Evaluation and Management of Neurogenic Bladder: What Is New in China?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Anatomical Study of the Superior Cluneal Nerve and Its Estimation of Prevalence As a Cause of Lower Back Pain in a South African Population
Anatomical study of the superior cluneal nerve and its estimation of prevalence as a cause of lower back pain in a South African population by Leigh-Anne Loubser (10150804) Dissertation to be submitted in full fulfilment of the requirements for the degree Master of Science in Anatomy In the Faculty of Health Science University of Pretoria Supervisor: Prof AN Van Schoor1 Co-supervisor: Dr RP Raath2 1 Department of Anatomy, University of Pretoria 2 Netcare Jakaranda Hospital, Pretoria 2017 DECLARATION OF ORIGINALITY UNIVERSITY OF PRETORIA The Department of Anatomy places great emphasis upon integrity and ethical conduct in the preparation of all written work submitted for academic evaluation. While academic staff teach you about referencing techniques and how to avoid plagiarism, you too have a responsibility in this regard. If you are at any stage uncertain as to what is required, you should speak to your lecturer before any written work is submitted. You are guilty of plagiarism if you copy something from another author’s work (e.g. a book, an article, or a website) without acknowledging the source and pass it off as your own. In effect, you are stealing something that belongs to someone else. This is not only the case when you copy work word-for-word (verbatim), but also when you submit someone else’s work in a slightly altered form (paraphrase) or use a line of argument without acknowledging it. You are not allowed to use work previously produced by another student. You are also not allowed to let anybody copy your work with the intention of passing if off as his/her work. -
Curative Efficacy of Low Frequency Electrical Stimulation in Preventing
Li et al. World Journal of Surgical Oncology (2019) 17:141 https://doi.org/10.1186/s12957-019-1689-2 RESEARCH Open Access Curative efficacy of low frequency electrical stimulation in preventing urinary retention after cervical cancer operation Huan Li1,2†, Can-Kun Zhou4†, Jing Song1,2, Wei-Ying Zhang1,2, Su-Mei Wang1,2, Yi-Ling Gu1,2, Kang Wang1,2, Zhe Ma1,2, Yan Hu1,2, Ai-Min Xiao1,2, Jian-Liu Wang3 and Rui-Fang Wu1,2* Abstract Background: To evaluate the clinical significance of low-frequency electrical stimulation in preventing urinary retention after radical hysterectomy. Methods: A total of 91 women with stage IA2–IB2 cervical cancer, who were treated with radical hysterectomy and lymphadenectomy from January 2009 to December 2012, were enrolled into this study and were randomly divided into two groups: trail group (48 cases) and control group (43 cases). Traditional bladder function training and low- frequency electrical stimulation were conducted in the trail group, while patients in the control group were only treated by traditional bladder training. The general condition, rate of urinary retention, and muscle strength grades of pelvic floor muscle in the perioperative period were compared between these two groups. Results: The incidence of postoperative urinary retention in the electrical stimulation group was 10.41%, significantly lower than that in the control group (44.18%), and the difference was statistically significant (P < 0.01). The duration of postoperative fever and use of antibiotics were almost the same between these two groups. Eleven days after surgery, the difference in grades of the pelvic floor muscle between these two groups was not statistically significant. -

Overview of Spinal Nerves
