388 April 2016 1.5 CE Credits $9
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Absorbable Surgical Gut Suture
Food and Drug Administration, HHS § 878.4840 § 878.4800 Manual surgical instrument in subpart E of part 807 of this chapter, for general use. subject to the limitations in § 878.9. (a) Identification. A manual surgical [53 FR 23872, June 24, 1988, as amended at 61 instrument for general use is a non- FR 1123, Jan. 16, 1996; 66 FR 38803, July 25, powered, hand-held, or hand-manipu- 2001] lated device, either reusable or dispos- able, intended to be used in various § 878.4820 Surgical instrument motors general surgical procedures. The device and accessories/attachments. includes the applicator, clip applier, bi- (a) Identification. Surgical instrument opsy brush, manual dermabrasion motors and accessories are AC-pow- brush, scrub brush, cannula, ligature ered, battery-powered, or air-powered carrier, chisel, clamp, contractor, cu- devices intended for use during surgical rette, cutter, dissector, elevator, skin procedures to provide power to operate graft expander, file, forceps, gouge, in- various accessories or attachments to strument guide, needle guide, hammer, cut hard tissue or bone and soft tissue. hemostat, amputation hook, ligature Accessories or attachments may in- passing and knot-tying instrument, clude a bur, chisel (osteotome), knife, blood lancet, mallet, disposable dermabrasion brush, dermatome, drill or reusable aspiration and injection bit, hammerhead, pin driver, and saw needle, disposable or reusable suturing needle, osteotome, pliers, rasp, re- blade. tainer, retractor, saw, scalpel blade, (b) Classification. Class I (general con- scalpel handle, one-piece scalpel, snare, trols). The device is exempt from the spatula, stapler, disposable or reusable premarket notification procedures in stripper, stylet, suturing apparatus for subpart E of part 807 of this chapter the stomach and intestine, measuring subject to § 878.9. -

Oral and Maxillofacial Surgery
ORAL AND MAXILLOFACIAL SURGERY 3rd EDITION 2/2012 US Chapter Pages 1 BASIC SETS OMFS-SET 1-36 TELESCOPES AND INSTRUMENTS FOR FRAKT 37-54 2 ENDOSCOPIC FRACTURE TREATMENT TELESCOPES AND INSTRUMENTS FOR TMJ 55-60 3 ARTHROSCOPY OF TEMPOROMANDIBULAR JOINT TELESCOPES AND INSTRUMENTS FOR DENT 61-80 4 MAXILLARY ENDOSCOPY TELESCOPES AND INSTRUMENTS DENT-K 81-120 5 FOR DENTAL SURGERY TELESCOPES AND INSTRUMENTS SIAL 121-134 6 FOR SIALENDOSCOPY 7 FLEXIBLE ENDOSCOPES FL-E 135-142 8 HOSPITAL SUPPLIES HS 143-240 9 INSTRUMENTS FOR RHINOLOGY AND RHINOPLASTY N 241-298 10 BIPOLAR AND UNIPOLAR COAGULATION COA 299-312 11 HEADMIRRORS – HEADLIGHTS OMFS-J 313-324 12 AUTOFLUORESCENCE AF-INTRO, AF 325-342 13 HOLDING SYSTEMS HT 343-356 VISUALIZATION SYSTEMS OMFS-MICRO, OMFS-VITOM 357-378 14 FOR MICROSURGERY OMFS-UNITS-INTRO, UNITS AND ACCESSORIES U 1-54 15 OMFS-UNITS COMPONENTS OMFS-SP SP 1-58 16 SPARE PARTS KARL STORZ OR1 NEO™, TELEPRESENCE 17 HYGIENE, ENDOPROTECT1 ORAL AND MAXILLOFACIAL SURGERY 3rd EDITION 2/2012 US Important information for U.S. customers Note: Certain devices and references made herein to specific indications of use may have not received clearance or ap- proval by the United States Food and Drug Administration. Practitioners in the United States should first consult with their local KARL STORZ representative in order to ascertain product availability and specific labeling claims. Federal (USA) law restricts certain devices referenced herein to sale, distribution, and use by, or on the order of a physician, dentist, veterinarian, or other practitioner licensed by the law of the State in which she/he practices to use or order the use of the device. -

