GARP-Nepal National Working Group (NWG)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Some Notes on Nepali Castes and Sub-Castes—Jat and Thar
SOME NOTES ON NEPALI CASTES AND SUB-CASTES- JAT AND THAR. - Suresh Singh This paper attempts to make a re-presentation of evolution and construction of Jat and Thar system among the Parbatya or hill people of Nepal. It seeks to expose the reality behind the myth that the large number of Aryans migrated from Indian plains due to Muslim invasion and conquered to become the rulers in Nepal, and the Mongoloids were the indigenous people. It also seeks to show the construction and reconstruction of identity of the different castes (Jats) and subcastes (Thars). The Nepalese history is lost in legends and fables. Archaeological data, which might shed light on the early years, are practically nonexistent or largely unexplored, because the Nepalese Government has not encouraged such research within its borders. However, there seem to be a number of sites that might yield valuable find, once proper excavation take place. Another problem seems to be that history writing is closely connected with the traditional conception of Nepali historiography, constructed and intervened by the efforts of the ruling elite. Many of the written documents have been re-presented to legitimatize the ruling elite’s claim to power. As it is well known from political history, the social history, too, becomes an interpretation from the view of the Kathmandu valley, and from the Indian or alleged Indian immigrants and priestly class. It is difficult to imagine, that Aryans came to Nepal in greater numbers about 600 years ago, and because of their mental superiority and their noble character, they were asked by the people to become the rulers of their small states. -

Nepal: Rural Reconstruction and Rehabilitation Sector Development Project
Resettlement Planning Document Due Diligence Report Resettlement Grant Number: 0093 April 2010 Nepal: Rural Reconstruction and Rehabilitation Sector Development Project Surunga-Sharnamati-Tagandubba-Digalbank Road Sub-Project, Jhapa (0+000-23+704) Prepared by the Government of Nepal for the Asian Development Bank. This resettlement plan is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. Your attention is directed to the “terms of use” section of this website. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. Government of Nepal Ministry of Local Development Office of District Development Committee District Technical Office Jhapa Rural Reconstruction and Rehabilitation Sector Development Program Resettlement Statement Document of Surunga – Sharnamati – Tagandubba – Digalbank Road Sub-project (0+000-23+704) April 2010 Abbreviation ADB Asian Development Bank APs Affected People CDC Compensation Determination Committee CDO Chief District Officer CISC Central Implementation Support Consultant DDC District Development Committee DIST District Implementation Support Team DPO District Project Office DoLIDAR Department of Local Infrastructure Development and Agricultural Roads -
Branch Account Name
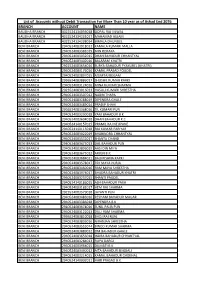
List of Accounts without Debit Transaction For More Than 10 year as of Ashad End 2076 BRANCH ACCOUNT NAME BAUDHA BRANCH 4322524134056018 GOPAL RAJ SILWAL BAUDHA BRANCH 4322524134231017 MAHAMAD ASLAM BAUDHA BRANCH 4322524134298014 BIMALA DHUNGEL BENI BRANCH 2940524083918012 KAMALA KUMARI MALLA BENI BRANCH 2940524083381019 MIN ROKAYA BENI BRANCH 2940524083932015 DHAN BAHADUR CHHANTYAL BENI BRANCH 2940524083402016 BALARAM KHATRI BENI BRANCH 2922524083654016 SURYA BAHADUR PYAKUREL (KHATRI) BENI BRANCH 2940524083176016 KAMAL PRASAD POUDEL BENI BRANCH 2940524083897015 MUMTAJ BEGAM BENI BRANCH 2936524083886017 SHUSHIL KUMAR KARKI BENI BRANCH 2940524083124016 MINA KUMARI SHARMA BENI BRANCH 2923524083016013 HASULI KUMARI SHRESTHA BENI BRANCH 