Spinal Nerves Boundless Overview of Spinal Nerves Spinal nerves, a part of the PNS, generally refers to mixed nerves, with motor, sensory, and autonomic signals between the CNS and the body. 1. fig. 1 shows a spinal nerve Spinal nerves arise from a combination of nerve fibers: the dorsal and ventral roots of the spinal cord. Afferent sensory axons, bringing sensory information from the body to the spinal cord and brain, travel through the dorsal roots of the spinal cord, and efferent motor axons, bringing motor information from the brain to the body, travel through the ventral roots of the spinal cord. All spinal nerves except the first pair emerge from the spinal column through an opening between vertebrae, called an intervertebral foramen. The spinal nerves are typically labeled by their location in the body: thoracic, lumbar, or sacral. Dorsal Root: Also known as the posterior root, the afferent sensory root of a spinal nerve. Autonomic: Acting or occurring involuntarily, without conscious control. Intervertebral Foramen: The foramen allows for the passage of the spinal nerve root, dorsal root ganglion, the spinal artery of the segmental artery, communicating veins between the internal and external plexuses, recurrent meningeal (sinu- vertebral) nerves, and transforaminal ligaments. 2. Source URL: https://www.boundless.com/physiology/peripheral-nervous-system-pns/spinal-nerves/ Saylor URL: http://www.saylor.org/courses/psych402/ Attributed to: [Boundless] www.saylor.org Page 1 of 12 fig. 2 shows intervertebral foramina Intervertebral foramina are indicated by arrows. Spinal Nerves The term spinal nerve generally refers to a mixed spinal nerve, which carries motor, sensory, and autonomic signals between the spinal cord and the body. -

The Spinal Cord and Spinal Nerves
14 The Nervous System: The Spinal Cord and Spinal Nerves PowerPoint® Lecture Presentations prepared by Steven Bassett Southeast Community College Lincoln, Nebraska © 2012 Pearson Education, Inc. Introduction • The Central Nervous System (CNS) consists of: • The spinal cord • Integrates and processes information • Can function with the brain • Can function independently of the brain • The brain • Integrates and processes information • Can function with the spinal cord • Can function independently of the spinal cord © 2012 Pearson Education, Inc. Gross Anatomy of the Spinal Cord • Features of the Spinal Cord • 45 cm in length • Passes through the foramen magnum • Extends from the brain to L1 • Consists of: • Cervical region • Thoracic region • Lumbar region • Sacral region • Coccygeal region © 2012 Pearson Education, Inc. Gross Anatomy of the Spinal Cord • Features of the Spinal Cord • Consists of (continued): • Cervical enlargement • Lumbosacral enlargement • Conus medullaris • Cauda equina • Filum terminale: becomes a component of the coccygeal ligament • Posterior and anterior median sulci © 2012 Pearson Education, Inc. Figure 14.1a Gross Anatomy of the Spinal Cord C1 C2 Cervical spinal C3 nerves C4 C5 C 6 Cervical C 7 enlargement C8 T1 T2 T3 T4 T5 T6 T7 Thoracic T8 spinal Posterior nerves T9 median sulcus T10 Lumbosacral T11 enlargement T12 L Conus 1 medullaris L2 Lumbar L3 Inferior spinal tip of nerves spinal cord L4 Cauda equina L5 S1 Sacral spinal S nerves 2 S3 S4 S5 Coccygeal Filum terminale nerve (Co1) (in coccygeal ligament) Superficial anatomy and orientation of the adult spinal cord. The numbers to the left identify the spinal nerves and indicate where the nerve roots leave the vertebral canal. -

Clinical Policy: Injections and Radiofrequency Neurotomy for Pain Management Reference Number: CP.MP.118 Coding Implications Last Review Date: 04/18 Revision Log
Clinical Policy: Injections and Radiofrequency Neurotomy for Pain Management Reference Number: CP.MP.118 Coding Implications Last Review Date: 04/18 Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Invasive pain management procedures considered in this policy include epidural steroid injections/selective nerve root blocks, facet joint diagnostic and therapeutic blocks and radiofrequency ablation, sacroiliac joint injections and radiofrequency ablation, intradiscal steroid injections, trigger point injections, occipital nerve blocks, peripheral nerve blocks and sympathetic blocks. Policy/Criteria It is the policy of health plans affiliated with Centene Corporation® that invasive pain management procedures performed by a physician are medically necessary when the relevant criteria are met and the patient receives only one procedure per visit, with or without radiographic guidance. I. Caudal or Interlaminar Epidural Steroid Injections .............................................................1 II. Selective Nerve Root Blocks ...............................................................................................2 III. Transforaminal Epidural Steroid Injections .........................................................................3 IV. SNRB/TFESI for Acute Pain Management .........................................................................4 V. Facet Joint Interventions ......................................................................................................4 -

