Glans Resurfacing with Skin Graft for Penile Cancer: a Step-By-Step Video Presentation of the Technique and Review of the Literature
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Absorbable Surgical Gut Suture
Food and Drug Administration, HHS § 878.4840 § 878.4800 Manual surgical instrument in subpart E of part 807 of this chapter, for general use. subject to the limitations in § 878.9. (a) Identification. A manual surgical [53 FR 23872, June 24, 1988, as amended at 61 instrument for general use is a non- FR 1123, Jan. 16, 1996; 66 FR 38803, July 25, powered, hand-held, or hand-manipu- 2001] lated device, either reusable or dispos- able, intended to be used in various § 878.4820 Surgical instrument motors general surgical procedures. The device and accessories/attachments. includes the applicator, clip applier, bi- (a) Identification. Surgical instrument opsy brush, manual dermabrasion motors and accessories are AC-pow- brush, scrub brush, cannula, ligature ered, battery-powered, or air-powered carrier, chisel, clamp, contractor, cu- devices intended for use during surgical rette, cutter, dissector, elevator, skin procedures to provide power to operate graft expander, file, forceps, gouge, in- various accessories or attachments to strument guide, needle guide, hammer, cut hard tissue or bone and soft tissue. hemostat, amputation hook, ligature Accessories or attachments may in- passing and knot-tying instrument, clude a bur, chisel (osteotome), knife, blood lancet, mallet, disposable dermabrasion brush, dermatome, drill or reusable aspiration and injection bit, hammerhead, pin driver, and saw needle, disposable or reusable suturing needle, osteotome, pliers, rasp, re- blade. tainer, retractor, saw, scalpel blade, (b) Classification. Class I (general con- scalpel handle, one-piece scalpel, snare, trols). The device is exempt from the spatula, stapler, disposable or reusable premarket notification procedures in stripper, stylet, suturing apparatus for subpart E of part 807 of this chapter the stomach and intestine, measuring subject to § 878.9. -

Noelle La Croix Article Ophthalmic Instrumentation
1 Ophthalmic instrumentation Specialized instruments are required for delicate ocular surgery. The American Conference of Veterinary Ophthalmologists (ACVO) asserts that microsurgery of the cornea and intraocular structures should only be performed by or under the supervision of a board-certified ophthalmologist. However, there are surgeries of the ocular adnexa that can be comfortably performed by other qualified veterinarians. This article will describe the minimal instrumentation (an “eye pack”) necessary for a general practitioner to perform these procedures (Table 1). Ophthalmic instruments are typically no larger than a pen or pencil and have been designed solely for wrist or finger manipulation to maximize precision. Extraneous motions, including that of a surgeon’s elbows or shoulders, decrease surgical accuracy. To further limit sway, ophthalmic surgeons tend to remain seated with their forearms resting upon their operating table. Magnifying surgical loupes and brightly-lit surgical fields are also required for most procedures. Surgical eye pack forceps are used to manipulate adnexal tissues (eyelids, blood vessels and conjunctiva) and to grasp cilia and foreign bodies with precision (Figure 1). For adnexal manipulation serrated instruments, such as Brown-Adson tissue forceps, are used to grasp palpebrae and membrana nictitans. Desmarres Chalazion forceps can be used to hold adnexa in place while providing hemostatis. Bishop Harman iris forceps are ideal for manipulation of the conjunctiva, and Hartman Mosquito forceps can be used for hemostatis. Smooth-tipped instruments, such as Jeweler’s forceps or Barraquer cilia forceps, are ideal for grasping cilia or foreign bodies. Surgical eye packs also include instruments to cut and/or separate ocular adnexa without significant tissue damage (Figure 2). -

