X-Ray Film Reading Made Easy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

5G Candidate Band Study
5G Candidate Band Study Study on the Suitability of Potential Candidate Frequency Bands above 6GHz for Future 5G Mobile Broadband Systems Final Report to Ofcom, March 2015 Contributors Steve Methley, William Webb, Stuart Walker, John Parker Quotient Associates Limited Compass House, Vision Park, Chivers Way, Histon, Cambridge, CB24 9AD, UK EMAIL [email protected] WEB www.QuotientAssociates.com Ver si on 02 Status Approved History Reviewed by Ofcom Type Public 5G Candidate Band Study | Contributors Final Report : qa1015 © Quotient Associates Ltd. 2015 Commercial in Confidence. No part of the contents of this document may be disclosed, used or reproduced in any form, or by any means, without the prior written consent of Quotient Associates Ltd. ii EXECUTIVE SUMMARY Objective and scope Within industry and academia there is significant activity in research and development towards the next generation of mobile broadband technologies (5G). Coupled with this there is increasing interest in identifying the frequency bands that will be needed to deliver 5G services. At the moment there is no overall consensus on what 5G will actually be. Work in ITU-R (WP5D) is ongoing to develop a vision for 5G (IMT 2020) including identifying the target capabilities. It is, however, widely accepted that at least one element of 5G will require the use of spectrum bands at much higher frequencies than those that current mobile broadband technologies can make use of, e.g. bands above 6 GHz. A first step currently being discussed is a proposal for an agenda item for the World Radio Conference after next (WRC-19) to identify suitable high frequency spectrum for 5G in the ITU Radio Regulations. -

X-Ray Interpretation
Objectives Describe a systematic method for interpretation of chest and abdomen x-rays List findings to accurately identify common X-ray Interpretation pathology in chest & abdomen x-rays Describe a systematic method to approach the Denise Ramponi, DNP, FNP-C, ENP-BC, FAANP, FAEN important components in interpretation of upper & lower extremity x-rays Chest X-ray: Standard Views Lateral Film Postero-anterior (PA): (LAT) view can determine th On inspiration – diaphragm descends to 10 rib the anterior-posterior posteriorly structures along the axis of the body Normal LAT film Counting Ribs AP View - Portable http://www.lumen.luc.edu/lumen/MedEd/medicine/pulmonar/cxr/cxr_f.htm When the patient is unable to tolerate routine views with pts sitting or supine No participation from the patient Film is against the patient's back (supine) 1 Consolidation, Atelectasis, Chest radiograph Interstitial involvement Consolidation - any pathologic process that fills the alveoli with Left and right heart fluid, pus, blood, cells or other borders well defined substances Interstitial - involvement of the Both hemidiaphragms supporting tissue of the lung visible to midline parenchyma resulting in fine or coarse reticular opacities Right - higher Atelectasis - collapse of a part of Heart less than 50% of the lung due to a decrease in the amount of air resulting in volume diameter of the chest loss and increased density. Infiltrate, Consolidation vs. Congestive Heart Failure Atelectasis Fluid leaking into interstitium Kerley B 2 Kerley B lines Prominent interstitial markings Kerley lines Magnified CXR Cardiomyopathy & interstitial pulmonary edema Short 1-2 cm white lines at lung periphery horizontal to pleural surface Distended interlobular septa - secondary to interstitial edema. -
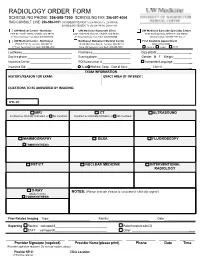
Radiology Order Form
RADIOLOGY ORDER FORM SCHEDULING PHONE: 206-598-7200 SCHEDULING FAX: 206-597-4004 RAD CONSULT LINE: 206-598-0101 UW RADIOLOGY RECORDS: Tel: 206-598-6206 Fax: 206-598-7690 NW RADIOLOGY RECORDS: Tel: 206-668-1748 Fax: 206-688-1398 UW Medical Center - Montlake UW Medicine Roosevelt Clinic UW Medicine Eastside Specialty Center 1959 NE Pacific Street, Seattle, WA 98195 4245 Roosevelt Way NE, Seattle, WA 98105 3100 Northup Way, Bellevue, WA 98004 2nd Floor Radiology Front Desk: 206-598-6200 2nd Floor Radiology Front Desk: 206-598-6868 ESC Front Desk: 425-646-7777 Opt. 2 UW Medical Center - Northwest Northwest Outpatient Medical Center First Available Appointment 1550 N 115th St, Seattle, WA 98133 10330 Meridian Ave N, Seattle, WA 98133 (ANY LOCATION) 2nd Floor Radiology Front Desk: 206-668-1302 Suite 130 Radiology Front Desk: 206-668-6050 Routine Urgent STAT Last Name: First Name: Date of Birth: _ Daytime phone: Evening phone: Gender: M F Weight:___________ Insurance Carrier: RQI/Authorization #: Interpreter/Language: __ Insurance ID#: Auto Workers’ Comp Date of Injury: ______ Claim # __ EXAM INFORMATION HISTORY/REASON FOR EXAM: EXACT AREA OF INTEREST: EXAM INFORMATION QUESTIONS TO BE ANSWERED BY IMAGING: ICD-10: MRI CT ULTRASOUND Contrast as clinically indicated, or No Contrast Contrast as clinically indicated, or No Contrast MAMMOGRAPHY DEXA FLUOROSCOPY TOMOSYNTHESIS PET/CT NUCLEAR MEDICINE INTERVENTIONAL RADIOLOGY X-RAY NOTES: (Please indicate if exam is considered “clinically urgent”) (Walk-In Only) TOMOSYNTHESIS Prior Related Imaging Type:_________________________ Facility:_________________________ Date:___________________ Reporting Routine call report # Patient to return with CD STAT call report # Other: __________ ________________________ ______________________ ____________ _______ ______ Provider Signature (required) Provider Name (please print) Phone Date Time (Provider signature required. -