CPT Code Description Charge Amount 83498 17-Alpha
CPT Code Description Charge Amount 83498 17-alpha-Hydroxyprogester 308.41 83497 5-HIAA, SO 125.99 83516 A MYELOPEROX (MPO) AB QL 74.1 86021 AB ID LEUKOCYTE AB/SO 610.25 86022 AB ID, PLATELET ABS;SRA U 1318 86720 AB LEPTOSPIRA/SO 166.12 86850 AB SCREEN (IDC) 207.83 86850 AB SCREEN RBC EA SRM TECH 195.25 86793 AB, YERSINIA/SO 149 74018 ABDOMEN 1 VIEW 348.75 74018 ABDOMEN 1 VIEW PORTABLE 321.36 74022 ABDOMEN ACUTE COMP WSGL V 398.36 74019 ABDOMEN COMPLETE 398.36 74018 ABDOMEN SGL ANTEROPOSTERI 475.8 49083 ABDOMINAL PARACENTESIS W/ 1216.89 86870 ABID,WNJ 294.85 ABLATOR APOLLORF XL90 ASP 877.8 86900 ABO BLOOD TYPE 370 86900 ABO,BBSO 176.5 73050 AC JOINTS W/WO WEIGHTS BI 297.94 ACCUGRID RADIOGRAPH BREAS 121.36 82164 ACE, CSF SO 144.38 83519 ACHR BIND AB QT,RIA/SO MA 258 83519 ACHR BIND QNT MGP/SO 181.37 83519 ACHR BLOC QNT MGP/SO 181.37 83519 ACHR GANGL NEUR AB,RIA/SO 258 83519 ACHR MOD QNT MGP/SO 201.16 87116 ACID FAST CULTURE SO 227.33 83519 ACR BLOCKING QNT SO 181.37 83519 ACR RECEPTOR QNT SO 108.61 82024 ACTH,SO 459.3 86602 ACTINOMYCES AB/SO 64 85347 ACTIVATED CLOTTING TIME 126.93 85307 Activated Protein C Resis 216.04 97535GO ACTIVITY DAILY LIVING 15 265.91 78278 ACUTE GI BLOOD LOSS IMAGI 1326.15 82017 ACYLCARNITINES; QUANT, EA 574 85397 ADAMSTS 13 ACTIVITY/SO 796.62 ADAPTER CATH LUER 8.69 ADAPTER CONFIDENCE CEMENT 743.66 ADAPTER DLP PERFUS Y W/6 47.54 ADAPTER FIBEROPTIC SWIVEL 73.16 ADAPTER LUER LOC SHORT 3/ 2.2 ADAPTER LUER TO COLDER 15.29 ADAPTER MALE-MALE 4.57 C1776 ADAPTER PFC SIGMA FEMORAL 8474.76 ADAPTER PLUG MALE CLAVE 5.02 ADAPTER PRODIGY EXTENSION 2340 ADAPTER UROSTOMY DRAIN TU 9.09 ADAPTER VERSO AIRWAY ADUL 33.51 82952 ADDL GLUCOSE > 3 SPEC 136.24 87260 ADENOV/ RSPFAC / SO 141.75 ADHESIVE DEMABOND .07 PEN 193.48 ADHESIVE DEMABOND .07 PEN 193.48 ADHESIVE DERMABOND PEN 0. -

Hospitals for War-Wounded
hospitals_war_cover_april2003 9.6.2005 13:47 Page 1 ICRC HOSPITALS FOR WAR-WOUNDED HOSPITALS FORHOSPITALS WAR-WOUNDED This book is intended for anyone who is faced A practical guide for setting up with the task of setting up or running a hospital and running a surgical hospital which admits war-wounded. It is a practical guide in an area of armed conflict based on the experience of four nurses who have managed independent hospitals set up by the International Committee of the Red Cross. It addresses specific problems associated with setting up a hospital in a difficult and potentially dangerous environment. It provides a framework for the administration of such a hospital. It also describes a system for managing the patients from admission to discharge and includes guidelines on how to manage an influx of wounded. These guidelines represent a realistic and achievable standard of care whatever the circumstances. A practical guide 0714/002 05/2005 1000 HOSPITALS FOR WAR-WOUNDED International Committee of the Red Cross 19 Avenue de la Paix 1202 Geneva, Switzerland T +41 22 734 6001 F +41 22 733 2057 E-mail: [email protected] www.icrc.org # ICRC, April 2005, revised and updated edition This book is dedicated to the memory of Jo´n Karlsson (died in Afghanistan, 22 April 1992) Fernanda Calado Hans Elkerbout Ingebjørg Foss Nancy Malloy Gunnhild Myklebust Sheryl Thayer (died in Chechnya, 17 December 1996) HOSPITALS FOR WAR-WOUNDED A practical guide for setting up and running a surgical hospital in an area of armed conflict Jenny Hayward-Karlsson Sue Jeffery Ann Kerr Holger Schmidt INTERNATIONAL COMMITTEE OF THE RED CROSS ISBN 2-88145-094-6 # International Committee of the Red Cross, Geneva, 1998 WEB address: http://www.icrc.org CONTENTS vii CONTENTS FOREWORD ............................................ -
