Byaruhanga-Cobams-Msc
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ministry of Education,Science,Technology And
Vote Performance Report and Workplan Financial Year 2015/16 Vote: 013 Ministry of Education, Science, Technology and Sports Structure of Submission QUARTER 3 Performance Report Summary of Vote Performance Cumulative Progress Report for Projects and Programme Quarterly Progress Report for Projects and Programmes QUARTER 4: Workplans for Projects and Programmes Submission Checklist Page 1 Vote Performance Report and Workplan Financial Year 2015/16 Vote: 013 Ministry of Education, Science, Technology and Sports QUARTER 3: Highlights of Vote Performance V1: Summary of Issues in Budget Execution This section provides an overview of Vote expenditure (i) Snapshot of Vote Releases and Expenditures Table V1.1 below summarises cumulative releases and expenditures by the end of the quarter: Table V1.1: Overview of Vote Expenditures (UShs Billion) Approved Cashlimits Released Spent by % Budget % Budget % Releases (i) Excluding Arrears, Taxes Budget by End by End End Mar Released Spent Spent Wage 11.218 9.015 9.015 8.648 80.4% 77.1% 95.9% Recurrent Non Wage 131.229 109.486 108.844 104.885 82.9% 79.9% 96.4% GoU 62.227 41.228 28.424 24.904 45.7% 40.0% 87.6% Development Ext Fin. 200.477 N/A 77.806 77.806 38.8% 38.8% 100.0% GoU Total 204.674 159.728 146.283 138.436 71.5% 67.6% 94.6% Total GoU+Ext Fin. (MTEF) 405.150 N/A 224.089 216.242 55.3% 53.4% 96.5% Arrears 0.642 N/A 0.642 0.553 100.0% 86.1% 86.1% (ii) Arrears and Taxes Taxes** 19.258 N/A 12.804 2.548 66.5% 13.2% 19.9% Total Budget 425.050 159.728 237.535 219.343 55.9% 51.6% 92.3% * Donor expenditure -

Assessment Form
Local Government Performance Assessment Mukono Municipal Council (Vote Code: 772) Assessment Scores Accountability Requirements % Crosscutting Performance Measures 73% Educational Performance Measures 77% Health Performance Measures 61% Water & Environment Performance Measures 0% 772 Accountability Requirements 2019 Mukono Municipal Council Definition of No. Summary of requirements Compliance justification Compliant? compliance Annual performance contract 1 Yes LG has submitted an annual • From MoFPED’s Mukono MC submitted the Annual performance contract of the inventory/schedule of Performance Contract of the forthcoming forthcoming year by June 30 on the LG submissions of year on 23rd July 2019. This is within the basis of the PFMAA and LG performance contracts, adjusted deadline of 31st August 2019. Budget guidelines for the coming check dates of Thus, the LG is compliant. financial year. submission and issuance of receipts and: o If LG submitted before or by due date, then state ‘compliant’ o If LG had not submitted or submitted later than the due date, state ‘non- compliant’ • From the Uganda budget website: www.budget.go.ug, check and compare recorded date therein with date of LG submission to confirm. Supporting Documents for the Budget required as per the PFMA are submitted and available 2 Yes LG has submitted a Budget that • From MoFPED’s The Approved Budget for Mukono MC includes a Procurement Plan for inventory of LG budget dated 23rd July 2019 had a Procurement the forthcoming FY by 30th June submissions, check Plan for FY 2019/2020 attached. (LG PPDA Regulations, 2006). whether: o The LG budget is accompanied by a Procurement Plan or not. -
A Case of Mwanamugimu Nutrition Unit, Mulago National Referral