2940524083507012 NABIN THAPA BENI BRANCH 2940524083288019 DIPENDRA GHALE BENI BRANCH 2940524083489014 PRADIP SHAHI BENI BRANCH 2936524083368016 TIL KUMARI PUN BENI BRANCH 2940524083230018 YAM BAHADUR B.K. BENI BRANCH 2940524083604018 DHAN BAHADUR K.C BENI BRANCH 2940524140157015 PRAMIL RAJ NEUPANE BENI BRANCH 2940524140115018 RAJ KUMAR PARIYAR BENI BRANCH 2940524083022019 BHABINDRA CHHANTYAL BENI BRANCH 2940524083532017 SHANTA CHAND BENI BRANCH 2940524083475013 DAL BAHADUR PUN BENI BRANCH 2940524083896019 AASI DIN MIYA BENI BRANCH 2940524083675012 ARJUN B.K. BENI BRANCH 2940524083684011 BALKRISHNA KARKI BENI BRANCH 2940524083578017 TEK MAYA PURJA BENI BRANCH 2940524083460016 RAM MAYA SHRESTHA BENI BRANCH 2940524083974017 BHADRA BAHADUR KHATRI BENI BRANCH 2940524083237015 SHANTI PAUDEL BENI BRANCH 2940524140186015 -
List of Active Agents
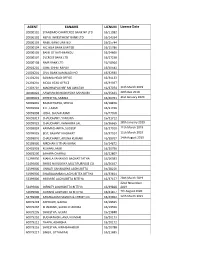
AGENT EANAME LICNUM License Date 20000101 STANDARD CHARTERED BANK NP LTD 16/11082 20000102 NEPAL INVESTMENT BANK LTD 16/14334 20000103 NABIL BANK LIMITED 16/15744 20000104 NIC ASIA BANK LIMITED 16/15786 20000105 BANK OF KATHMANDU 16/24666 20000107 EVEREST BANK LTD. 16/27238 20000108 NMB BANK LTD 16/18964 20901201 GIME CHHETRAPATI 16/30543 21001201 CIVIL BANK KAMALADI HO 16/32930 21101201 SANIMA HEAD OFFICE 16/34133 21201201 MEGA HEAD OFFICE 16/34037 21301201 MACHHAPUCHRE BALUWATAR 16/37074 11th March 2019 40000022 AAWHAN BAHUDAYSIYA SAHAKARI 16/35623 20th Dec 2019 40000023 SHRESTHA, SABINA 16/40761 31st January 2020 50099001 BAJRACHARYA, SHOVA 16/18876 50099003 K.C., LAXMI 16/21496 50099008 JOSHI, SHUVALAXMI 16/27058 50099017 CHAUDHARY, YAMUNA 16/31712 50099023 CHAUDHARY, KANHAIYA LAL 16/36665 28th January 2019 50099024 KARMACHARYA, SUDEEP 16/37010 11th March 2019 50099025 BIST, BASANTI KADAYAT 16/37014 11th March 2019 50099026 CHAUDHARY, ARUNA KUMARI 16/38767 14th August 2019 50199000 NIRDHAN UTTHAN BANK 16/14872 50401003 KISHAN LAMKI 16/20796 50601200 SAHARA CHARALI 16/22807 51299000 MAHILA SAHAYOGI BACHAT TATHA 16/26083 51499000 SHREE NAVODAYA MULTIPURPOSE CO 16/26497 51599000 UNNATI SAHAKARYA LAGHUBITTA 16/28216 51999000 SWABALAMBAN LAGHUBITTA BITTIYA 16/33814 52399000 MIRMIRE LAGHUBITTA BITTIYA 16/37157 28th March 2019 22nd November 52499000 INFINITY LAGHUBITTA BITTIYA 16/39828 2019 52699000 GURANS LAGHUBITTA BITTIYA 16/41877 7th August 2020 52799000 KANAKLAXMI SAVING & CREDIT CO. 16/43902 12th March 2021 60079203 ADHIKARI, GAJRAJ -

35173-015: Urban Water Supply and Sanitation (Sector) Project
Land Acquisition, Involuntary Resettlement and Indigenous Peoples Due Diligence Report Document Stage: Draft for consultation Project Number: 35173-015 January 2021 Nepal: Urban Water Supply and Sanitation (Sector) Project – Dadhikot Urban Water Supply and Sanitation Project, Suryabinayak Municipality, Bhaktapur (PART B) Package Number: W-20 Prepared by the Ministry of Water Supply, Government of Nepal for the Asian Development Bank. This draft land acquisition and involuntary resettlement due diligence report is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. Your attention is directed to the “terms of use” section of this website. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. DDR of Dadhikot UWSSP BDA - JPZ- UDAYA Consultants (P) Ltd., January 2021 Appendix-8, B Phone no.: 01-6631215 Suryabinayak Municipality 4 No. Ward Office, Dadhikot Bhaktapur, Bagmati Province, Nepal Letter No.: Dispatched No.: 421 Date: 24thSeptember 2020 (2077/06/08) To whom it may concern Subject: Regarding Users Committee Continuation In reference to the above subject, Dadhikot Brihat Water Supply and Sanitation Main Users Committee that registered in Office of District Water Resource Committee, Bhaktapur, registration no.2150 (registration date: 15th July 2015 / 2072-03-30) is providing water supply in the then Dadhikot VDC, ward no.3, 6, 7, 8, 9. -