RADIOGRAPHY to Prepare Individuals to Become Registered Radiologic Technologists
RADIOGRAPHY To prepare individuals to become Registered Radiologic Technologists. THE WORKFORCE CAPITAL This two-year, advanced medical program trains students in radiography. Radiography uses radiation to produce images of tissues, organs, bones and vessels of the body. The radiographer is an essential member of the health care team who works in a variety of settings. Responsibili- ties include accurately positioning the patient, producing quality diagnostic images, maintaining equipment and keeping computerized records. This certificate program of specialized training focuses on each of these responsibilities. Graduates are eligible to apply for the national credential examination to become a registered technologist in radiography, RT(R). Contact Student Services for current tuition rates and enrollment information. 580.242.2750 Mission, Goals, and Student Learning Outcomes Program Effectiveness Data Radiography Program Guidelines (Policies and Procedures) “The programs at Autry prepare you for the workforce with no extra training needed after graduation.” – Kenedy S. autrytech.edu ENDLESS POSSIBILITIES 1201 West Willow | Enid, Oklahoma, 73703 | 580.242.2750 | autrytech.edu COURSE LENGTH Twenty-four-month daytime program î August-July î Monday-Friday Academic hours: 8:15am-3:45pm Clinical hours: Eight-hour shifts between 7am-5pm with some ADMISSION PROCEDURES evening assignments required Applicants should contact Student Services at Autry Technology Center to request an information/application packet. Applicants who have a completed application on file and who have met entrance requirements will be considered for the program. Meeting ADULT IN-DISTRICT COSTS the requirements does not guarantee admission to the program. Qualified applicants will be contacted for an interview, and class Year One: $2732 (Additional cost of books and supplies approx: $1820) selection will be determined by the admissions committee. -