SIT Graduate Institute/SIT Study Abroad SIT Digital Collections Independent Study Project (ISP) Collection SIT Study Abroad Fall 2013 A Comparison of Malnutrition Causes and Treatments: A Case of Mwanamugimu Nutrition Unit, Mulago National Referral Hospital, Kampala District and Nakifuma Government Health Unit, Mukono District Berkley Singer SIT Study Abroad Follow this and additional works at: https://digitalcollections.sit.edu/isp_collection Part of the Community-Based Research Commons, Community Health and Preventive Medicine Commons, Family, Life Course, and Society Commons, Health Services Research Commons, Inequality and Stratification Commons, Maternal and Child Health Commons, Place and Environment Commons, and the Public Health Education and Promotion Commons Recommended Citation Singer, Berkley, "A Comparison of Malnutrition Causes and Treatments: A Case of Mwanamugimu Nutrition Unit, Mulago National Referral Hospital, Kampala District and Nakifuma Government Health Unit, Mukono District" (2013). Independent Study Project (ISP) Collection. 1693. https://digitalcollections.sit.edu/isp_collection/1693 This Unpublished Paper is brought to you for free and open access by the SIT Study Abroad at SIT Digital Collections. It has been accepted for inclusion in Independent Study Project (ISP) Collection by an authorized administrator of SIT Digital Collections. For more information, please contact [email protected]. A Comparison of Malnutrition Causes and Treatments: A Case of Mwanamugimu Nutrition Unit, Mulago National Referral Hospital, Kampala District and Nakifuma Government Health Unit, Mukono District Berkley Singer Advisor: Dr. Jolly Kamugisha Academic Director: Dr. Charlotte Mafumbo Fall 2013 Acknowledgement: I would like to acknowledge Dr. Charlotte Mafumbo for all her hard work and dedication throughout the research process. She is an amazing worker and deserves all the praise in the world. -

October 21 2017 Thesis New Changes Tracked
The Status, Rights and Treatment of Persons with Disabilities within Customary Legal Frameworks in Uganda: A Study of Mukono District By David Brian Dennison BA (honours), MBA, JD (cum laude) (University of Georgia, USA) Thesis Presented for the Degree of Doctor of Philosophy in the Department of Private TownLaw Faculty of Law UNIVERSITY OF CAPE TOWN Cape of Date of submission: 31 October 2017 Supervisor: Professor Chuma Himonga University Department of Private Law University of Cape Town The copyright of this thesis vests in the author. No quotation from it or information derivedTown from it is to be published without full acknowledgement of the source. The thesis is to be used for private study or non- commercial research purposes Capeonly. of Published by the University of Cape Town (UCT) in terms of the non-exclusive license granted to UCT by the author. University The copyright for this thesis rests with the University of Cape Town. No quotation from it or information derived from it is to be published without full acknowledgment of the source. The thesis is to be used for private study or non-commercial research purposes only. "ii ABSTRACT Thesis Title: The Status, Rights and Treatment of Persons with Disabilities within Customary Legal Frameworks in Uganda: A Study of Mukono District Submitted by: David Brian Dennison on 31 October 2017 This thesis addresses the question: How do customary legal frameworks impact the status, rights and treatment of persons with disabilities? It is motivated by two underlying premises. First, customary legal frameworks are highly consequential in Sub-Saharan contexts. -

