Standardization of Non-Clinical Terminologies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Penser Un Monde Par-Delà Les Frontières: Derrida Et Tirumular
Penser un monde par-delà les frontières : Derrida et Tirumular, essai de philosophie comparative Nishant Alphonse Irudayadason To cite this version: Nishant Alphonse Irudayadason. Penser un monde par-delà les frontières : Derrida et Tirumu- lar, essai de philosophie comparative. Philosophie. Université Paris-Est, 2008. Français. NNT : 2008PEST0217. tel-00462179 HAL Id: tel-00462179 https://tel.archives-ouvertes.fr/tel-00462179 Submitted on 8 Mar 2010 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. UNIVERSITÉ PARIS-EST Espace Éthique et Politique École doctorale de Cultures et Sociétés Nishant Alphonse IRUDAYADASON PENSER UN MONDE PAR-DELÀ LES FRONTIÈRES Derrida et Tirumular – Essai de philosophie comparative Directeur de thèse : Monsieur le Professeur Dominique FOLSCHEID Université Paris-Est Marne-la-vallée Rapporteurs : Examinateurs : M. le Professeur François CHENET M. le Professeur Jean GREISCH Université Sorbonne Paris IV Institut Catholique de Paris M. le Professeur Jeffrey BLOECHL M. le Professeur Ronan SHARKEY Boston College, Etats-Unis Institut Polytechnique La Salle Beauvais Thèse soutenue le 14 novembre 2008 « L’appel au dénuement total qui est l’appel à la libération totale car seul est libre celui qui n’a rien absolument rien qu’il puisse dire sien. -

Hinduism and Hindu Philosophy
Essays on Indian Philosophy UNIVE'aSITY OF HAWAII Uf,FU:{ Essays on Indian Philosophy SHRI KRISHNA SAKSENA UNIVERSITY OF HAWAII PRESS HONOLULU 1970 Library of Congress Catalog Card Number 78·114209 Standard Book Number 87022-726-2 Copyright © 1970 by University of Hawaii Press All Rights Reserved Printed in the United States of America Contents The Story of Indian Philosophy 3 Basic Tenets of Indian Philosophy 18 Testimony in Indian Philosophy 24 Hinduism 37 Hinduism and Hindu Philosophy 51 The Jain Religion 54 Some Riddles in the Behavior of Gods and Sages in the Epics and the Puranas 64 Autobiography of a Yogi 71 Jainism 73 Svapramanatva and Svapraka!;>atva: An Inconsistency in Kumarila's Philosophy 77 The Nature of Buddhi according to Sankhya-Yoga 82 The Individual in Social Thought and Practice in India 88 Professor Zaehner and the Comparison of Religions 102 A Comparison between the Eastern and Western Portraits of Man in Our Time 117 Acknowledgments The author wishes to make the following acknowledgments for permission to reprint previously published essays: "The Story of Indian Philosophy," in A History of Philosophical Systems. edited by Vergilius Ferm. New York:The Philosophical Library, 1950. "Basic Tenets of Indian Philosophy," previously published as "Are There Any Basic Tenets of Indian Philosophy?" in The Philosophical Quarterly. "Testimony in Indian Philosophy," previously published as "Authority in Indian Philosophy," in Ph ilosophyEast and West. vo!.l,no. 3 (October 1951). "Hinduism," in Studium Generale. no. 10 (1962). "The Jain Religion," previously published as "Jainism," in Religion in the Twentieth Century. edited by Vergilius Ferm. -

Kaur Inderjeet Et Al : Tanmatras-Key to Holistic Healing Through Doors Of
International Journal of Applied Ayurved Research ISSN: 2347- 6362 TANMATRAS-KEY TO HOLISTIC HEALING THROUGH DOORS OF PERCEPTIONS Kaur Inderjeet 1, Pandey Reena 2, Sharma. Giriraj .G 3 1M.D Scholar in Deptt. of Kaumarbhritya at Rishikul P.G Ayurved College, Haridwar ,Uttrakhand, India. 2Associate Prof. in Deptt. of Kaumarbhritya at Rishikul P.G College, Haridwar, Uttrakhand, India 3Associate Prof. in Deptt. of Rachna Sharir at Seth JP Govt. Ayurved College, Bhavnagar, Gujrat. India ABSTRACT We are all part of an infinite field of intelligence that orchestrates all of the activities in the universe and our sense organs are truly our only means of contact with the outside world. "Nothing is in the understanding, which was not first perceived by some of the senses." attributed to English philosopher, John Locke (1632-1704). Our senses provide the keys to unifying two systems, in particular, to bridge our outer and our inner worlds. The study of the interaction between these worlds (Healing through the Senses) interfaces with psychological processes and the nervous and immune systems of the human body. Balance your senses through both inner and outer experiences of nourishing sounds, sensations, images, tastes, and smells, and your inner pharmacy which provide natural health promoting chemicals to improve immunity, relieve anxiety and depression, normalize digestive function, and keep you pain free. Treating ourselves through the 5 senses is one of the most important ways to heal our body, mind and spirit. Ayurveda places great importance on improving the acumen and strength of the five senses. What if your taste was stronger, your eyes keener, your ears more sensitive? You would have a higher perception of reality. -

