Original Article
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sustainability of Rural Socio-Economic
African Journal of Politics and Administrative Studies, Vol. 9, 1; March, 2016 Department of Political Science, Ebonyi State University, Abakaliki SUSTAINABILITY OF RURAL SOCIO-ECONOMIC DEVELOPMENT PROGRAMMES AND POVERTY REDUCTION IN NIGERIA: A STUDY OF EBONYI STATE COMMUNITY AND SOCIAL DEVELOPMENT AGENCY (EB-CSDA) IN IZZI CLAN. Nwankwo, Oliver U. 1; Nwuzor, Chidi Iroko 2; David M.E. Nwogbaga, Ph.D 3; Doris O. Onwa 4 1,3,&4 Department of Political Science 2 Department of Public Administrations Ebonyi State University, Abakaliki E-mail: [email protected];[email protected] Abstract The dynamic, complex and multi-dimensional nature of poverty makes it one of the most current problems that are negatively affecting the globe. This study investigated the high level socio-economic poverty ravaging Izzi clan of Ebonyi State Nigeria. Specifically, the study sort to find out why there is high incidence of poverty in Izzi despite government and individual efforts over the years. The study adopted the Progressive Utilization Theory (PROUT) by PrahatRanjan Sarkar in 1959, and the Socio-Political and Economic Theory as propounded by Adam Smith in 1776 as its frameworks of analysis. Some randomly selected Izzi people, particularly from the villages were interviewed to elicit relevant information and data for the study. We discovered that over reliance on persistent farming, lack of helping hands from the haves, lack of family planning and non-exposure to early formal education, were among the major causes of unending poverty amongIzzi people. The study therefore recommended for the enabling legislation to check the ever-increasing population without a corresponding means of livelihood, aggressive rural electrification and provision of portable water, provision of micro-credit loan scheme to the rural poor and proper sensitization of the rural communities on the activities EB-CSDA. -

Nigeria's Constitution of 1999
PDF generated: 26 Aug 2021, 16:42 constituteproject.org Nigeria's Constitution of 1999 This complete constitution has been generated from excerpts of texts from the repository of the Comparative Constitutions Project, and distributed on constituteproject.org. constituteproject.org PDF generated: 26 Aug 2021, 16:42 Table of contents Preamble . 5 Chapter I: General Provisions . 5 Part I: Federal Republic of Nigeria . 5 Part II: Powers of the Federal Republic of Nigeria . 6 Chapter II: Fundamental Objectives and Directive Principles of State Policy . 13 Chapter III: Citizenship . 17 Chapter IV: Fundamental Rights . 20 Chapter V: The Legislature . 28 Part I: National Assembly . 28 A. Composition and Staff of National Assembly . 28 B. Procedure for Summoning and Dissolution of National Assembly . 29 C. Qualifications for Membership of National Assembly and Right of Attendance . 32 D. Elections to National Assembly . 35 E. Powers and Control over Public Funds . 36 Part II: House of Assembly of a State . 40 A. Composition and Staff of House of Assembly . 40 B. Procedure for Summoning and Dissolution of House of Assembly . 41 C. Qualification for Membership of House of Assembly and Right of Attendance . 43 D. Elections to a House of Assembly . 45 E. Powers and Control over Public Funds . 47 Chapter VI: The Executive . 50 Part I: Federal Executive . 50 A. The President of the Federation . 50 B. Establishment of Certain Federal Executive Bodies . 58 C. Public Revenue . 61 D. The Public Service of the Federation . 63 Part II: State Executive . 65 A. Governor of a State . 65 B. Establishment of Certain State Executive Bodies . -