Corrigendum for Open Surgical Instruments for the Department Of
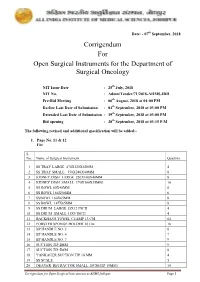
Date: - 07th September, 2018 Corrigendum For Open Surgical Instruments for the Department of Surgical Oncology NIT Issue Date : 25th July, 2018 NIT No. : Admn/Tender/71/2018-AIIMS.JDH Pre-Bid Meeting : 06th August, 2018 at 04:00 PM Earlier Last Date of Submission : 04th September, 2018 at 03:00 PM Extended Last Date of Submission : 19th September, 2018 at 03:00 PM Bid opening : 20th September, 2018 at 03:15 P.M The following revised and additional specification will be added:- 1. Page No. 11 & 12 For S. No. Name of Surgical Instrument Quantity 1 SS TRAY LARGE 470X320X50MM 4 2 SS TRAY SMALL 350X240X40MM 8 3 KIDNEY DISH LARGE 250X140X40MM 8 4 KIDNEY DISH SMALL 170X100X35MM 10 5 SS BOWL 80X40MM 6 6 SS BOWL 166X50MM 6 7 SSBOWL 160X65MM 8 8 SS BOWL 147X65MM 8 9 SS DRUM LARGE 15X12 INCH 4 10 SS DRUM SMALL 11X9 INCH 4 11 BACKHAUS TOWEL CLAMP 13 CM 64 12 FORSTER SPONGE HOLDER 18 Cm 18 13 BP HANDLE NO. 3 8 14 BP HANDLE NO. 4 7 15 BP HANDLE NO. 7 9 16 SUCTION TIP 2MM 9 17 SUCTION TIP 5MM 8 18 YANKAUER SUCTION TIP 10 MM 4 19 SS SCALE 5 20 DEAVER RETRACTOR SMALL 18CM(TIP 19MM) 14 Corrigendum for Open Surgical Instruments at AIIMS Jodhpur Page 1 21 DEAVER RETRACTOR MEDIUM 30.5CM (TIP 25 MM) 10 22 DEAVER RETRACTOR LARGE 31.5CM (TIP 50MM) 10 23 DOYEN’S RETRACTOR 4 24 MORRIS RETRACTOR 25cm ( BLADE 7x4cm) 6 25 SKIN HOOK 32 26 LANGENBECK RETRACTOR SMALL 16cm (TIP 21x 8mm) 16 27 LANGENBECK RETRACTOR MEDIUM 22cm (TIP 50x11mm) 16 28 LANGENBECK RETRACTOR LARGE 22.5cm (TIP 85x15mm) 14 29 C ZERNY RETRACTOR 17.2 cm 14 30 VEIN RETRACTOR 18 31 BALFOUR ABDOMINAL RETRACTOR 20cm 3 32 MASTOID RETRACTOR 4 33 PERIOSTEUM ELEVATOR SHARP 4 34 PERIOSTEUM ELEVATOR BLUNT 4 35 DISSECTING TOOTH FORCEPS 15 CM 16 36 DISSECTING PLAIN FORCEPS 18 CM 16 37 ARTERY FORCEPS CVD 15 CM 36 38 ARTERY FORCEPS ST. -

Healthcare Product Description Guideline
Canadian Healthcare Product Description Standardization Implementation Guidelines Version: 1.1 Updated: 2018 March Canadian Healthcare Product Description Standardization Implementation Guidelines Document Summary Document Item Current Value Document Name Canadian Healthcare Product Description Standardization Implementation Guidelines Document Version 1.1 Document Status Initial Publication December, 2010 Update formatting and appendix June 2016 Errata in abbreviation list “Universal” March 2018 Document Status FINAL Document Description Supplements the formal GS1 Canada Healthcare Supply Chain Guidelines January 2010 Version 1.0 providing information on the standardization of the short product description for the healthcare supply chain in Canada. Content Developers Organization Name 3M Canada Company Content Developer Ruth Wisotzki 3M Canada Company Content Developer Marilyn Piper HealthPRO Procurement Services Content Developer Ronda Harris HealthPRO Procurement Services Content Developer Tricia Cooper Medtronic Canada Inc. Content Developer Alain Boutin North Bay General Hospital Content Developer Lise Morris North York General Hospital Content Developer Marty McKinlay Ontario Hospital Association (OHA) Content Developer Peter Roman Source Medical Content Developer Anne Griffin Source Medical Content Developer Phil Kelly St. Michael’s Hospital Content Developer Diane Eley Toronto General Hospital (UHN) Content Developer Maria Masella Toronto General Hospital (UHN) Content Developer Wendy Watson Toronto Western Hospital (UHN) Content -