Practice of Karma Yoga
PRACTICE OF KARMA YOGA By SRI SWAMI SIVANANDA SERVE, LOVE, GIVE, PURIFY, MEDITATE, REALIZE Sri Swami Sivananda So Says Founder of Sri Swami Sivananda The Divine Life Society A DIVINE LIFE SOCIETY PUBLICATION Sixth Edition: 1995 (4,000 Copies) World Wide Web (WWW) Edition: 2001 WWW site: http://www.SivanandaDlshq.org/ This WWW reprint is for free distribution © The Divine Life Trust Society ISBN 81-7052-014-2 Published By THE DIVINE LIFE SOCIETY P.O. SHIVANANDANAGAR—249 192 Distt. Tehri-Garhwal, Uttaranchal, Himalayas, India. OM Dedicated to all selfless, motiveless, disinterested workers of the world who are struggling hard to get knowledge of the Self by purifying their minds, by getting Chitta Suddhi through Nishkama Karma Yoga OM PUBLISHERS’ NOTE The nectar-like teachings of His Holiness Sri Swami Sivananda Saraswati, the incomparable saint of the Himalayas, famous in song and legend, are too well-known to the intelligent public as well as to the earnest aspirant of knowledge Divine. Their aim and object is nothing but emancipation from the wheel of births and deaths through absorption of the Jiva with the supreme Soul. Now, this emancipation can be had only through right knowledge. It is an undisputed fact that it is almost a Herculean task for the man in the street, blinded as he is by worldly desires of diverse kinds, to forge his way to realisation of God. Not only is it his short-sightedness that stands in the way but innumerable other difficulties and obstacles hamper the progress onward towards the goal. He is utterly helpless until someone who has successfully trodden the path, comes to his aid or rescue, takes him by the hand, leads him safely through the inextricable traps and pitfalls of worldly temptation and desires, and finally brings him to his destination which is the crowning glory of the be-all and end-all of life, where all suffering ceases and all quest comes to an end. -

Legal Status of Ayurvedic, Siddha & Unani Medicines in India
Govt. of India Department of AYUSH Ministry of Health and Family Welfare Pharmacopoeial Laboratory for Indian Medicines GHAZIABAD LEGAL STATUS OF AYURVEDIC, SIDDHA & UNANI MEDICINES Dr. D.R. Lohar, M.Sc., Ph.D. Director Government of India Department of AYUSH Ministry of Health & Family Welfare PHARMACOPOEIAL LABORATORY FOR INDIAN MEDICINES GHAZIABAD PREFACE uring the past five decades, the Ayurvedic, Siddha and Unani DD Pharmaceutical Industries have provided a vast range of drugs for human use and have evolved an increasing sophistication in the production of medicaments. Manufacture and quality control of Ayurvedic, Siddha and Unani Medicines come under the purview of Drugs & Cosmetics Act. Regulatory and recommendatory standards for most of them have been released. There has been appreciable acceptance with considerable improvement in quality. Information about manufacture, sale, import of Ayurvedic, Siddha and Unani medicines in relation to pharmacopoeia and legal provisions etc. are scattered. Attempts have been made to bring various aspects of manufacture of Ayurvedic, Siddha and Unani drugs, quality control measures, legal provisions relating to quality control and the penal actions at one place so that it may become handy for manufacturers, pharmacies, and the persons involved in quality control of Ayurvedic, Siddha and Unani medicines. The need of compilation of different Ayurvedic, Siddha and Unani manufacturing processes, Good Manufacturing Practices and the related portion of Drugs & Cosmetics Act to create general awareness among the persons who are involved in this professions or who are keen in this profession was long felt. This laboratory has made an endeavor to compile such information. Besides the Legal provisions of ASU medicines, related provisions and proforma for import of medicines (which are directly or indirectly related to ASU medicines, marker compounds or materials for research or self use) have also been given for related products. -