Nigeria Conflict Re-Interview (Emergency Response
This PDF generated by kmcgee, 8/18/2017 11:01:05 AM Sections: 11, Sub-sections: 0, Questionnaire created by akuffoamankwah, 8/2/2017 7:42:50 PM Questions: 130. Last modified by kmcgee, 8/18/2017 3:00:07 PM Questions with enabling conditions: 81 Questions with validation conditions: 14 Shared with: Rosters: 3 asharma (never edited) Variables: 0 asharma (never edited) menaalf (never edited) favour (never edited) l2nguyen (last edited 8/9/2017 8:12:28 PM) heidikaila (never edited) Nigeria Conflict Re- interview (Emergency Response Qx) [A] COVER No sub-sections, No rosters, Questions: 18, Static texts: 1. [1] DISPLACEMENT No sub-sections, No rosters, Questions: 6. [2] HOUSEHOLD ROSTER - BASIC INFORMATION No sub-sections, Rosters: 1, Questions: 14, Static texts: 1. [3] EDUCATION No sub-sections, Rosters: 1, Questions: 3. [4] MAIN INCOME SOURCE FOR HOUSEHOLD No sub-sections, No rosters, Questions: 14, Static texts: 1. [5] MAIN EMPLOYMENT OF HOUSEHOLD No sub-sections, No rosters, Questions: 6, Static texts: 1. [6] ASSETS No sub-sections, Rosters: 1, Questions: 12, Static texts: 1. [7] FOOD AND MARKET ACCESS No sub-sections, No rosters, Questions: 21. [8] VULNERABILITY MEASURE: COPING STRATEGIES INDEX No sub-sections, No rosters, Questions: 6. [9] WATER ACCESS AND QUALITY No sub-sections, No rosters, Questions: 22. [10] INTERVIEW RESULT No sub-sections, No rosters, Questions: 8, Static texts: 1. APPENDIX A — VALIDATION CONDITIONS AND MESSAGES APPENDIX B — OPTIONS LEGEND 1 / 24 [A] COVER Household ID (hhid) NUMERIC: INTEGER hhid SCOPE: IDENTIFYING -
“Burn the Mmonwu” Contradictions and Contestations in Masquerade Perfor- Mance in Uga, Anambra State in Southeastern Nigeria
“Burn the Mmonwu” Contradictions and Contestations in Masquerade Perfor- mance in Uga, Anambra State in Southeastern Nigeria Charles Gore asked performances organized by male asso- ciations are a distinctive feature of public per- ALL PHOTOS BY THE AUTHOR formance among Igbo-speaking peoples of southeastern Nigeria (Jones 1984, Cole and Ania- kor 1984) and have been the subject of attention by African art historians in the twentieth cen- tury (Ottenberg 1975, Aniakor 1978, Ugonna 1984, Henderson and MUmunna 1988, Bentor 1995). Innovation and change in terms of iconography, ritual, and dramatic presentation have always been important components to these performances, as well as flexible adaptations and responses to changing social circumstances (Figs. 1–3). However, in the last two decades, new mass movements of Christian evangelism and Pentecostalism have emerged, success- fully exhorting their members to reject masquerade as a pagan practice. During this time, in many places in southeastern Nige- ria, famous and long-standing masquerade associations have dis- banded and their masks and costumes burnt as testimonies to the efficacy of Pentecostalism, affirming the successful conversion of former masquerade members. This research examines the chal- lenges that changing localized circumstances pose to masquerade practice in one locale in southeastern Nigeria. Uga1 is located in southeastern Nigeria in Aguata Local Gov- ernment Area (LGA) in Anambra state, along the Nnewi-Okigwe expressway in Nigeria, some 40 km (25 mi.) eastwards from Onitsha on the river Niger (Fig. 4). It consisted until recently of four village units—Umueze, Awarasi, Umuoru, and Oka—spa- tially contiguous with each other and has a population of some 20,000 individuals. -