Redalyc.Topographic Anatomy of the Spinal Cord and Vertebromedullary
Acta Scientiarum. Biological Sciences ISSN: 1679-9283 [email protected] Universidade Estadual de Maringá Brasil Campos Lima, Fabiano; Quagliatto Santos, André Luiz; Carvalho Lima, Betania; Gonçalves Vieira, Lucélia; Queiroz Luz Hirano, Líria Topographic anatomy of the spinal cord and vertebromedullary relationships in Mazama gouazoubira Fisher, 1814 (Artiodactyla; Cervidae) Acta Scientiarum. Biological Sciences, vol. 32, núm. 2, 2010, pp. 189-194 Universidade Estadual de Maringá .png, Brasil Available in: http://www.redalyc.org/articulo.oa?id=187114387013 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative DOI: 10.4025/actascibiolsci.v32i2.5061 Topographic anatomy of the spinal cord and vertebromedullary relationships in Mazama gouazoubira Fisher, 1814 (Artiodactyla; Cervidae) Fabiano Campos Lima, André Luiz Quagliatto Santos*, Betania Carvalho Lima, Lucélia Gonçalves Vieira and Líria Queiroz Luz Hirano Laboratório de Pesquisa em Animais Silvestres, Faculdade de Medicina Veterinária, Universidade Federal de Uberlândia, Av. Amazonas, 2245, 38405-302, Jardim Umuarama, Uberlândia, Minas Gerais, Brazil, *Author for correspondence. E-mail: [email protected] ABTRACT. To gain an understanding of the detailed anatomical aspects of Mazama gouazoubira (brocket deer), this paper describes the relationships between its spinal cord and the vertebral canal, adding information with a clinical and surgical approach. Three specimens of M. gouazoubira were prepared following the methods normally used in anatomy. The epaxial muscles and vertebral arches were removed to expose the spinal cord and the spinal nerve roots. The dimensions of the medullary segments were measured using a pachymeter with 0.05 mm precision. -

In Shortly About Cauda Equina Syndrome Siniša Franjić*
Archives of Neurology and Neuro Disorders ISSN: 2638-504X Volume 3, Issue 1, 2020, PP: 21-26 In Shortly about Cauda Equina Syndrome Siniša Franjić* [email protected] Faculty of Law, International University of Brcko District, Brcko, Bosnia and Herzegovina. *Corresponding Author: Siniša Franjić, Faculty of Law, International University of Brcko District, Brcko, Bosnia and Herzegovina. Abstract Cauda equina syndrome affects a group of nerve roots called Cauda equina (in latin “horse tail“). These nerves are located at the lower end of the spine in the lumbosacral part. They send and receive messages for the legs, feet and pelvis. Trauma, overexertion, violent injuries, and some diseases and conditions result in compression of the roots of these nerves. There is severe lower back pain, loss or change of sensation in the legs, buttocks, difficulty in urinating. Surgical treatment must be performed quickly to prevent permanent damage, such as leg paralysis, bladder and bowel dysfunction, sexual function, or other problems. Keywords: Cauda equina, Spinal cord, Pathology, Treatment Introduction CES is a neurosurgical emergency. The goal is to prevent irreversible loss of bowel and bladder function Cauda equina syndrome (CES). The signs and and motor function of the lower extremities. While symptoms of lower extremity weakness and pain developing acutely after heavy lifting should raise CES is primarily a clinical diagnosis, further imaging suspicion for a herniated intervertebral disc, which will be required to aid decision-making and operative is the commonest cause of CES [1]. Depending on the planning. Ultimately, an MRI of the lumbar spine will location and degree of the herniation, a combination help guide the neurosurgeon. -

ESMO–Paedcan–EURACAN Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up†