An Analysis of the Gayatri Mantra As a Mega-Compression: a Cognitive Linguistic Perspective in Light of Conceptual Blending Theory
HTS Teologiese Studies/Theological Studies ISSN: (Online) 2072-8050, (Print) 0259-9422 Page 1 of 11 Original Research An analysis of the Gayatri mantra as a mega-compression: A cognitive linguistic perspective in light of conceptual blending theory Author: In this article, the Gayatri mantra, one of the most sacred chants to be found in Hindu lore, will 1 Suren Naicker be analysed as a blend, where an entire philosophy is compressed into these few syllables, Affiliation: which will be expounded upon here in more detail. Drawing upon insights from conceptual 1Department of Linguistics blending theory, this sacred mantra will be unpacked and explored, and it will be shown here and Modern Languages, that this ancient Rigvedic hymn is actually a nucleic compression which once tapped into University of South Africa, leads the practitioner to new insights and higher levels of spiritual awareness as the inner Pretoria, South Africa meaning unfolds. Practising Hindus around the world revere and recite this mantra with the Corresponding author: utmost reverence, and this is true of the Indian diaspora in South Africa as well. Aside from Suren Naicker, presenting this hymn through the lens of blending theory, the aim is to demonstrate and [email protected] explain why exactly this mantra is chanted with such reverence and given precedence over the many other mantras found throughout the Vedic texts. Dates: Received: 09 Nov. 2018 Keywords: Hindu philosophy; Vedas; Sankhya; cognitive linguistics; conceptual blending Accepted: 19 July 2019 theory; Gayatri mantra. Published: 27 Nov. 2019 How to cite this article: Naicker, S., 2019, ‘An analysis Introduction of the Gayatri mantra as a mega-compression: A The aim of this article is to look at a well-known mantra and expound on the importance of the chant, cognitive linguistic which is seen as a mega-compression with concentrated layers of meaning. -

Sacred Traditions the Heritage, Philosophy, & History of Yoga by Danny Arguetty
Sacred Traditions The Heritage, Philosophy, & History of Yoga By Danny Arguetty PRE-VEDIC Yoga’s roots began around 2500 BCE on the banks of the Indus River (modern day Pakistan). The Indus Valley Civilization (IVC) flourished in an area of land two times the size of California. The people began as animal herders in countryside villages but over time discovered the rich soil on the flood plains of the Valley. The fertile nutrients generated superior crop yields of cotton, sesame, peas, and barley. Soon two large urban centers Mohenjo-daro and Harappa began to boom enabling the Indus people to trade with neighboring civilizations. The two urban areas continued to thrive for over eight hundred years. Archeologists have extracted many artifacts from the region and among animal statues, pots, coins and tools they found a “square seal depicting a nude male deity with three faces, seated in yogic position on a throne, wearing bangles on both arms and an elaborate headdress. Five symbols of the Indus script appear on either side of the headdress which is made of two outward projecting buffalo style curved horns, with two upward projecting points. A single branch with three papal leaves rises from the middle of the headdress. Seven bangles are depicted on the left arm and six on the right, with the hands resting on the knees. The heels are pressed together under the groin and the feet project beyond the edge of the throne. The feet of the throne are carved with a hoof of a bovine as is seen on the bull and unicorn seals. -