Oral and Maxillofacial Surgery
ORAL AND MAXILLOFACIAL SURGERY 3rd EDITION 2/2012 US Chapter Pages 1 BASIC SETS OMFS-SET 1-36 TELESCOPES AND INSTRUMENTS FOR FRAKT 37-54 2 ENDOSCOPIC FRACTURE TREATMENT TELESCOPES AND INSTRUMENTS FOR TMJ 55-60 3 ARTHROSCOPY OF TEMPOROMANDIBULAR JOINT TELESCOPES AND INSTRUMENTS FOR DENT 61-80 4 MAXILLARY ENDOSCOPY TELESCOPES AND INSTRUMENTS DENT-K 81-120 5 FOR DENTAL SURGERY TELESCOPES AND INSTRUMENTS SIAL 121-134 6 FOR SIALENDOSCOPY 7 FLEXIBLE ENDOSCOPES FL-E 135-142 8 HOSPITAL SUPPLIES HS 143-240 9 INSTRUMENTS FOR RHINOLOGY AND RHINOPLASTY N 241-298 10 BIPOLAR AND UNIPOLAR COAGULATION COA 299-312 11 HEADMIRRORS – HEADLIGHTS OMFS-J 313-324 12 AUTOFLUORESCENCE AF-INTRO, AF 325-342 13 HOLDING SYSTEMS HT 343-356 VISUALIZATION SYSTEMS OMFS-MICRO, OMFS-VITOM 357-378 14 FOR MICROSURGERY OMFS-UNITS-INTRO, UNITS AND ACCESSORIES U 1-54 15 OMFS-UNITS COMPONENTS OMFS-SP SP 1-58 16 SPARE PARTS KARL STORZ OR1 NEO™, TELEPRESENCE 17 HYGIENE, ENDOPROTECT1 ORAL AND MAXILLOFACIAL SURGERY 3rd EDITION 2/2012 US Important information for U.S. customers Note: Certain devices and references made herein to specific indications of use may have not received clearance or ap- proval by the United States Food and Drug Administration. Practitioners in the United States should first consult with their local KARL STORZ representative in order to ascertain product availability and specific labeling claims. Federal (USA) law restricts certain devices referenced herein to sale, distribution, and use by, or on the order of a physician, dentist, veterinarian, or other practitioner licensed by the law of the State in which she/he practices to use or order the use of the device. -

Lawtonelite Series Brochure
LawtonElite Series Mizuho America, Inc. 30057 Ahern Avenue Note: Mizuho America is constantly improving its Union City, CA 94587 products. All specification are subject to change Telephone: 510-324-4500 without notice. Toll Free: 800-699-2547 Fax: 510-324-4545 mizuho.com 2021 © Mizuho America ABPM 040 REV D LawtonElite Microscissors LawtonElite Series An intricately crafted, comprehensive micro instrumentation series for neurovascular • Ultra-thin and sharp blades with curved tips and skull base procedures. • Reusable and reposable options • Non-slip, counter-balanced, ergonomic handles SERIES INCLUDES: • Reusable and Reposable Micro Scissors • Can be used as a curved microdissector in closed position • Neurovascular Bypass Instrumentation • Micro Dissectors Titanium, Straight • 6.0 cm Working Length • 18.0 cm Total Length Designed in collaboration with • Reusable MICHAEL T. LAWTON, MD Titanium, Bayonet President and CEO, Barrow Neurological Institute • 7.6 cm Working Length Professor and Chair, Neurosurgery Chief, Neurovascular Surgery • 18.5 cm Total Length • Curved Left or Right • Reusable Michael T. Lawton MD is the chairman of the Department of Neurological Surgery at the Barrow Neurological Institute, as well as its President and Chief Executive Officer and the Robert F. Spetzler Endowed Chair in Neurosciences. He is chief of vascular Reposable, Straight and skull base neurosurgery, specializing in the surgical treatment of aneurysms, • 5.0 cm Working Length arteriovenous malformations, arteriovenous fistulas, cavernous malformations, and • 18.0 cm Total Length cerebral revascularization, including carotid endarterectomy. As the leader of the largest • Lifespan Up to 10 Procedures cerebrovascular center in the country, he has experience in surgically treating over 4800 • Always Sharp brain aneurysms and over 900 AVMs. -