NATIONAL YOUTH SYMPOSIUM YOUTH in AGRIBUSINESS: for Income Generation and Job Creation
NATIONAL YOUTH SYMPOSIUM YOUTH IN AGRIBUSINESS: For income generation and job creation SUMMARY REPORT Debate Winners: Gayaza High School receiving a certificate of recognition during the National Youth Symposium at the Source of the Nile, Jinja National Agricultural & Trade show held on 20th July 2018. “Farmers must deal with the “madness” in farming of practising the same thing over and over and expecting different results. Farmers need to get more organised” said Agume Bless, AgriProFocus youth member. Introduction AgriProFocus in partnership with Uganda National Young Farmers Association (UNYFA) organised a National Youth Symposium held on Friday the 20th July 2018. The symposium was organised under the National Agricultural & Trade Show in Jinja which provides a unique understanding of the entire food chain. The symposium was dubbed under the theme; ‘Youth in agribusiness for income generation and job creation’ with an overall objective of unlocking the underlying business opportunities for youth in the agribusiness sector. In order to achieve the above mentioned objective, the day’s program consisted of the following activities; 1. Keynote Address on Youth in Agribusiness: opportunities for income enhancement and job creation. 2. A panel of discussants on topical issues i.e learning opportunities, agribusiness opportunities 3. A School’s Agribusiness debate between Gayaza High school and Namilyango College 4. Sharing of Success Stories by the youth entrepreneurs. Participants: The symposium was attended by a cross section of people from civil society organisations, students from different schools at different levels, farmer organisations, Government representatives, the media, the private sector as well as development partners. During the symposium, a total of 100 participants who expressed interest to join the AgriProFocus online platform were registered. -

UGANDA: PLANNING MAP (Details)
IMU, UNOCHA Uganda http://www.ugandaclusters.ug http://ochaonline.un.org UGANDA: PLANNING MAP (Details) SUDAN NARENGEPAK KARENGA KATHILE KIDEPO NP !( NGACINO !( LOPULINGI KATHILE AGORO AGU FR PABAR AGORO !( !( KAMION !( Apoka TULIA PAMUJO !( KAWALAKOL RANGELAND ! KEI FR DIBOLYEC !( KERWA !( RUDI LOKWAKARAMOE !( POTIKA !( !( PAWACH METU LELAPWOT LAWIYE West PAWOR KALAPATA MIDIGO NYAPEA FR LOKORI KAABONG Moyo KAPALATA LODIKO ELENDEREA PAJAKIRI (! KAPEDO Dodoth !( PAMERI LAMWO FR LOTIM MOYO TC LICWAR KAPEDO (! WANDI EBWEA VUURA !( CHAKULYA KEI ! !( !( !( !( PARACELE !( KAMACHARIKOL INGILE Moyo AYUU POBURA NARIAMAOI !( !( LOKUNG Madi RANGELAND LEFORI ALALI OKUTI LOYORO AYIPE ORAA PAWAJA Opei MADI NAPORE MORUKORI GWERE MOYO PAMOYI PARAPONO ! MOROTO Nimule OPEI PALAJA !( ALURU ! !( LOKERUI PAMODO MIGO PAKALABULE KULUBA YUMBE PANGIRA LOKOLIA !( !( PANYANGA ELEGU PADWAT PALUGA !( !( KARENGA !( KOCHI LAMA KAL LOKIAL KAABONG TEUSO Laropi !( !( LIMIDIA POBEL LOPEDO DUFILE !( !( PALOGA LOMERIS/KABONG KOBOKO MASALOA LAROPI ! OLEBE MOCHA KATUM LOSONGOLO AWOBA !( !( !( DUFILE !( ORABA LIRI PALABEK KITENY SANGAR MONODU LUDARA OMBACHI LAROPI ELEGU OKOL !( (! !( !( !( KAL AKURUMOU KOMURIA MOYO LAROPI OMI Lamwo !( KULUBA Koboko PODO LIRI KAL PALORINYA DUFILE (! PADIBE Kaabong LOBONGIA !( LUDARA !( !( PANYANGA !( !( NYOKE ABAKADYAK BUNGU !( OROM KAABONG! TC !( GIMERE LAROPI PADWAT EAST !( KERILA BIAFRA !( LONGIRA PENA MINIKI Aringa!( ROMOGI PALORINYA JIHWA !( LAMWO KULUYE KATATWO !( PIRE BAMURE ORINJI (! BARINGA PALABEK WANGTIT OKOL KINGABA !( LEGU MINIKI -