Pancha Maha Bhutas (Earth-Water-Fire-Air-Sky)
1 ESSENCE OF PANCHA MAHA BHUTAS (EARTH-WATER-FIRE-AIR-SKY) Compiled, composed and interpreted by V.D.N.Rao, former General Manager, India Trade Promotion Organisation, Pragati Maidan, New Delhi, Ministry of Commerce, Govt. of India, now at Chennai. Other Scripts by the same Author: Essence of Puranas:-Maha Bhagavata, Vishnu Purana, Matsya Purana, Varaha Purana, Kurma Purana, Vamana Purana, Narada Purana, Padma Purana; Shiva Purana, Linga Purana, Skanda Purana, Markandeya Purana, Devi Bhagavata;Brahma Purana, Brahma Vaivarta Purana, Agni Purana, Bhavishya Purana, Nilamata Purana; Shri Kamakshi Vilasa Dwadasha Divya Sahasranaama: a) Devi Chaturvidha Sahasra naama: Lakshmi, Lalitha, Saraswati, Gayatri; b) Chaturvidha Shiva Sahasra naama-Linga-Shiva-Brahma Puranas and Maha Bhagavata; c) Trividha Vishnu and Yugala Radha-Krishna Sahasra naama-Padma-Skanda-Maha Bharata and Narada Purana. Stotra Kavacha- A Shield of Prayers -Purana Saaraamsha; Select Stories from Puranas Essence of Dharma Sindhu - Dharma Bindu - Shiva Sahasra Lingarchana-Essence of Paraashara Smriti Essence of Pradhana Tirtha Mahima Essence of Upanishads : Brihadaranyaka , Katha, Tittiriya, Isha, Svetashwara of Yajur Veda-Chhandogya and Kena of Saama Veda-Atreya and Kausheetaki of Rig Veda-Mundaka, Mandukya and Prashna of Atharva Veda ; Also ‗Upanishad Saaraamsa‘ (Quintessence of Upanishads) Essence of Virat Parva of Maha Bharata- Essence of Bharat Yatra Smriti Essence of Brahma Sutras Essence of Sankhya Parijnaana- Also Essence of Knowledge of Numbers Essence of Narada Charitra; Essence Neeti Chandrika-Essence of Hindu Festivals and Austerities Essence of Manu Smriti- Quintessence of Manu Smriti- Essence of Paramartha Saara; Essence of Pratyaksha Bhaskra; Essence of Maha Narayanopashid; Essence of Maitri Upanishad Essence of Vidya-Vigjnaana-Vaak Devi; Essence of Bhagya -Bhogya-Yogyata Lakshmi Essence of Soundarya Lahari*- Essence of Popular Stotras*- Essence of Pratyaksha Chandra*- Essence of Pancha Bhutas* Note: All the above Scriptures already released on www. -
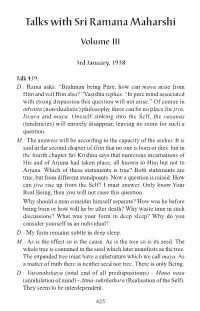
Talks with Ramana Maharshi
Talks with Sri Ramana Maharshi Volume III 3rd January, 1938 Talk 439. D.: Rama asks: “Brahman being Pure, how can maya arise from Him and veil Him also? “Vasishta replies: “In pure mind associated with strong dispassion this question will not arise.” Of course in advaita (non-dualistic) philosophy there can be no place for jiva, Isvara and maya. Oneself sinking into the Self, the vasanas (tendencies) will entirely disappear, leaving no room for such a question. M.: The answers will be according to the capacity of the seeker. It is said in the second chapter of Gita that no one is born or dies: but in the fourth chapter Sri Krishna says that numerous incarnations of His and of Arjuna had taken place, all known to Him but not to Arjuna. Which of these statements is true? Both statements are true, but from different standpoints. Now a question is raised: How can jiva rise up from the Self? I must answer. Only know Your Real Being, then you will not raise this question. Why should a man consider himself separate? How was he before being born or how will he be after death? Why waste time in such discussions? What was your form in deep sleep? Why do you consider yourself as an individual? D.: My form remains subtle in deep sleep. M.: As is the effect so is the cause. As is the tree so is its seed. The whole tree is contained in the seed which later manifests as the tree. The expanded tree must have a substratum which we call maya. -

Tattva Bodha
|| iɨuÉoÉÉåkÉÈ || TATTVA BODHA Basic Vedanta Terms & Definitions “THE SANDEEPANY EXPERIENCE” Reflections by TEXT SWAMI GURUBHAKTANANDA 02 Sandeepany’s Vedanta Course List of All the Course Texts in Chronological Sequence: Text TITLE OF TEXT Text TITLE OF TEXT No. No. 1 Sadhana Panchakam 24 Hanuman Chalisa 2 Tattwa Bodha 25 Vakya Vritti 3 Atma Bodha 26 Advaita Makaranda 4 Bhaja Govindam 27 Kaivalya Upanishad 5 Manisha Panchakam 28 Bhagavad Geeta (Discourse -- ) 6 Forgive Me 29 Mundaka Upanishad 7 Upadesha Sara 30 Amritabindu Upanishad 8 Prashna Upanishad 31 Mukunda Mala (Bhakti Text) 9 Dhanyashtakam 32 Tapovan Shatkam 10 Bodha Sara 33 The Mahavakyas, Panchadasi 5 11 Viveka Choodamani 34 Aitareya Upanishad 12 Jnana Sara 35 Narada Bhakti Sutras 13 Drig-Drishya Viveka 36 Taittiriya Upanishad 14 “Tat Twam Asi” – Chand Up 6 37 Jivan Sutrani (Tips for Happy Living) 15 Dhyana Swaroopam 38 Kena Upanishad 16 “Bhoomaiva Sukham” Chand Up 7 39 Aparoksha Anubhuti (Meditation) 17 Manah Shodhanam 40 108 Names of Pujya Gurudev 18 “Nataka Deepa” – Panchadasi 10 41 Mandukya Upanishad 19 Isavasya Upanishad 42 Dakshinamurty Ashtakam 20 Katha Upanishad 43 Shad Darshanaah 21 “Sara Sangrah” – Yoga Vasishtha 44 Brahma Sootras 22 Vedanta Sara 45 Jivanmuktananda Lahari 23 Mahabharata + Geeta Dhyanam 46 Chinmaya Pledge A NOTE ABOUT SANDEEPANY Sandeepany Sadhanalaya is an institution run by the Chinmaya Mission in Powai, Mumbai, teaching a 2-year Vedanta Course. It has a very balanced daily programme of basic Samskrit, Vedic chanting, Vedanta study, Bhagavatam, Ramacharitmanas, Bhajans, meditation, sports and fitness exercises, team-building outings, games and drama, celebration of all Hindu festivals, weekly Gayatri Havan and Guru Paduka Pooja, and Karma Yoga activities. -