The Land Has Changed: History, Society and Gender in Colonial Eastern Nigeria
University of Calgary PRISM: University of Calgary's Digital Repository University of Calgary Press University of Calgary Press Open Access Books 2010 The land has changed: history, society and gender in colonial Eastern Nigeria Korieh, Chima J. University of Calgary Press Chima J. Korieh. "The land has changed: history, society and gender in colonial Eastern Nigeria". Series: Africa, missing voices series 6, University of Calgary Press, Calgary, Alberta, 2010. http://hdl.handle.net/1880/48254 book http://creativecommons.org/licenses/by-nc-nd/3.0/ Attribution Non-Commercial No Derivatives 3.0 Unported Downloaded from PRISM: https://prism.ucalgary.ca University of Calgary Press www.uofcpress.com THE LAND HAS CHANGED History, Society and Gender in Colonial Eastern Nigeria Chima J. Korieh ISBN 978-1-55238-545-6 THIS BOOK IS AN OPEN ACCESS E-BOOK. It is an electronic version of a book that can be purchased in physical form through any bookseller or on-line retailer, or from our distributors. Please support this open access publication by requesting that your university purchase a print copy of this book, or by purchasing a copy yourself. If you have any questions, please contact us at [email protected] Cover Art: The artwork on the cover of this book is not open access and falls under traditional copyright provisions; it cannot be reproduced in any way without written permission of the artists and their agents. The cover can be displayed as a complete cover image for the purposes of publicizing this work, but the artwork cannot be extracted from the context of the cover of this specific work without breaching the artist’s copyright. -
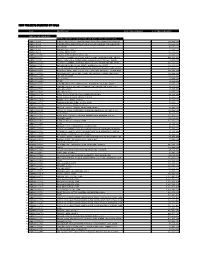
New Projects Inserted by Nass
NEW PROJECTS INSERTED BY NASS CODE MDA/PROJECT 2018 Proposed Budget 2018 Approved Budget FEDERAL MINISTRY OF AGRICULTURE AND RURAL SUPPLYFEDERAL AND MINISTRY INSTALLATION OF AGRICULTURE OF LIGHT AND UP COMMUNITYRURAL DEVELOPMENT (ALL-IN- ONE) HQTRS SOLAR 1 ERGP4145301 STREET LIGHTS WITH LITHIUM BATTERY 3000/5000 LUMENS WITH PIR FOR 0 100,000,000 2 ERGP4145302 PROVISIONCONSTRUCTION OF SOLAR AND INSTALLATION POWERED BOREHOLES OF SOLAR IN BORHEOLEOYO EAST HOSPITALFOR KOGI STATEROAD, 0 100,000,000 3 ERGP4145303 OYOCONSTRUCTION STATE OF 1.3KM ROAD, TOYIN SURVEYO B/SHOP, GBONGUDU, AKOBO 0 50,000,000 4 ERGP4145304 IBADAN,CONSTRUCTION OYO STATE OF BAGUDU WAZIRI ROAD (1.5KM) AND EFU MADAMI ROAD 0 50,000,000 5 ERGP4145305 CONSTRUCTION(1.7KM), NIGER STATEAND PROVISION OF BOREHOLES IN IDEATO NORTH/SOUTH 0 100,000,000 6 ERGP445000690 SUPPLYFEDERAL AND CONSTITUENCY, INSTALLATION IMO OF STATE SOLAR STREET LIGHTS IN NNEWI SOUTH LGA 0 30,000,000 7 ERGP445000691 TOPROVISION THE FOLLOWING OF SOLAR LOCATIONS: STREET LIGHTS ODIKPI IN GARKUWARI,(100M), AMAKOM SABON (100M), GARIN OKOFIAKANURI 0 400,000,000 8 ERGP21500101 SUPPLYNGURU, YOBEAND INSTALLATION STATE (UNDER OF RURAL SOLAR ACCESS STREET MOBILITY LIGHTS INPROJECT NNEWI (RAMP)SOUTH LGA 0 30,000,000 9 ERGP445000692 TOSUPPLY THE FOLLOWINGAND INSTALLATION LOCATIONS: OF SOLAR AKABO STREET (100M), LIGHTS UHUEBE IN AKOWAVILLAGE, (100M) UTUH 0 500,000,000 10 ERGP445000693 ANDEROSION ARONDIZUOGU CONTROL IN(100M), AMOSO IDEATO - NCHARA NORTH ROAD, LGA, ETITI IMO EDDA, STATE AKIPO SOUTH LGA 0 200,000,000 11 ERGP445000694 -

Gov'ship Polls: INEC, Security Agents Identify Flash Points in Bayelsa, Kogi