Vote:542 Mukono District Quarter1
Local Government Quarterly Performance Report FY 2019/20 Vote:542 Mukono District Quarter1 Terms and Conditions I hereby submit Quarter 1 performance progress report. This is in accordance with Paragraph 8 of the letter appointing me as an Accounting Officer for Vote:542 Mukono District for FY 2019/20. I confirm that the information provided in this report represents the actual performance achieved by the Local Government for the period under review. Nkata. B. James Date: 05/12/2019 cc. The LCV Chairperson (District) / The Mayor (Municipality) 1 Local Government Quarterly Performance Report FY 2019/20 Vote:542 Mukono District Quarter1 Summary: Overview of Revenues and Expenditures Overall Revenue Performance Ushs Thousands Approved Budget Cumulative Receipts % of Budget Received Locally Raised Revenues 2,165,188 541,297 25% Discretionary Government 4,425,042 1,190,092 27% Transfers Conditional Government Transfers 35,247,076 9,611,327 27% Other Government Transfers 3,791,074 663,098 17% External Financing 256,500 42,410 17% Total Revenues shares 45,884,879 12,048,224 26% Overall Expenditure Performance by Workplan Ushs Thousands Approved Cumulative Cumulative % Budget % Budget % Releases Budget Releases Expenditure Released Spent Spent Administration 7,460,303 2,150,500 1,922,394 29% 26% 89% Finance 469,132 114,856 85,192 24% 18% 74% Statutory Bodies 1,007,284 252,999 177,696 25% 18% 70% Production and Marketing 2,330,532 595,709 469,467 26% 20% 79% Health 6,530,010 1,841,368 1,760,879 28% 27% 96% Education 24,190,088 6,039,281 5,341,989 -

Croc's 05.Qxd
CLASSIFIED ADVERTS NEW VISION, Tuesday, June 5, 2012 35 RABBAI “With Trust & Honesty” Sema Properties Ltd Tested & Reliable Housing HOSSANA REAL .....we settle you RABBAI REAL ESTATES HERITAGE SITES LTD Vacancies Vacancies SPECIAL OFFER 10% DISCOUNT RentWell surveyed plots with ready Sema Properties Ltd ESTATES LTD RentON ALL PLOTS “Your Home, Your Prestige” Mailo Land Titles. 1. NAKAWUKA Entebbe Road Real Estate Developers, CANAAN SITES UP TO 30TH JUNE, 2012 CCANAANANAAN SSITESITES Surveyors & Contractors PLANNED PLOTS WITH WELL PLANNED AND ORGANISED with green Environment - ZION PLOTS WITH TITLES, “FIRST STEP TO NEW HOME” 1. GAYAZA-ZIROBWE 50 x 100ft = 4.5m Well planned plots with Mailo land PRIVATE MAILO LAND ESTATES WITH MAILO LAND TITLES, titles at hand. Water & power and accessible SEVERAL PLOTS WITH MAILO WATER & POWER. 1 Km from tarmac 100 x 100ft = 9m TITLES LAND TITLES AT HAND. 50 x 100ft - 3.6m 1. MUKONO-KAYANJA with public means. 1. GAYAZA KIRA ROYAL ESTATE 2. MATUGGA Migadde. 1. KAKIRI-MWERA PHASE II 1. KAKIRI-Hoima Road 50 x 100 ft - 2.3m (Cash) 50 x 100ft - 2.5m All tarmac from Kampala to the 100 x 100ft - 7.2m Good view of Kampala & 1. MATUGA-KIWEBWA 50ft x 100ft - 2.5m Estate with mailo land titles. 50 x 100 ft - 2.6m (Instalments) 100 x 100ft - 5m 2. GAYAZA RD, near main road 100 x 100 ft - 4.6m ESTATE 100ft x 100ft - 5m 50 x 100ft - 10m & 14m 2. MUKONO-Kayunga Road, 50 X 100ft 2.5m & 3.5m Live like Vice President NAKASAJJA 50 x 100ft = 3.5m 2. -