Gaurishankar 2067 68
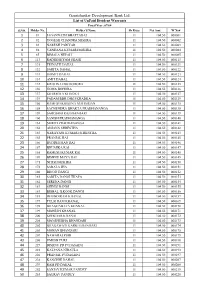
Gaurishankar Development Bank Ltd. List of UnPaid Divident Warrants Fiscal Year :67/68 S.NO. Holder No. Holder'S Name Sh Kitta Net Amt W No# 1 81 JAGANNATH BHATTARAI 11 104.50 000081 2 82 YOGESH CHANDRA MISHRA 11 104.50 000082 3 83 NARESH PARIYAR 11 104.50 000083 4 84 VANDANA KUMARI MISHRA 11 104.50 000084 5 85 BIMALA NEPALI 11 104.50 000085 6 113 RADHESHYAM SHAHI 11 104.50 000113 7 131 TEJNATH DAHAL 11 104.50 000121 8 132 SARITA DAHAL 11 104.50 000122 9 133 ISHMIT DAHAL 11 104.50 000123 10 134 AMIT DAHAL 11 104.50 000124 11 135 KRISHNA DOJ BOHORA 11 104.50 000125 12 136 GOMA BOHORA 11 104.50 000126 13 137 SHARMILA KHADKA 11 104.50 000127 14 139 PADAM BDR DHOJ KHADKA 11 104.50 000129 15 150 RAMESH KRISHNA MAHARJAN 11 104.50 000135 16 158 SACHENDRA BHAKTA PRADHANANGA 11 104.50 000138 17 159 SAROJANI RAJBHANDARI 11 104.50 000139 18 160 SANISH PRADHANANGA 11 104.50 000140 19 161 SMRITI PRADHANANGA 11 104.50 000141 20 162 ANJANA SHRESTHA 11 104.50 000142 21 163 NARAYANI KUMARI SHRESTHA 11 104.50 000143 22 165 PRANJAL RAI 11 104.50 000145 23 166 BUDDHI MAN RAI 11 104.50 000146 24 167 BHUMIKA RAI 11 104.50 000147 25 168 RAMESH KUMAR RAI 11 104.50 000148 26 169 BISHNU MAYA RAI 11 104.50 000149 27 171 NITISH MISHRA 11 104.50 000150 28 172 SARALA JHA 11 104.50 000151 29 180 BINOD DANGI 11 104.50 000152 30 181 SARITA DANGI THAPA 11 104.50 000153 31 182 SERENA DANGI 11 104.50 000154 32 183 SHINBI DANGI 11 104.50 000155 33 184 BISHAL ILKOOK DANGI 11 104.50 000156 34 185 DHUNDIRAM KHANAL 11 104.50 000157 35 197 TULSI RAM KHANAL 11 104.50 000169 36 -

Executive Board Meeting March. 10Th 2018 Chair By: President Dr
Executive Board Meeting March. 10th 2018 Chair by: President Dr. Keshab Paudel Moderated by : General Secretary Mr. Babu Ram (BR) Lama General Secretary Mr. Babu Ram (BR) Lama called the NRNA NCC USA EXECUTIVE BOARD 2017-19 6th bOard meeting On the authOrity Of President Dr. Keshab Paudel’s directiOn to Order in March 10th 2018 at 9:30 pm EST On the https://glObal.gOtomeeting.cOm/jOin/772994637 and, thOse in attendance and cOnstituting a quOrum were: S.N. Name Designation Attend 1 Dr. Keshab Paudel President Yes 2 Mr. Suneel Sah Senior Vice President No 3 Ms. Radha K Paudel Mid-West R.Vice President Yes 4 Mr. Ram Kumar Subedi NOrth East R. Vice President Yes 5 Mr. Jedu Pokhrel SOuth R. Vice President Yes 6 Ms. Uma Karki Thapa West R. Vice President No 7 Mr. Babu Ram Lama General Secretary Yes 8 Mr. Hom Nath Gautam Secretary Yes 9 Dr. Prakash Aryal Treasurer Yes 10 Mr. Pawan YOnjan JOint Treasurer Yes 11 Mr. Bal K JOshi Media COOrdinator No 12 Mr. BinOd K Tiwari Spokesperson Yes 13 Mr. Swaraj Khati YOuth COOrdinator Yes 14 Ms. Idira Tripathi WOman COOrdinator Yes 15 Dr. Arjun Banjade BOD Yes 16 Mr. Krishna P Lamichhane BOD Yes 17 Ms. Trishna Sharma BOD Yes 18 Mr. Sanjay Thapa BOD Yes 19 Ms. Divya KC Oli BOD Yes 20 Mr. GOpendra Bhattarai BOD Yes 21 Ms. Bindu SapkOta BOD No 22 Mr. Amrit Babu Kattel BOD Yes 23 Mr. Priti Sagar Khatri BOD Yes 24 Mr. Angngima G Sherpa BOD Yes 25 Mr. -
Nepal Customary Right Reportpdf
Documentation and assessing customary practices of managing forest resources at local level REDD Implementation Centre Ministry of Forests and Soil Conservation Babar Mahal, Kathmandu, Nepal August 25, 2015 Produced by Nav Raj Baral Produced for REDD Implementation Centre, Ministry of Forests and SoilConservation, Nepal Copyright © REDD Implementation Centre, Ministry of Forests andSoil Conservation, Nepal Version Final Disclaimer: Although the REDD Implementation Centre, Ministry of Forests and Soil Conservation, Nepal, commissioned this study, neither the REDD IC nor the government assumes any responsibility for the accuracy, completeness, or usefulness of any information in the report. ii Acknowledgements Many individuals and institutions have