SATURDAY No. 717 N300 FOR GOD AND COUNTRY 02.11.19 www.leadership.ng NIGERIA'S MOST INFLUENTIAL NEWSPAPER Leadership Newspapers @leadershipNGA MY SECRET LIFE: EFCC GOES AFTER DOCTORS FG TO ESTABLISH LG➔ ` PAGE 10 I GO EXTRA MILE FOR CLIENTS ISSUING FAKE MEDICAL FARM SETTLEMENTS – LABESA ` PAGE 71 REPORTS TO SUSPECTS` PAGE 12 NATIONWIDE – MINISTER Gov’ship Polls: INEC, Security Agents Identify Flash Points In Bayelsa, Kogi BY SUNDAY ISUWA, Abuja Police to deploy 66,214 officers flashpoints posed to the polls. He said that 66, 214 policemen Ahead of the November 16 identified major flashpoints in Kogi INEC and the security agencies agency for election security, who is would be deployed in Kogi and governorship election, the and Bayelsa States. to swing into action in order to also the inspector-general of police Bayelsa States to man all the polling Independent National Electoral LEADERSHIP Weekend recalls stem the menace in the upcoming (IGP), Mohammed Adamu, said units, INEC offices, the Central Bank Commission (INEC) and the that the two states have a history of gubernatorial election. that the security agencies were country’s security agencies have election violence which prompted To this end, the head of the lead not unmindful of the threat the ` CONTINUED ON PAGE 5 INSURGENCY Army Begins Trial Of 20 Officers, 4 Soldiers For Cowardice, Negligence Flags off ‘Operation Ayem Akpatuma 2’ in Benue, Kogi Emefiele Proposes 2-yr Border Closure Says it will solve Nigeria’s security problems BY JONATHAN NDA-ISAIAH, Abuja Emefiele Proposes Border Closure For 2 Years The governor of the Central Bank of Nigeria (CBN), Mr Godwin Emefiele, has said that if the current closure of Nigerian borders is sustained for the next two years, insurgency, banditry and kidnapping would be eradicated. -

Inventory of Nigeria Cultural Resources M
Co lu Column2 Inventory of Nigeria Cultural Resources m 1 Oral Traditions and Expressions including Languages as a Vehicle for the transmission STATE \ N0 LOCATION NAME SEX AGE CRAFT Dexterous application of proverbs in speech (proverbs are near extinction 1 Akwa Ibom Sunday Okon William M 52 in the State) Always goes about on bare feet, 2 Rivers Elder Bliss Iyalla M 70s versed in local Kalabari dialect 3 Rivers Chief Beresiri M Versed in Oral Tradition. 4 Rivers Elechi Amadi M Renouned Writer 5 Rivers Madam Adaobi Whyte F Renouned Writer Produced Several Albums in Kalabari language thereby projecting the traditions and cultural imagery of the 6 Rivers Mary Girls Social Club of Abonema F people. Used Songs to record the traditions of 7 Rivers First Owuama Ogbo of Okrika M the people Oral historian. Informs on past events , relationship of some of Nigerians tribes, well versed in past heroes like Kanta of Kabi, Sheikh Usman Danfodio, Origin of Sokoto, Argungu, Katsina, etc., and the wars fought, origin , relationship of tribes e.g. Hausas, Fulani, Yoruba, Zabarma etc. 8 Kebbi State Alh. Adamu Wakili Augie M 70s Also trains others 9 Niger Delta Gabriel Okara M Traditional Poet Has preserved Yoruba Cultural 10 Oyo Akinwumi Isola M Heritage through lingual Arts 11 Plateau Dan Maraya Jos M Traditional and dramatic Hausa Poet Light drumming for talking and praising people.Also court music for 12 Katsina Sarki Taushi Katsina M spreading news A reed flute for playing traditional music and praising traditional rulers 13 Bornu Algaita etc. Inmole Folklore singer and drummer; Kogi ( Ogidi an exponent and trainer of Inmole 14 Ojumu) Mrs Jogole Balaogun F 80s customs and rites Igbo linguist, Safgeguards the Igbo language, folklore and culture through educating students and children alike, publishing and translating in the Igbo 15 Imo Prof. -