Mukono Town Council
MUKONO TOWN COUNCIL Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized Env ironmental Impact Statement for the Proposed Waste Composting Plant and Landfill in Katikolo Village, Mukono Town Council Prepared By: Enviro-Impact and Management Consults Total Deluxe House, 1ST Floor, Plot 29/33, Jinja Road Public Disclosure Authorized P.O. Box 70360 Kampala, Tel: 41-345964, 31-263096, Fax: 41-341543 E-mail: [email protected] Web Site: www.enviro-impact.co.ug September 2006 Mukono Town Council PREPARERS OF THIS REPORT ENVIRO-IMPACT and MANAGEMENT CONSULTS was contracted by Mukono Town Council to undertake the Environmental impact Assessment study of the proposed Katikolo Waste Composting Plant and Landfill, and prepare this EIS on their behalf. Below is the description of the lead consultants who undertook the study. Aryagaruka Martin BSc, MSc (Natural Resource Management) Team Leader ………………….. Otim Moses BSc, MSc (Industrial Chemistry/Environmental Systems Analysis) …………………… Wilbroad Kukundakwe BSc Industrial Chemistry …………………… EIS Katikolo Waste Site i EIMCO Environmental Consultants Mukono Town Council TABLE OF CONTENTS PREPARERS OF THIS REPORT.....................................................................I ACKNOWLEDGEMENTS ........................................................................... VI ABBREVIATIONS AND ACRONYMS .............................................................. VI EXECUTIVE SUMMARY.....................................................................................VII -

COVID-19 Effects on the Construction Industry
Issue No. 15, August 2020 THEME: COVID-19 & CONSTRUCTION SAFETY: Keep your site safe during COVID-19 crisis COVID-19: Govt’s intervention to aid sector ’s recovery is crucial RULES: Strict regulation key in eliminating shoddy work COVID-19 effects on the construction industry www.unabcec.co.ug UNABCEC UNABCEC_UG AUGUST, 2020 1 COVID-19 should The Contractor Magazine is a quarterly publication that acts as the voice for the leave you with AUTHENTIC ICON construction industry. We print and distribute The Contractor free of charge to UNABCEC many lessons members and all stakeholders in the construc- tion industry, international and local partners, am excited about this particular is- ministries, departments and agencies, works sue of The Contractor, you should and technical officers of all central and local I too, and this is why. Government entities, Members of Parliament, The lockdown was lifted and for banks, embassies, academic institutions and most sectors, work has resumed nor- the general public. We highlight issues and mally. Although operations of the con- possible solutions relating to the construction struction sector had not been halted as that usually happen at construction business community. Visit our website today to sites. Therefore, in addition to wear- access soft copies of the recent issues. part of measures to prevent the spread of the pandemic, operations were ing masks, do not downplay helmets, Call for articles made difficult by several restrictions, boots, reflectors and other safety gear. All articles on construction experiences, including movement of workers and More than this, insure your workers opinions on developing the industry, policy closure of material outlets. -

Bachelor of Science in Software Engineering