contributed to this study and made it possible for me to complete this assignment. Therefore, I wish to thank all community members and respondents of Sankhuwsabha, Panchthar, Jhapa, Bara and Sarlahi, Sindhuli, Dolkha, Sindhuplachowk, Chitwan, Nawalparasi, Jumla, Kailali and Doti districts for sharing their views and insights, as well as their time and hospitality. I am very much grateful to REDD Implementation Centre, Ministry of Forest and Soil Conservation Babarmahal for entrusting me with this assignment and providing necessary technical and institutional support related to the assignment. It has helped a lot to enrich my knowledge and skills on this important subject and also to work with a number of government officials, professional scholars, farmers and their networks. I would like to offer special thanks to Mr. Man Bahadur Khadaka, Chief REDD IC and also to Mr. Rajnedra Kafley, the former REDD IC Chief and all officials of REDD. I would like to thank in particular Dr. Narendra Chand, Mr.Mohan Khanal, and Mr. -
Pangolin Conservation Action Plan for Nepal (2018-2022)
Pangolin Conservation Action Plan for Nepal (2018-2022) Government of Nepal Ministry of Forests and Environment Department of National Parks and Wildlife Conservation Department of Forests 2018 Pangolin Conservation Action Plan for Nepal (2018-2022) Government of Nepal Ministry of Forests and Environment Department of National Parks and Wildlife Conservation Department of Forests 2018 Technical Team Mr. Gopal Prakash Bhattarai Deputy Director General, DNPWC Mr. Laxman Prasad Poudyal Ecologist, DNPWC Mrs. Madhuri Karki (Thapa) Planning Offi cer, DoF Dr. Naresh Subedi Manager (Conservation Program), NTNC Dr. Kanchan Thapa Technical Advisor Hariyo Ban Programme-II, WWF Nepal Dr. Bhagawan Raj Dahal Transboundary Tiger Manager, ZSL Nepal Mr. Rishi Ranabhat Assistant Ecologist, DNPWC Mr. Bhupendra Yadav Assistant Ecologist, DNPWC Review Team Mr. Man Bahadur Khadka Director General, DNPWC Mr. Krishna Prasad Acharya Director General, DoF Dr. Maheshwar Dhakal Joint Secretary (Technical), MoFE Mr. Ram Chandra Kandel Deputy Director General, DNPWC Published by: Dr. Shant Raj Jnawali Department of National Parks and Wildlife Conservation Chief of Party, Hariyo Ban Programme-II, and Department of Forests WWF Nepal Kathmandu, Nepal. Copyright: Dr. Hem Sagar Baral Department of National Parks and Wildlife Conservation Country Representative, ZSL Nepal and Department of Forests (2018) Prof. Karan Bahadur Shah Citation: Herpetofauna Expert DNPWC and DoF. 2018. Pangolin Conservation Action Plan for Nepal (2018-2022) Department of National Parks and Wildlife -

NACA 2021 Conference
NACA 2021 INAUGURAL CONFERENCE April 16 and 17, 2021 (10:00 AM - 01:30 PM EST) PRELIMINARY PROGRAM (LAST UPDATED April 10, 12pm EST) DAY 1 - APRIL 16 (FRIDAY) Times are in EST 10:00 - 10:45 OPENING SESSION WELCOME REMARKS, Udaya Wagle (President, NACA) KEYNOTE SPEECH, Amir Sapkota (University of Maryland), Emerging Knowledge on Climate Change: Responding to Threats and Opportunities Zoom link: (register to get the link) BREAK (5 MINUTES) 10:50 - 11:35 CONCURRENT PANEL SESSIONS PL16-01, HIGHER EDUCATION POLICIES AND PRACTICES Organizer: Udaya Wagle (Western Michigan University) Moderator: Brijesh Thapa (Oklahoma State University) Zoom link: (registrants only) Panelists: Udaya Wagle (Western Michigan University), Satis Devkota (University of Minnesota Morris), Amina Singh (Kathmandu University), Kapil Dev Regmi (University of British Columbia) PL16-02, SCIENTIFIC FOREST MANAGEMENT IN NEPAL: CONTEMPORARY ISSUES AND PATHS FORWARD ` Organizer/Moderator: Rajan Parajuli (North Carolina State University) Zoom link: (registrants only) Panelists: Dinesh Paudel (Appalachian State University), Suman Bhattarai (Institute of Forestry, Tribhuvan University), Dil Bahadur Khatri (South Asia Institute of Advanced Studies, Nepal), Omkar Joshi (Oklahoma State University) BREAK (5 MINUTES) 11:40 - 12:30 CONCURRENT PAPER PRESENTATIONS PR16-01, DISASTER RISKS IN THE HIMALAYA Organizer/Moderator: Milan Shrestha (Arizona State University) Zoom link: (registrants only) Presenters: Nitesh Khadka (Chinese Academy of Sciences) The Status of Glacial Lakes, GLOF Risk -