Annals of Oncology 29 (Supplement 4): iv79–iv95, 2018 doi:10.1093/annonc/mdy310 CLINICAL PRACTICE GUIDELINES Downloaded from https://academic.oup.com/annonc/article-abstract/29/Supplement_4/iv79/5115250 by Università degli Studi di Milano user on 29 May 2019 Bone sarcomas: ESMO–PaedCan–EURACAN Clinical Practice Guidelines for diagnosis, treatment and follow-up† P. G. Casali‡1, S. Bielack‡2, N. Abecassis3, H.T. Aro4, S. Bauer5, R. Biagini6, S. Bonvalot7, I. Boukovinas8, J. V. M. G. Bovee9, B. Brennan10, T. Brodowicz11, J. M. Broto12, L. Brugie`res13, A. Buonadonna14, E. De A´ lava15, A. P. Dei Tos16, X. G. Del Muro17, P. Dileo18, C. Dhooge19, M. Eriksson20, F. Fagioli21, A. Fedenko22, V. Ferraresi6, A. Ferrari23, S. Ferrari24, A. M. Frezza25, N. Gaspar13, S. Gasperoni26, H. Gelderblom27, T. Gil28, G. Grignani29, A. Gronchi1, R. L. Haas30, B. Hassan31, S. Hecker-Nolting2, P. Hohenberger32, R. Issels33, H. Joensuu34, R. L. Jones35, I. Judson36, P. Jutte37, S. Kaal38, L. Kager39, B. Kasper32, K. Kopeckova40, D. A. Kra´korova´41, R. Ladenstein39, A. Le Cesne13, I. Lugowska42, O. Merimsky43, M. Montemurro44, B. Morland45, M. A. Pantaleo46, R. Piana21, P. Picci24, S. Piperno-Neumann7, A. L. Pousa47, P. Reichardt48, M. H. Robinson49, P. Rutkowski42, A. A. Safwat50, P. Scho¨ffski51, S. Sleijfer52, S. Stacchiotti25, S. J. Strauss18, K. Sundby Hall53, M. Unk54, F. Van Coevorden55, W.T.A. van der Graaf35,38,55, J. Whelan18, E. Wardelmann56, O. Zaikova57 & J. Y. Blay58, on behalf of the ESMO Guidelines Committee, PaedCan and ERN EURACAN* 1Fondazione -

Neurological Examination in Spinal Cord Injury Author: Ricardo Botelho, MD Editor in Chief: Dr Néstor Fiore Senior Editor: José A
CONTINUOUS LEARNING LIBRARY Trauma Pathology Neurological Examination in Spinal Cord Injury Author: Ricardo Botelho, MD Editor In Chief: Dr Néstor Fiore Senior Editor: José A. C. Guimarães Consciência OBJECTIVES CONTINUOUS LEARNING LIBRARY Trauma Pathology Neurological examination in spinal cord injury ■■ To describe a normal neurological examination, as well as the possible abnormalities. ■■ To identify the dermatome and myotome distribution patterns. ■■ To highlight the difficulties of the neurological evaluation in unconscious patients. ■■ To recognize the international scales applied for neurological evaluations. Neurological Examination in Spinal Cord Injury. Author: Ricardo Botelho, MD 2 CONTENTS 1. Introduction Overview ........................................................................................................................................04 2. Classification .......................................................................................................06 3. Standardized neurological clinical examination (ASIA) Sensory evaluation (ASIA) ....................................................................................................... 07 Motor evaluation (ASIA)............................................................................................................10 Neurological examination (ASIA) .......................................................................................... 14 4. Examining an unconscious patient ................................ 16 References .......................................................................................................................17 -
International Standards for Neurological and Functional Classi®Cation of Spinal Cord Injury
Spinal Cord (1997) 35, 266 ± 274 1997 International Medical Society of Paraplegia All rights reserved 1362 ± 4393/97 $12.00 International Standards for Neurological and Functional Classi®cation of Spinal Cord Injury Frederick M Maynard, Jr, Michael B Bracken, Graham Creasey, John F Ditunno, Jr, William H Donovan, Thomas B Ducker, Susan L Garber, Ralph J Marino, Samuel L Stover, Charles H Tator, Robert L Waters, Jack E Wilberger and Wise Young American Spinal Injury Association, 2020 Peachtree Road, NW Atlanta Georgia 30309, USA The ®rst edition of the International Standards for ASIA Board has established a standing committee Neurological and Functional Classi®cation of Spinal to reevaluate regularly the need for further Cord Injury, ie neural disturbances (`Spinal Cord modi®cations in the Standards booklet and in the Injury') whether from trauma or disease, was Training Package, as well as to respond to published in 19826 by the American Spinal Injury questions and criticisms of the Standards from Association (ASIA). Reference was made to the 1992 the many users. This committee welcomes corre- Revision of the International Standards and published spondence that raises questions, oers constructive in Paraplegia (the former title of Spinal Cord) in 1994, criticism or provides new empirical data that is Volume 32, pages 70 ± 80 by JF Ditunno Jr, W Young, relevant for further re®nements and improvements WH Donovan and G Creasey7. Since then there have in the reliability and validity of the ISCSCI. been three revisions, the most recent being -