Evolution of Instruments for Harvest of the Skin Grafts Original Article
Original Article Evolution of instruments for harvest of the skin grafts Faisal Ameer, Arun Kumar Singh1, Sandeep Kumar2 Department of Plastic Surgery, Lala Lajpat Rai Memorial Medical College, Meerut, 1Department of Plastic Surgery, King George’s Medical University, Lucknow, UP, India. 2All Indian Institute of Medical Sciences Saket Nagar, Bhopal, Madhya Pradesh, India Address for correspondence: Dr. Faisal Ameer, L-20, Lala Lajpat Rai Memorial Medical College Campus, Meerut - 250 004, UP, India. E-mail: [email protected] ABSTRACT Background: The harvest of autologous skin graft is considered to be a fundamental skill of the plastic surgeon. The objective of this article is to provide an interesting account of the development of skin grafting instruments as we use them today in various plastic surgical procedures. Materials and Methods: The authors present the chronological evolution and modifications of the skin grafting knife, including those contributions not often cited in the literature, using articles sourced from MEDLINE, ancient manuscripts, original quotes, techniques and illustrations. Results: This article traces the evolution of instrumentation for harvest of skin grafts from free hand techniques to precise modern automated methods. Conclusions: Although skin grafting is one of the basic techniques used in reconstructive surgery yet harvest of a uniform graft of desired thickness poses a challenge. This article is dedicated to innovators who have devoted their lives and work to the advancement of the field of plastic surgery. KEY WORDS Dermatomes; split-thickness skin graft; skin grafting knives INTRODUCTION a piece of skin whose thickness is controlled by a calibrated setting on the instrument or by the surgeon himself. -
Overview of Gynecologic Oncology
Overview of Gynecologic Oncology “The Blue Book” R. Kevin Reynolds, MD 11th Edition, Revised February 2010 www.med.umich.edu/obgyn/gynonc Gyn Oncology.......................................................................734-764-9106 Cancer Center Answer Line ...............................................800-865-1125 Contents Gyn Tumors Page Breast Cancer ......................................................................... 1 Cervical Cancer 6 Endometrial Cancer................................................. 17 Gestational Trophoblastic Neoplasia 24 Ovarian Cancer ....................................................... 29 Sarcomas 44 Vaginal Cancer........................................................ 51 Vulvar Cancer 53 Associated Treatment Modalities Nutrition, Fluid and Electrolytes 66 Radiation Therapy ................................................... 71 Chemotherapy 75 Perioperative Management ..................................... 94 Tools and Equipment for the Art of Surgery 108 Appendix Out-of-Date Staging Rules .................................... 123 GOG Toxicity Criteria 125 Performance Status............................................... 129 Web Resources 130 Special thanks to William Burke, MD, and to Catherine Christen, PharmD Favorite Quotes "Statistics are no substitute for judgment." Henry Clay "A leading authority is anyone who has guessed right more than once." Frank A. Clark "Well done is better than well said." Ben Franklin "Trust me. I'm a doctor" Donald H. Chamberlain, MD "To err is human; to repeat the -

A Narrative Review of the History of Skin Grafting in Burn Care