Chest and Abdominal Radiograph 101
Chest and Abdominal Radiograph 101 Ketsia Pierre MD, MSCI July 16, 2010 Objectives • Chest radiograph – Approach to interpreting chest films – Lines/tubes – Pneumothorax/pneumomediastinum/pneumopericar dium – Pleural effusion – Pulmonary edema • Abdominal radiograph – Tubes – Bowel gas pattern • Ileus • Bowel obstruction – Pneumoperitoneum First things first • Turn off stray lights, optimize room lighting • Patient Data – Correct patient – Patient history – Look at old films • Routine Technique: AP/PA, exposure, rotation, supine or erect Approach to Reading a Chest Film • Identify tubes and lines • Airway: trachea midline or deviated, caliber change, bronchial cut off • Cardiac silhouette: Normal/enlarged • Mediastinum • Lungs: volumes, abnormal opacity or lucency • Pulmonary vessels • Hila: masses, lymphadenopathy • Pleura: effusion, thickening, calcification • Bones/soft tissues (four corners) Anatomy of a PA Chest Film TUBES Endotracheal Tubes Ideal location for ETT Is 5 +/‐ 2 cm from carina ‐Normal ETT excursion with flexion and extension of neck 2 cm. ETT at carina Right mainstem Intubation ‐Right mainstem intubation with left basilar atelectasis. ETT too high Other tubes to consider DHT down right mainstem DHT down left mainstem NGT with tip at GE junction CENTRAL LINES Central Venous Line Ideal location for tip of central venous line is within superior vena cava. ‐ Risk of thrombosis decreased in central veins. ‐ Catheter position within atrium increases risk of perforation Acceptable central line positions • Zone A –distal SVC/superior atriocaval junction. • Zone B – proximal SVC • Zone C –left brachiocephalic vein. Right subclavian central venous catheter directed cephalad into IJ Where is this tip? Hemiazygous Or this one? Right vertebral artery Pulmonary Arterial Catheter Ideal location for tip of PA catheter within mediastinal shadow. -

ACR–SPR-STR Practice Parameter for the Performance of Chest Radiography
The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists, and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice parameters and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice parameters and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice parameter and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review and approval. The practice parameters and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice parameter and technical standard by those entities not providing these services is not authorized. Revised 2017 (Resolution 2)* ACR–SPR–STR PRACTICE PARAMETER FOR THE PERFORMANCE OF CHEST RADIOGRAPHY PREAMBLE This document is an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care1. -
Cardiothoracic Fellowship Program
Cardiothoracic Fellowship Program Table of Contents Program Contact ............................................................................................ 3 Other contact numbers .................................................................................. 4 Introduction ........................................................................................................... 5 Goals and Objectives of Fellowship: ..................................................................... 6 Rotation Schedule: ........................................................................................ 7 Core Curriculum .................................................................................................... 8 Fellow’s Responsibilities ..................................................................................... 22 Resources ........................................................................................................... 23 Facilities ....................................................................................................... 23 Educational Program .......................................................................................... 26 Duty Hours .......................................................................................................... 29 Evaluation ........................................................................................................... 30 Table of Appendices .................................................................................... 31 Appendix A -