2013 Federal Capital Budget Pull for South East
2013 FEDERAL CAPITAL BUDGET Of the States in the SOUTH EAST Geo-Political Zone Citizens Wealth Platform (CWP) (Public Resources Are Made To Work And Be Of Benefit To All) 2013 FEDERAL CAPITAL BUDGET of the States in the South East Geo-Political Zone Citizens Wealth Platform (CWP) (Public Resources Are Made To Work And Be Of Benefit To All) ii 2013 FEDERAL CAPITAL BUDGET of the States in the South East Geo-Political Zone Compiled by ……………………… For Citizens Wealth Platform (CWP) (Public Resources Are Made To Work And Be Of Benefit To All) iii First Published in September 2013 By Citizens Wealth Platform C/o Centre for Social Justice 17 Yaounde Street, Wuse Zone 6, Abuja Email: [email protected] iv Table of Contents Acknowledgment vi Foreword vii Abia State 1 Anambra State 16 Ebonyi State 25 Enugu State 29 Imo State 42 v Acknowledgment Citizens Wealth Platform acknowledges the financial and secretariat support of Centre for Social Justice towards the publication of this Capital Budget Pull-Out. vi Foreword This is the second year of the publication of Capital Budget Pull-outs for the six geo-political zones. Citizens Wealth Platform (CWP) is setting the agenda of public participation in fiscal governance especially in monitoring and tracking capital budget implementation. Popular and targeted participation is essential to hold government accountable to the promises made in the annual budget particularly the aspects of the budget that touch on the lives of the common people. In 2013, the Federal Government of Nigeria (FGN) promised to build roads, bridges, hospitals, renovate airports and generally take actions to improve living standards. -

The Fourth Republic, the Orgy of Violence and the Plight of Internally Displaced Persons in Nigeria, 1999-2009
Journal of Internal Displacement Volume 2 Number 1 © JID 2012; all rights reserved THE FOURTH REPUBLIC, THE ORGY OF VIOLENCE AND THE PLIGHT OF INTERNALLY DISPLACED PERSONS IN NIGERIA, 1999-2009 Jimoh Adele Bamgbose Abstract The twenty-ninth day of May 1999, marked the beginning of a more enduring democratic transition in the annals of democratic transitions in Nigeria. The earlier two democratic experiments of between 1960 and 1966, and between 1979 and 1983 suffered a political shipwreck as the military swept the two republics into oblivion. The Third Republic was stifled at the incubation stage, as it was not allowed to see the light of the day. This paper however examines the Nigeria’s Fourth Republic and argues that even though, it stands as a democracy with the longest life span in Nigeria, its attendant crises made it the worst type the country has ever experienced since the First Republic as thousands of people met their untimely death while scores of people were internally displaced with little or no government attention. Keywords: Nigeria, violence, ethnicity, democracy, internally displaced persons Email Alerts/Reprints/Permission: [email protected] Subscription: JID is a Free Open Access Journal Archives: http://journalinternaldisplacement.webs.com/archives.htm Submission (January 2012 Edition): http://journalinternaldisplacement.webs.com/announcements.htm JID is produced and published by EV Research Inc. – www.evresearch.ca Author’s Affiliation Jimoh Adele Bamgbose, Ph.D was formerly a programme officer in Diploma in Refugee Studies at Lagos State University. He is now a senior lecturer in the Department of Political Science at Lagos State University in Ojo, Nigeria THE FOURTH REPUBLIC, THE ORGY OF VIOLENCE AND THE PLIGHT OF INTERNALLY DISPLACED PERSONS IN NIGERIA, 1999-2009 Jimoh Adele Bamgbose Introduction Political revolution, which has taken diverse forms of transitions from authoritarianism to democracy, has become a common phenomenon the world over. -