STILLE Surgical Instruments Kirurgisk Perfektion I Närmare 180 År Surgical Perfection for Almost 180 Years
STILLE Surgical Instruments Kirurgisk perfektion i närmare 180 år Surgical Perfection for almost 180 years I närmare 180 år har vi utvecklat och tillverkat de bästa kirurgiska For almost 180 years, we have developed and manufactured the best instrumenten till världens mest krävande kirurger. Vi vill rikta ett stort surgical instruments for the world’s most demanding surgeons. tack till alla våra trogna kunder och samtidigt välkomna våra nya kunder. We would like to extend a heartfelt thank you to all our loyal I den här katalogen presenterar vi vårt kompletta sortiment av customers and a warm welcome to our new customers. In this catalog STILLEs original instrument. we present our complete range of STILLE original surgical instruments. Precision, hållbarhet och känsla är typiska egenskaper för alla Precision, durability and feel are characteristic qualities of all STILLE STILLE-instrument. Den stora majoriteten är handgjorda av våra instruments. The vast majority are handcrafted by our highly skilled skickliga instrumentmakare Eskilstuna. Instrumentets resa från rundstål instrument makers in Eskilstuna, west of Stockholm, Sweden. The instru- till ett färdigt instrument är lång, och består av många tillverkningssteg. ments’ journey from a rod of stainless steel to a finished instrument is a STILLEs unika tillverkningsmetod och användning av enbart det bästa long one, involving multiple stages. STILLE’s unique method of crafting its materialet ger våra instrument deras unika känsla och hållbarhet. instrument materials, and its usage of only the very highest-grade steels, give our instruments their unique feel and durability. I det första kapitlet hittar du våra saxar, allt från vanliga operationssaxar till våra unika SuperCut och Diamond SuperCut-saxar. -

CPT Code Description Charge Amount 83498 17-Alpha
CPT Code Description Charge Amount 83498 17-alpha-Hydroxyprogester 308.41 83497 5-HIAA, SO 125.99 83516 A MYELOPEROX (MPO) AB QL 74.1 86021 AB ID LEUKOCYTE AB/SO 610.25 86022 AB ID, PLATELET ABS;SRA U 1318 86720 AB LEPTOSPIRA/SO 166.12 86850 AB SCREEN (IDC) 207.83 86850 AB SCREEN RBC EA SRM TECH 195.25 86793 AB, YERSINIA/SO 149 74018 ABDOMEN 1 VIEW 348.75 74018 ABDOMEN 1 VIEW PORTABLE 321.36 74022 ABDOMEN ACUTE COMP WSGL V 398.36 74019 ABDOMEN COMPLETE 398.36 74018 ABDOMEN SGL ANTEROPOSTERI 475.8 49083 ABDOMINAL PARACENTESIS W/ 1216.89 86870 ABID,WNJ 294.85 ABLATOR APOLLORF XL90 ASP 877.8 86900 ABO BLOOD TYPE 370 86900 ABO,BBSO 176.5 73050 AC JOINTS W/WO WEIGHTS BI 297.94 ACCUGRID RADIOGRAPH BREAS 121.36 82164 ACE, CSF SO 144.38 83519 ACHR BIND AB QT,RIA/SO MA 258 83519 ACHR BIND QNT MGP/SO 181.37 83519 ACHR BLOC QNT MGP/SO 181.37 83519 ACHR GANGL NEUR AB,RIA/SO 258 83519 ACHR MOD QNT MGP/SO 201.16 87116 ACID FAST CULTURE SO 227.33 83519 ACR BLOCKING QNT SO 181.37 83519 ACR RECEPTOR QNT SO 108.61 82024 ACTH,SO 459.3 86602 ACTINOMYCES AB/SO 64 85347 ACTIVATED CLOTTING TIME 126.93 85307 Activated Protein C Resis 216.04 97535GO ACTIVITY DAILY LIVING 15 265.91 78278 ACUTE GI BLOOD LOSS IMAGI 1326.15 82017 ACYLCARNITINES; QUANT, EA 574 85397 ADAMSTS 13 ACTIVITY/SO 796.62 ADAPTER CATH LUER 8.69 ADAPTER CONFIDENCE CEMENT 743.66 ADAPTER DLP PERFUS Y W/6 47.54 ADAPTER FIBEROPTIC SWIVEL 73.16 ADAPTER LUER LOC SHORT 3/ 2.2 ADAPTER LUER TO COLDER 15.29 ADAPTER MALE-MALE 4.57 C1776 ADAPTER PFC SIGMA FEMORAL 8474.76 ADAPTER PLUG MALE CLAVE 5.02 ADAPTER PRODIGY EXTENSION 2340 ADAPTER UROSTOMY DRAIN TU 9.09 ADAPTER VERSO AIRWAY ADUL 33.51 82952 ADDL GLUCOSE > 3 SPEC 136.24 87260 ADENOV/ RSPFAC / SO 141.75 ADHESIVE DEMABOND .07 PEN 193.48 ADHESIVE DEMABOND .07 PEN 193.48 ADHESIVE DERMABOND PEN 0. -