Pediatrics-EOR-Outline.Pdf
DERMATOLOGY – 15% Acne Vulgaris Inflammatory skin condition assoc. with papules & pustules involving pilosebaceous units Pathophysiology: • 4 main factors – follicular hyperkeratinization with plugging of sebaceous ducts, increased sebum production, Propionibacterium acnes overgrowth within follicles, & inflammatory response • Hormonal activation of pilosebaceous glands which may cause cyclic flares that coincide with menstruation Clinical Manifestations: • In areas with increased sebaceous glands (face, back, chest, upper arms) • Stage I: Comedones: small, inflammatory bumps from clogged pores - Open comedones (blackheads): incomplete blockage - Closed comedones (whiteheads): complete blockage • Stage II: Inflammatory: papules or pustules surrounded by inflammation • Stage III: Nodular or cystic acne: heals with scarring Differential Diagnosis: • Differentiate from rosacea which has no comedones** • Perioral dermatitis based on perioral and periorbital location • CS-induced acne lacks comedones and pustules are in same stage of development Diagnosis: • Mild: comedones, small amounts of papules &/or pustules • Moderate: comedones, larger amounts of papules &/or pustules • Severe: nodular (>5mm) or cystic Management: • Mild: topical – azelaic acid, salicylic acid, benzoyl peroxide, retinoids, Tretinoin topical (Retin A) or topical antibiotics [Clindamycin or Erythromycin with Benzoyl peroxide] • Moderate: above + oral antibiotics [Minocycline 50mg PO qd or Doxycycline 100 mg PO qd], spironolactone • Severe (refractory nodular acne): oral -
Design of SWB Antenna with Triple Band Notch Characteristics for Multipurpose Wireless Applications
applied sciences Article Design of SWB Antenna with Triple Band Notch Characteristics for Multipurpose Wireless Applications Warsha Balani 1, Mrinal Sarvagya 1, Tanweer Ali 2,* , Ajit Samasgikar 3, Saumya Das 4, Pradeep Kumar 5,* and Jaume Anguera 6,7 1 School of Electronics and Communication Engineering, Reva University, Bangalore 560064, India; [email protected] (W.B.); [email protected] (M.S.) 2 Department of Electronics and Communication, Manipal Institute of Technology, Manipal Academy of Higher Education, Manipal, Karnataka 576104, India 3 MMRFIC Technology Pvt Ltd., Bangalore 560016, India; [email protected] 4 Department of Information Technology, Sikkim Manipal Institute of Technology, Sikkim Manipal University, Sikkim 737102, India; [email protected] 5 Discipline of Electrical, Electronic and Computer Engineering, University of KwaZulu-Natal, Durban 4041, South Africa 6 Fractus Antennas, 08174 Barcelona, Spain; [email protected] 7 Electronics and Telecommunication Department, Universitat Ramon LLull, 08022 Barcelona, Spain * Correspondence: [email protected] (T.A.); [email protected] (P.K.) Abstract: A compact concentric structured monopole antenna for super wide band (SWB) applica- tions with triple notch band characteristics is designed and experimentally validated. The antenna covers an immense impedance bandwidth (1.6–47.5 GHz) with sharp triple notch bands at 1.8– 2.2 GHz, 4–7.2 GHz, and 9.8–10.4 GHz to eliminate interference from co-existing advanced wireless services (AWS), C bands, and X bands, respectively. By loading an E-shaped stub connected at the top of the patch and by etching a split elliptical slot at the lower end of the radiating patch, the band rejection characteristics from 1.8–2.2 GHz for the AWS and 4–7.2 GHz for the C band are achieved, Citation: Balani, W.; Sarvagya, M.; respectively. -

Imaging: Results and Hospital Course: • Patient Initially Presented to RMH on 8/20/2019
Introduction / HPI: Imaging: Results and Hospital Course: • Patient initially presented to RMH on 8/20/2019. He was treated for RLE 27 yo male with past medical history of IVDA presented to cellulitis with a washout; as well as, IV Cefazolin for MSSA + Blood Roxborough Memorial Hospital (RMH) with right leg swelling for 5 cultures. Blood cultures remained positive x4; spurring a TTE, which was days and shortness of breath. The patient stated that 5 days prior he negative for vegetations. CXR preformed demonstrated concern for septic was using heroin and injecting the needle into his right medial foot. He embolic, spurring a Chest CT with reported finding of said that the following day he noticed a blister forming and sliced it hydropneumothorax. Patient was transferred to TJUH on 8/28 for the with a knife that he cleaned with soap and water. The next day he possibility of needing cardiothoracic surgery capabilities. noticed swelling of his foot with progressing redness and pain traveling up his leg to his knee. He described the pain as a 5 out of 10 when at • He was admitted to the TJUH SICU. Subsequently the patient had rest and a 7 out of 10 when walking on it. He stated that he has been multiple episodes of bloody BM’s and his Hgb dropped to 6.9. He taking 1 tablet of Motrin per day for last 3 days with minimal received 2 units pRBC’s with appropriate hemodynamic response. GI was relief. He endorsed shortness of breath when at rest and exertion, chest consulted, whom preformed an EGD and colonoscopy on 9/9. -