medicina Review A Narrative Review of the History of Skin Grafting in Burn Care Deepak K. Ozhathil *, Michael W. Tay, Steven E. Wolf and Ludwik K. Branski Department of Surgery, University of Texas Medical Branch at Galveston, Galveston, TX 77550, USA; [email protected] (M.W.T.); [email protected] (S.E.W.); [email protected] (L.K.B.) * Correspondence: [email protected]; Tel.: +1-508-654-8246 Abstract: Thermal injuries have been a phenomenon intertwined with the human condition since the dawn of our species. Autologous skin translocation, also known as skin grafting, has played an important role in burn wound management and has a rich history of its own. In fact, some of the oldest known medical texts describe ancient methods of skin translocation. In this article, we examine how skin grafting has evolved from its origins of necessity in the ancient world to the well-calibrated tool utilized in modern medicine. The popularity of skin grafting has ebbed and flowed multiple times throughout history, often suppressed for cultural, religious, pseudo-scientific, or anecdotal reasons. It was not until the 1800s, that skin grafting was widely accepted as a safe and effective treatment for wound management, and shortly thereafter for burn injuries. In the nineteenth and twentieth centuries skin grafting advanced considerably, accelerated by exponential medical progress and the occurrence of man-made disasters and global warfare. The introduction of surgical instruments specifically designed for skin grafting gave surgeons more control over the depth and consistency of harvested tissues, vastly improving outcomes. The invention of powered surgical instruments, such as the electric dermatome, reduced technical barriers for many surgeons, allowing the practice of skin grafting to be extended ubiquitously from a small group of technically gifted reconstructive surgeons Citation: Ozhathil, D.K.; Tay, M.W.; to nearly all interested sub-specialists. -

Sterilcontainer System Catalog
SterilContainer™ System General Catalog Aesculap Surgical Technologies — Sterile Processing Table of Contents Introduction ■ History ..................................................................................................... 4-6 ■ SterilContainer™ Design ................................................................... 7-8 SterilContainer System Containers & Baskets .................................... 9-23 ■ Full-Size .................................................................................................. 10-11 ■ Three-Quarter Size ............................................................................... 12-13 ■ Half Size .................................................................................................. 14-15 ■ Extra-Long Mini Size ........................................................................... 16 ■ Extra-Long Size ..................................................................................... 17 ■ Quarter Size ........................................................................................... 18-19 ■ Mini Size ................................................................................................. 20 ■ Wide-Body Size ..................................................................................... 21 ■ SterilContainer™ S ............................................................................... 22-23 Instrument Organization System ............................................................. 25-41 General Accessories ...................................................................................... -