Review Article
Sharada Khanal et al / Int. J. Res. Ayurveda Pharm. 9 (3), 2018 Review Article www.ijrap.net CRITICAL REVIEW OF RASA DRAVYA IN SHARANGADHARA SAMHITA Sharada Khanal 1*, Govinda Sharma K 2, Vinay R. Kadibagil 3, Ramesh Paudel 4 1PG Scholar, Department of Rasasashtra and Bhaishajya Kalpana, Sri Dharmasthala Manjunatheswara College of Ayurveda and Hospital Hassan, Karnataka, India 2Associate Professor, Department of Rasasashtra and Bhaishajya Kalpana, Sri Dharmasthala Manjunatheswara College of Ayurveda and Hospital Hassan, Karnataka, India 3HOD & Professor, Department of Rasasashtra and Bhaishajya Kalpana, Sri Dharmasthala Manjunatheswara College of Ayurveda and Hospital Hassan, Karnataka, India 4PG Scholar, Department of Shalya Tantra, Sri Dharmasthala Manjunatheswara College of Ayurveda and Hospital Hassan, Karnataka, India Received on: 25/01/18 Accepted on: 23/03/18 *Corresponding author E-mail: [email protected] DOI: 10.7897/2277-4343.09378 ABSTRACT Sharangadhara Samhita the authentic text of Ayurveda and is one among the Laghutrayee. The book is bifurcated into three Khanda (Parts) naming Prathama, Madhyama, Uttara Khanda. There are 7 chapters in Prathama khanda, 12 in Madhyama khanda and 13 in Uttara khanda. The salient features of the book are Nadi Pareksha (Pulse examination), Pharmacological terms, Principles and practice of pharmaceutics with number of Formulation. In this work an attempt has been done to review complete book to search the use of rasa dravya (Mineral drugs). The rasa dravya which were used as an ingredient, as anupana (adjuvant), used for storage purposes and also in cooking were enlisted in the present work. The book is more focused to Bhaishajya Kalpana, but the author has given importance to Rasa Dravyas also. -

Cross Cultural Psychology
ALAGAPPA UNIVERSITY [ACCREDITED WITH ‘A+’ Grade by NAAC (CGPA:3.64) in the Third Cycle and Graded as Category-I University by MHRD-UGC] (A State University Established by the Government of Tamilnadu) KARAIKUDI – 630 003 DIRECTORATE OF DISTANCE EDUCATION B.Sc., PSYCHOLOGY IV SEMESTER 11943- CROSS CULTURAL PSYCHOLOGY Copy Right Reserved For Private use only Author: Dr.S.Nasar, Assistant Professor, PG and Research Department of Commerce, Dr.Zakir Hussain College Illayangudi. “The Copyright shall be vested with Alagappa University” All rights reserved. No part of this publication which is material protected by this copyright notice may be reproduced or transmitted or utilized or stored in any form or by any means now known or hereinafter invented, electronic, digital or mechanical, including photocopying, scanning, recording or by any information storage or retrieval system, without prior written permission from the Alagappa University, Karaikudi, Tamil Nadu. SYLLABI – BOOK MAPPING TABLE 11943- CROSS CULTURAL PSYCHOLOGY Syllabi Mapping in Book BLOCK I PSYCHOLOGY AND CULTURE UNIT I Pages 1-23 Definition of culture Approaches to culture Interface between psychology and culture Pancultural principles verses culture UNIT II Pages 24-38 Specific Differences: Etics and Emics Methods of understanding culture, scope of cultural psychology. UNIT III Pages 39-58 Culture and perception – perception and experience cultural influence on visual perception Culture and Cognition culture, UNIT IV Pages 59-86 Categorization and concept formation, culture and