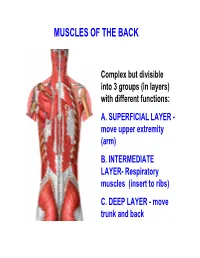
Muscles of the Back
MUSCLES OF THE BACK Complex but divisible into 3 groups (in layers) with different functions: A. SUPERFICIAL LAYER - move upper extremity (arm) B. INTERMEDIATE LAYER- Respiratory muscles (insert to ribs) C. DEEP LAYER - move trunk and back MUSCLES OF THE BACK - layered and multifunctional Vertebrae - almost all take origin from Upper vertebrae Extremity (arm) IN LAB: ORIENT TO SKELETON 1) Vertebra in midline 2) Ribs attach to vertebrae (thorax) - ribs move in respiration 3) Upper extremity (arm) - mostly Ribs free to move; attach to vertebrae by muscles SUPERFICIAL GROUP- origin VERTEBRAE; insert scapula, clavicle, humerus VERTEBRAE CLAVICLE SUPERFICIAL GROUP- insert to bones of upper extremity 1) CLAVICLE- only bony attachment of upper extremity to rest of skeleton SCAPULA 2) SCAPULA- shoulder blade 3) HUMERUS- arm attaches to scapula, if move scapula, move arm Functions- specialized for freedom of movement 1. TRAPEZIUS – Origin: 1) Skull - External occipital protuberance 2) Fascia - Ligamentum nuchae 3) Vertebrae - spines of C7, T1-T12 Insert: 1) Clavicle - lateral 1/3; 2) Scapula - acromion and spine Actions: 1) Elevates (upper fibers) and Depresses (lower fibers) Shoulder 2) Retracts scapula 3) Extends head Innervation: Accessory nerve (Cranial nerve XI) 2. LATISSIMUS DORSI Origin: Vertebrae T6-T12 (spines) Fascia- Thoracolumbar fascia Pelvic Bone- Iliac crest; Insertion: Humerus- Intertubercular (bicipital) groove Actions: Adducts, extends, and medially rotates arm Innervation: Thoracodorsal nerve Latissimus = broad, wide in Latin THORACOLUMBAR (LUMBAR) FASCIA – covers deep muscles of back - attaches medially to spines of vertebrae - inferiorly to ilium (pelvic bone) Provides for muscle attachments 3. LEVATOR SCAPULAE Origin: Vertebrae (C1-C4 transverse processes) Insertion: Scapula (sup. -

Dermatomes Anatomy Overview the Surface of the Skin Is Divided Into
Dermatomes Anatomy Overview The surface of the skin is divided into specific areas called dermatomes, which are derived from the cells of a somite. These cells differentiate into the following 3 regions: (1) myotome, which forms some of the skeletal muscle; (2) dermatome, which forms the connective tissues, including the dermis; and (3) sclerotome, which gives rise to the vertebrae. A dermatome is an area of skin in which sensory nerves derive from a single spinal nerve root (see the following image). Dermatomes of the head, face, and neck. There are 31 segments of the spinal cord, each with a pair (right and left) of ventral (anterior) and dorsal (posterior) nerve roots that innervate motor and sensory function, respectively. The anterior and posterior nerve roots combine on each side to form the spinal nerves as they exit the vertebral canal through the intervertebral foramina or neuroforamina. The 31 spine segments on each side give rise to 31 spinal nerves, which are composed of 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal spinal nerve. Dermatomes exist for each of these spinal nerves, except the first cervical spinal nerve. Sensory information from a specific dermatome is transmitted by the sensory nerve fibers to the spinal nerve of a specific segment of the spinal cord. The C1-C7 nerve roots emerge above their respective vertebrae; the C8 nerve root emerges between the C7 and T1 vertebrae . The remaining nerve roots emerge below their respective vertebrae. Along the thorax and abdomen, the dermatomes are evenly spaced segments stacked up on top of each other, and each is supplied by a different spinal nerve.