Skin Graft Products Dermatomes
Skin Graft Products Dermatomes Model S Slimline Electric Dermatome Kit 1 6 5 7 8 3 2 9 10 4 Slim Design, Serious Performance No. Catalog# Description 1. 3539700 Model S Slimline Dermatome Set, Complete, Universal Power Supply, 110-230 Volts 2. DP0009 Model S Slimline Dermatome Handpiece Êp 3. 35392660 Head Assembly Guard Plate Ê 4. 35392661 1” (2.54 cm) Width Clip (Not Shown) p 35392662 2” (5.08 cm) Width Clip 35392663 3” (7.62 cm) Width Clip 35392664 4” (10.16 cm) Width Clip 5. 353971513 13’ (3.96 m) Handpiece Power Cord 353971525 25’ (7.62 m) Handpiece Power Cord (Not Shown) p 6. DP0007 Power Supply 7. 3539620 U.S. Power Supply Wall Cord (Specify Country of Use for Alternative Plugs) 8. 3539252 Sterile Dermatome Blades, Box of 10 (3 Boxes of Blades Included with Initial Order) 9. 3539259 Calibration Guide 10. 3539257 Screwdriver for Dermatome, Philips, Stainless Steel 3539240 Carrying Case, ABS plastic (Not Shown) Product Is Included in Its Complete Kit p Special Order, if ordered separately Toll-free: 800-654-2873 Phone: 609-275-0500 Fax: 609-275-5363 www.Integra-LS.com 261 Skin Graft Products Model PI Electric Dermatome Kit 1 5 6 3 7 8 9 2 4 No. Catalog# Description 1. 3539600 PADGETT Model PI Dermatome, Complete, 120 Volts 3539600230 PADGETT Model PI Dermatome, Complete, 230 Volts (Not Shown) 2. PADGETT Model PI Dermatome Handpiece and Cord 3. 35396100 Head Assembly Guard Plate 4. 35396101 1” (2.54 cm) Width Clip (Not Shown) p 35396102 2” (5.08 cm) Width Clip 35396103 3” (7.62 cm) Width Clip 35396104 4” (10.16 cm) Width Clip 35396105 5” (12.7 cm) Width Clip 35396106 6” (15.24 cm) Width Clip 5. -

Critical Procedures
chapter 26 Critical Procedures Brent R. King, MMM, MD, FAAP, FACEP, FAAEM Christopher King, MD, FACEP Wendy C. Coates, MD, FACEP Objectives Chapter Outline Demonstrate the Introduction Section 10: Emergent Intubation 1 maneuvers required Section 1: Pediatric Length-Based 10.1 Endotracheal Intubation for the basic treatment Resuscitation Tape 10.2 Rapid Sequence Intubation of ill and injured Section 2: Cervical Spine Section 11: Rescue Airway children, including Stabilization Techniques oxygen administration, Section 3: Monitoring 11.1 Supraglottic Devices monitoring, and basic 3.1 ECG Monitoring 11.1A Laryngeal Mask Airway airway maneuvers. 3.2 Impedance Pneumatography 11.1B Combitube Demonstrate 3.3 Blood Pressure Monitors 11.2 Specialized Laryngoscopes 2 orotracheal intubation 3.4 Pulse Oximetry 11.2A Fiberoptic Scopes using a manikin model. 3.5 Exhaled Carbon Dioxide 11.3 Laryngoscopes With Special Monitors Blades Demonstrate 11.3A Video Laryngoscopes Section 4: Oxygen Administration placement of an 11.3B Lighted Stylet 3 4.1 Nasal Cannula intraosseous needle 11.4 Tracheal Guides 4.2 Oxygen Masks in a manikin or other 4.3 Nonrebreathing Masks Section 12: Surgical Airway model and describe 4.4 Oxygen Hoods Techniques the landmarks for 12.1 Needle Cricothyrotomy Section 5: Suction intraosseous needle 12.2 Retrograde Intubation Section 6: Opening the Airway placement in a child. 12.3 Wire-Guided Cricothyrotomy 6.1 Chin-Lift Maneuver Describe the 12.4 Surgical Cricothyrotomy 6.2 Jaw-Thrust Maneuver indications and 12.5 Tracheostomy Management 4 Section 7: Airway Adjuncts technique for needle Section 13: Cardioversion and 7.1 Oropharyngeal Airways thoracostomy. Defibrillation 7.2 Nasopharyngeal Airways 13.1 Cardioversion and Describe indications Section 8: Bag-Mask Ventilation Defibrillation and technique for 5 Section 9: Management of Upper 13.2 Automated External pericardiocentesis.