Nepalese Translation Volume 1, September 2017 Nepalese Translation
Nepalese Translation Volume 1, September 2017 Nepalese Translation Volume 1,September2017 Volume cg'jfbs ;dfh g]kfn Society of Translators Nepal Nepalese Translation Volume 1 September 2017 Editors Basanta Thapa Bal Ram Adhikari Office bearers for 2016-2018 President Victor Pradhan Vice-president Bal Ram Adhikari General Secretary Bhim Narayan Regmi Secretary Prem Prasad Poudel Treasurer Karuna Nepal Member Shekhar Kharel Member Richa Sharma Member Bimal Khanal Member Sakun Kumar Joshi Immediate Past President Basanta Thapa Editors Basanta Thapa Bal Ram Adhikari Nepalese Translation is a journal published by Society of Translators Nepal (STN). STN publishes peer reviewed articles related to the scientific study on translation, especially from Nepal. The views expressed therein are not necessarily shared by the committee on publications. Published by: Society of Translators Nepal Kamalpokhari, Kathmandu Nepal Copies: 300 © Society of Translators Nepal ISSN: 2594-3200 Price: NC 250/- (Nepal) US$ 5/- EDITORIAL strategies the practitioners have followed to Translation is an everyday phenomenon in the overcome them. The authors are on the way to multilingual land of Nepal, where as many as 123 theorizing the practice. Nepali translation is languages are found to be in use. It is through desperately waiting for such articles so that translation, in its multifarious guises, that people diverse translation experiences can be adequately speaking different languages and their literatures theorized. The survey-based articles present a are connected. Historically, translation in general bird's eye view of translation tradition in the is as old as the Nepali language itself and older languages such as Nepali and Tamang. than its literature. -

2076BS Yogmaya: Historical Reality in the Fictiona
JODEM: Journal of Language and Literature, vol. 10, no. 1, issue 12, 2019/ 2076BS 1 Yogmaya: Historical Reality in the Fictional Existence Anupa Wagle Abstract The aim of this article is to analyze the novel Yogmaya to find out the balance between the fictional world presented in it and the history related to it. Written as a novel on the background of Rana Period in Nepal, my endeavour is to find out whether the novel is successful to portray the contemporary Nepalese society. In order to analyze the novel this study draws insight from new historicism that demands the equal weight for literary foreground and historical background. For this, the study is limited within some aspects of New Historical approach and fictional world related to social phenomena presented in the novel. Finally, this article includes the major finding of this study that the fictional foregrounding of the novel successfully portrays the contemporary social background of the concerned time and place. Free translation is used while citing texts from the novel since it is in Nepali. Keywords: Realism, historicism, new historicism, evil customs, women movement. Yogmaya and the Nepalese History: An Introduction In the history of Nepal, Rana Regime is known as Dark Age as it lacked freedom, public sovereignty, and public literacy. It started from the rule of Jung Bahadur Rana in 1903 BS causing 'Kot Parwa' [Kot Massacre] to happen. From then Rana regime continued for 104 years. Many people sacrificed their lives while they revolted against that ruling system. Our history always remembers the contribution of four martyrs who belong to that age.