Clinical Acute Abdominal Pain in Children
Clinical Acute Abdominal Pain in Children Urgent message: This article will guide you through the differential diagnosis, management and disposition of pediatric patients present- ing with acute abdominal pain. KAYLEENE E. PAGÁN CORREA, MD, FAAP Introduction y tummy hurts.” That is a simple statement that shows a common complaint from children who seek “M 1 care in an urgent care or emergency department. But the diagnosis in such patients can be challenging for a clinician because of the diverse etiologies. Acute abdominal pain is commonly caused by self-limiting con- ditions but also may herald serious medical or surgical emergencies, such as appendicitis. Making a timely diag- nosis is important to reduce the rate of complications but it can be challenging, particularly in infants and young children. Excellent history-taking skills accompanied by a careful, thorough physical exam are key to making the diagnosis or at least making a reasonable conclusion about a patient’s care.2 This article discusses the differential diagnosis for acute abdominal pain in children and offers guidance for initial evaluation and management of pediatric patients presenting with this complaint. © Getty Images Contrary to visceral pain, somatoparietal pain is well Pathophysiology localized, intense (sharp), and associated with one side Abdominal pain localization is confounded by the or the other because the nerves associated are numerous, nature of the pain receptors involved and may be clas- myelinated and transmit to a specific dorsal root ganglia. sified as visceral, somatoparietal, or referred pain. Vis- Somatoparietal pain receptors are principally located in ceral pain is not well localized because the afferent the parietal peritoneum, muscle and skin and usually nerves have fewer endings in the gut, are not myeli- respond to stretching, tearing or inflammation. -

Listen to the Associated Podcast Episodes: MSK: Fractures for the ABR Core Exam Parts 1-3, Available at Theradiologyreview.Com O
MSK: Fractures for Radiology Board Study, Matt Covington, MD Listen to the associated podcast episodes: MSK: Fractures for the ABR Core Exam Parts 1-3, available Listen to associated Podcast episodes: ABR Core Exam, Multisystemic Diseases Parts 1-3, available at at theradiologyreview.com or on your favorite podcast directory. Copyrighted. theradiologyreview.com or on your favorite podcast direcry. Fracture resulting From abnormal stress on normal bone = stress Fracture Fracture From normal stress on abnormal bone = insuFFiciency Fracture Scaphoid Fracture site with highest risk for avascular necrosis (proximal or distal)? Proximal pole scaphoid Fractures are at highest risk For AVN Comminuted Fracture at the base oF the First metacarpal = Rolando Fracture Non-comminuted Fracture at base oF the First metacarpal = Bennett Fracture The pull oF which tendon causes the dorsolateral dislocation in a Bennett fracture? The abductor pollicus longus tendon. Avulsion Fracture at the base oF the proximal phalanx with ulnar collateral ligament disruption = Gamekeeper’s thumb. Same Fracture but adductor tendon becomes caught in torn edge oF the ulnar collateral ligament? Stener’s lesion. IF Stener’s lesion is present this won’t heal on its own so you need surgery. You shouldn’t image a Gamekeeper’s thumb with stress views because you can convert it to a Stener’s lesion. Image with MRI instead. Distal radial Fracture with dorsal angulation = Colle’s Fracture (C to D= Colle’s is Dorsal) Distal radial Fracture with volar angulation = Smith’s Fracture (S