BACHELOR OF SCIENCE IN SOFTWARE ENGINEERING COURSE CODE BSW INDEX NO NAME Al Yr SEX C'TRY SCHOOL 1 U0068/571 KATIRIMA Allan Phene Junior 2010 M U NTARE SCHOOL 2 U0956/965 SEMATIKO Douglas 2010 M U NAMIREMBE HILLSIDE S.S. 3 U1224/590 JUUKO Marvin 2010 M U ST MARY'S SS KITENDE 4 U0459/658 EKINAMUSHABIRE Preciou 2010 M U KAWEMPE MUSLIM SS 5 U0068/562 BYAMUGISHA Innocent 2010 M U NTARE SCHOOL 6 U0334/620 MUWONGE Bright Hosea 2010 M U UGANDA MARTYRS S.S., NAMUGONGO 7 U0068/585 MATSIKO Grace 2010 M U NTARE SCHOOL 8 U1223/634 NAMUTEBI Veronica 2010 F U SEETA HIGH SCHOOL 9 U0763/806 MUGISA Nicholas 2010 M U BUDDO SEC. SCHOOL 10 U0334/554 NAMPOGO Adrian Mwota 2010 M U UGANDA MARTYRS S.S., NAMUGONGO 11 U0063/552 NAKAYENGA Catherine 2010 F U MT.ST.MARY'S, NAMAGUNGA 12 U0956/960 MUGYENYI Martin 2010 M U NAMIREMBE HILLSIDE S.S. 13 U1085/517 AYESIGA Agnes 2010 F U BP CYPRIAN KIHANGIRE SS LUZIRA 14 U0794/590 ARINAITWE Tumusiime Bryan 2010 M U GREENHILL ACADEMY, KAMPALA 15 U0004/556 NAKALEMBE Margaret 2010 F U KING'S COLLEGE, BUDO 16 U1379/694 SSEGUJJA Conrad Micheal 2010 M U LUGAZI MIXED SEC. SCH. 17 U0082/579 NDYAMUHAKI Joseph 2010 M U ST.KAGGWA BUSHENYI HIGH SCH. 18 U1509/547 NALWADDA Dorothy 2010 F U COMPREHENSIVE COLLEGE KITETIKKA 19 U1224/813 OPIYO Brian Lamtoo 2010 M U ST MARY'S SS KITENDE 20 U0387/548 LUBEGA Edrin Evarest 2010 M U ST.PETER'S S S, NSAMBYA 21 U0068/607 NAHAMYA Colins 2010 M U NTARE SCHOOL 22 U0064/521 KABENGE Shem 2010 M U NAMILYANGO COLLEGE 23 U0064/502 AINOMUGISHA Solomon 2010 M U NAMILYANGO COLLEGE 24 U0459/694 NANKABIRWA Namusisi Linda 2010 F U KAWEMPE MUSLIM SS 25 U0030/709 MUBAZI Eric John 2010 M U KITANTE HILL SCHOOL 26 U0041/998 NANZIRI Bonita Beatrice 2010 F U LUBIRI SECONDARY SCHOOL 27 U0043/686 MUHEREZA Nicholas 2010 M U MAKERERE COLLEGE SCHOOL 28 U2339/533 SEBAGALA Charles 2010 M U ST. -
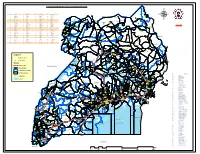
Legend " Wanseko " 159 !
CONSTITUENT MAP FOR UGANDA_ELECTORAL AREAS 2016 CONSTITUENT MAP FOR UGANDA GAZETTED ELECTORAL AREAS FOR 2016 GENERAL ELECTIONS CODE CONSTITUENCY CODE CONSTITUENCY CODE CONSTITUENCY CODE CONSTITUENCY 266 LAMWO CTY 51 TOROMA CTY 101 BULAMOGI CTY 154 ERUTR CTY NORTH 165 KOBOKO MC 52 KABERAMAIDO CTY 102 KIGULU CTY SOUTH 155 DOKOLO SOUTH CTY Pirre 1 BUSIRO CTY EST 53 SERERE CTY 103 KIGULU CTY NORTH 156 DOKOLO NORTH CTY !. Agoro 2 BUSIRO CTY NORTH 54 KASILO CTY 104 IGANGA MC 157 MOROTO CTY !. 58 3 BUSIRO CTY SOUTH 55 KACHUMBALU CTY 105 BUGWERI CTY 158 AJURI CTY SOUTH SUDAN Morungole 4 KYADDONDO CTY EST 56 BUKEDEA CTY 106 BUNYA CTY EST 159 KOLE SOUTH CTY Metuli Lotuturu !. !. Kimion 5 KYADDONDO CTY NORTH 57 DODOTH WEST CTY 107 BUNYA CTY SOUTH 160 KOLE NORTH CTY !. "57 !. 6 KIIRA MC 58 DODOTH EST CTY 108 BUNYA CTY WEST 161 OYAM CTY SOUTH Apok !. 7 EBB MC 59 TEPETH CTY 109 BUNGOKHO CTY SOUTH 162 OYAM CTY NORTH 8 MUKONO CTY SOUTH 60 MOROTO MC 110 BUNGOKHO CTY NORTH 163 KOBOKO MC 173 " 9 MUKONO CTY NORTH 61 MATHENUKO CTY 111 MBALE MC 164 VURA CTY 180 Madi Opei Loitanit Midigo Kaabong 10 NAKIFUMA CTY 62 PIAN CTY 112 KABALE MC 165 UPPER MADI CTY NIMULE Lokung Paloga !. !. µ !. "!. 11 BUIKWE CTY WEST 63 CHEKWIL CTY 113 MITYANA CTY SOUTH 166 TEREGO EST CTY Dufile "!. !. LAMWO !. KAABONG 177 YUMBE Nimule " Akilok 12 BUIKWE CTY SOUTH 64 BAMBA CTY 114 MITYANA CTY NORTH 168 ARUA MC Rumogi MOYO !. !. Oraba Ludara !. " Karenga 13 BUIKWE CTY NORTH 65 BUGHENDERA CTY 115 BUSUJJU 169 LOWER MADI CTY !.