National Assembly 260 2013 Appropriation
FEDERAL GOVERNMENT OF NIGERIA 2013 BUDGET SUMMARY FEDERAL MINISTRY OF WATER RESOURCES TOTAL TOTAL PERSONNEL TOTAL CODE MDA OVERHEAD TOTAL RECURRENT TOTAL CAPITAL COST ALLOCATION COST =N= =N= =N= =N= =N= FEDERAL MINISTRY OF WATER RESOURCES - 0252001001 1,062,802,556 434,615,687 1,497,418,243 28,714,910,815 30,212,329,058 HQTRS 0252037001 ANAMBRA/ IMO RBDA 455,494,870 69,652,538 525,147,408 7,223,377,629 7,748,525,037 252038001 BENIN/ OWENA RBDA 310,381,573 48,517,004 358,898,577 2,148,547,575 2,507,446,152 0252039001 CHAD BASIN RBDA 349,481,944 66,930,198 416,412,142 2,090,796,556 2,507,208,698 0252040001 CROSS RIVER RBDA 336,692,834 69,271,822 405,964,656 5,949,000,000 6,354,964,656 0252051001 GURARA WATER MANAGEMENT AUTHORITY 17,112,226 70,346,852 87,459,078 167,000,000 254,459,078 0252041001 HADEJIA-JAMAļARE RBDA 384,683,182 53,037,247 437,720,429 5,322,607,552 5,760,327,981 0252042001 LOWER BENUE RBDA 305,996,666 49,183,926 355,180,592 4,684,200,000 5,039,380,592 0252043001 LOWER NIGER RBDA 510,037,910 66,419,289 576,457,199 5,452,950,000 6,029,407,199 0252044001 NIGER DELTA RBDA 509,334,321 77,714,503 587,048,824 4,382,640,000 4,969,688,824 NIGERIA INTEGRATED WATER MANAGEMENT 0252050001 143,297,122 89,122,355 232,419,477 154,000,000 386,419,477 COMMISSION NATIONAL WATER RESOURCES INSTITUTE- 0252049001 266,646,342 40,532,007 307,178,349 403,000,000 710,178,349 KADUNA 0252045001 OGUN/ OSUN RBDA 387,437,686 79,556,978 466,994,664 3,500,153,045 3,967,147,709 0252046001 SOKOTO RIMA RBDA 431,782,730 83,609,292 515,392,022 6,827,983,001 7,343,375,023 -

O Rigin Al a Rticle
International Journal of History and Research (IJHR) ISSN(P): 2249–6963; ISSN(E): 2249–8079 Vol. 10 Issue 2, Dec 2020, 1–12 ©TJPRC Pvt. Ltd AFIKPO-ABAKALIKI RELATIONS: TRACING THE ROOTS DR. FRANCIS C. ODEKE & DR. IKECHUKWU O. ONUOHA Department of History and International Relations, Faculty of Social Sciences and Humanities, Ebonyi State University, Abakaliki ABSTRACT There has been a serious controversy over the origin of Afikpo and Abakaliki people of Ebonyi State, Nigeria. The argument borders on whether the two groups had shared a common origin before they parted ways as a result of wars and other factors in their early histories. This paper is a comparative study of the two cultural groups. It intends to examine their similar and dissimilar traits with a view to unearthing their common grounds in the early times of their history. The study uses both the primary and secondary sources of data. A thematic study, the paper adopts the analytic and narrative approaches of history as its methodology. The paper finds facts in some deities bearing the same name in both clans, initiations rites that serve the same purpose among the groups, same belief systems, some common customs and norms, veneration methods for social violations, and many other common traits in the lives of the two groups, as proofs that the people had had many things in common in their early history. With these findings, the paper holds that Afikpo andAbakaliki people migrated from same place,and later settled together for some centuries at a commonlocation Article Original where they evolved some of their cultures before wars and other exigencies of the environment scattered them to new settlements.