and parasym- 3 cular junction , were groundbreaking advances in proving that pathetic branches, and (2) the neurons communicate with each other using chemical messengers4. somatic nervous system which controls the skeletal muscles. In addition, Dale recognised that acetylcholine had both mus- carinic and nicotinic-like actions depending on its site of action. -
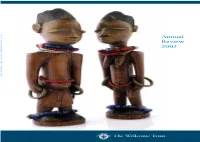
Annual Review 2003
The Wellcome Trust is an independent – 30 September 2003 1 October 2002 Review Annual Trust Wellcome The research-funding charity, established under the will of Sir Henry Wellcome in 1936. Annual It is funded from a private endowment, which is managed with long-term stability and growth in mind. Review Its mission is to foster and promote research with the aim of improving human and animal health. Its work covers four areas: 2003 Knowledge – improving our understanding of human and animal biology in health and disease, and of the past and present role of medicine in society. Resources – providing exceptional researchers with the infrastructural and career support they need to fulfil their potential. Translation – ensuring maximum health benefits are gained from biomedical research. Public engagement – raising awareness of the medical, ethical and social implications of biomedical science. www.wellcome.ac.uk Annual Review 2003 Contents 2 From the Director 6 Making a difference 8 Financial summary 10 Knowledge 16 Resources Advancing knowledge and Contributing to a long-term and understanding in the biomedical vibrant research environment. sciences and their impact on society – past, present and future. 22 Translation 28 Public engagement Advancing the translation of Trust- Engaging with the public through funded research into health benefits. informed dialogue. The cover images are of objects displayed at the ‘Medicine Man’ exhibition at the British Museum in 2003.The exhibition commemorated the 150th anniversary of the birth of Henry Wellcome. Front cover Back cover, left Back cover, right Yoruban figures representing Protective amulet said to Tobacco resuscitator kit. 34 A year at the Trust deceased twins, 1870–1910. -

Annual Report and Financial Statements
Financial year 2014 Annual Report and Financial Statements Contents Chairman’s Statement 02 Trustee’s Report 04 Vision and objects, mission, focus areas and 04 challenges Financial Review 05 Review of Past and Future Activities 09 Review of Investment Activities 15 Structure and Governance 26 Remuneration Report 32 Social Responsibility 34 Independent Auditors 36 Audit Committee Report 37 Independent Auditors’ Report 39 Consolidated Statement of Financial Activities 45 Consolidated Balance Sheet 46 Statement of Financial Activities of the Trust 47 Balance Sheet of the Trust 48 Consolidated Cash Flow Statement 49 Notes to the Financial Statements 50 Reference and Administrative Details 90 Chairman’s Statement The best research for better health Creating cultures for research who we are and what we do, and has at the frontiers of medicine helped us achieve an ever more and health integrated approach within. This was a challenging first year for The built environment is a huge our Director, Dr Jeremy Farrar. As a influence on the way we work. The clinician and a researcher with Francis Crick Institute, a partnership expertise across global health and between the Trust, the Medical infectious diseases, his skills were in Research Council, Cancer Research high demand, particularly when it UK and several of London’s became clear that the Ebola virus universities, opens next year. It, too, outbreak in West Africa this year was has been designed to encourage an epidemic of unprecedented interdisciplinary working. As well as proportion. At the same time, Jeremy enhancing research partnerships, the was listening carefully to the views of Crick will bring biomedical research We have streamlined the his new colleagues at the Wellcome together with clinical skills and many framework for our funding Trust and of the research community other scientific disciplines. -
Modelling Biological Sequences by Grammatical Inference
Modelling Biological Sequences by Grammatical Inference François Coste ICGI 2010 Tutorial Day F. Coste (Symbiose, INRIA/IRISA) ICGI Tutorial September 13, 2010 1 / 82 Motivation: learning the grammar of DNA F. Coste (Symbiose, INRIA/IRISA) ICGI Tutorial September 13, 2010 2 / 82 This talk: The Paleolithic of Modelling Biological Sequences by Grammatical Inference artistic view of old stone edge Glyptodon by Heinrich Harder Focus on working tools and specicity of modelling biosequences F. Coste (Symbiose, INRIA/IRISA) ICGI Tutorial September 13, 2010 3 / 82 Outline 1 Molecular genetics 2 Modelling a set of conserved sequences 3 Inference of grammatical structure F. Coste (Symbiose, INRIA/IRISA) ICGI Tutorial September 13, 2010 4 / 82 1 Molecular genetics Central dogma Technology Sequences annotation 2 Modelling a set of conserved sequences 3 Inference of grammatical structure F. Coste (Symbiose, INRIA/IRISA) ICGI Tutorial September 13, 2010 5 / 82 Genome Organism's hereditary information DNA Genetic heredity F. Coste (Symbiose, INRIA/IRISA) ICGI Tutorial September 13, 2010 6 / 82 DNA Genetic heredity Genome Organism's hereditary information F. Coste (Symbiose, INRIA/IRISA) ICGI Tutorial September 13, 2010 6 / 82 DNA Genetic heredity Genome Organism's hereditary information F. Coste (Symbiose, INRIA/IRISA) ICGI Tutorial September 13, 2010 6 / 82 DNA structure source: U.S. Department of Energy We wish to suggest a structure for the salt of deoxyribose nucleic acid (D.N.A.). This structure has novel features which are of considerable biological interest. John Watson and Francis Crick in Molecular Structure of Nucleic Acids. A structure for deoxyribose nucleic acid. Nature No. 4356, April 25, 1953 F. -

Annual Review 2011
Annual Review 2011 Highlights of the Wellcome Trust’s work in 2011, our 75th anniversary year, in which we redoubled our personal support for the brightest minds in research. Executive Board Wellcome Trust Mark Walport We are a global charitable foundation Director of the Wellcome Trust dedicated to achieving extraordinary Ted Bianco Director of Technology Transfer improvements in human and animal Simon Jeffreys health by supporting the brightest minds Chief Operating Officer in biomedical research and the medical David Lynn Head of Strategic Planning and Policy humanities. Clare Matterson Director of Medical Humanities Our ten-year Strategic Plan for 2010–20 and Engagement Kevin Moses provides the framework for how we intend Director of Science Funding to evolve our support to be even more John Stewart effective in achieving this aim. Head of Legal and Company Secretary Danny Truell Chief Investment Officer Our funding focuses on: As at December 2011 1. Supporting outstanding researchers 2. Accelerating the application of research 3. Exploring medicine in historical and Board of Governors cultural contexts. William Castell, Chairman Peter Rigby, Deputy Chairman Our five major challenges are: Kay Davies 1. Maximising the health benefits Peter Davies Christopher Fairburn of genetics and genomics Richard Hynes 2. Understanding the brain Anne Johnson 3. Combating infectious disease Roderick Kent Eliza Manningham-Buller 4. Investigating development, ageing Peter Smith and chronic disease As at December 2011 5. Connecting environment, nutrition