Hospitals for War-Wounded
hospitals_war_cover_april2003 9.6.2005 13:47 Page 1 ICRC HOSPITALS FOR WAR-WOUNDED HOSPITALS FORHOSPITALS WAR-WOUNDED This book is intended for anyone who is faced A practical guide for setting up with the task of setting up or running a hospital and running a surgical hospital which admits war-wounded. It is a practical guide in an area of armed conflict based on the experience of four nurses who have managed independent hospitals set up by the International Committee of the Red Cross. It addresses specific problems associated with setting up a hospital in a difficult and potentially dangerous environment. It provides a framework for the administration of such a hospital. It also describes a system for managing the patients from admission to discharge and includes guidelines on how to manage an influx of wounded. These guidelines represent a realistic and achievable standard of care whatever the circumstances. A practical guide 0714/002 05/2005 1000 HOSPITALS FOR WAR-WOUNDED International Committee of the Red Cross 19 Avenue de la Paix 1202 Geneva, Switzerland T +41 22 734 6001 F +41 22 733 2057 E-mail: [email protected] www.icrc.org # ICRC, April 2005, revised and updated edition This book is dedicated to the memory of Jo´n Karlsson (died in Afghanistan, 22 April 1992) Fernanda Calado Hans Elkerbout Ingebjørg Foss Nancy Malloy Gunnhild Myklebust Sheryl Thayer (died in Chechnya, 17 December 1996) HOSPITALS FOR WAR-WOUNDED A practical guide for setting up and running a surgical hospital in an area of armed conflict Jenny Hayward-Karlsson Sue Jeffery Ann Kerr Holger Schmidt INTERNATIONAL COMMITTEE OF THE RED CROSS ISBN 2-88145-094-6 # International Committee of the Red Cross, Geneva, 1998 WEB address: http://www.icrc.org CONTENTS vii CONTENTS FOREWORD ............................................ -

Surgery Instrumnts Khaled Khalilia Group 7
Surgery Instrumnts khaled khalilia Group 7 Scalpel handle blade +blade scalpel blade disposable fixed blade knife (Péan - Hand-grip : This grip is best for initial incisions and larger cuts. - Pen-grip : used for more precise cuts with smaller blades. - Changing Blade with Hemostat Liston Charrière Saw AmputationAmputati knife on knife Gigli Saw . a flexible wire saw used by surgeons for bone cutting .A gigli saw is used mainly for amputation surgeries. is the removal of a body extremity by trauma, prolonged constriction, or surgery. Scissors: here are two types of scissors used in surgeries.( zirconia/ ceramic,/ nitinol /titanium) . Ring scissors look much like standard utility scissors with two finger loops. Spring scissors are small scissors used mostly in eye surgery or microsurgery . Bandage scissors: Bandage scissors are angled tip scissors. helps in cutting bandages without gouging the skin. To size bandages and dressings. To cut through medical gauze. To cut through bandages already in place. Tenotomy Scissors: used to perform delicate surgery. used to cut small tissues They can be straight or curved, and blunt or sharp, depending upon necessity. operations in ophthalmic surgery or in neurosurgery. 10 c”m Metzenbaum scissors: designed for cutting delicate tissue come in variable lengths and have a relatively long shank-to-blade ratio blades can be curved or straight. the most commonly used scissors for cutting tissue. Use: ental, obstetrical, gynecological, dermatological, ophthalmological. Metzenbaum scissors Bandage scissors Tenotomy scissors Surgical scissors Forceps: Without teeth With teeth Dissecting forceps (Anatomical) With teeth: for tougher(hart) tissue: Fascia,Skin Without teeth: (atraumatic): for delicate tissues (empfindlich): Bowel Vessels. -

Save Page As
Surgical Instruments Catalog Home // Scissors Scissors 055502 : Iris Barraquer Scissors Curved, 18 mm blades, 5-3/4" (14.5 cm) 357653 : You-Potts Vascular Scissors Narrow, thin blade and round spring handles designed for a more precise and controlled arteriotomy. 357653: Angled 45, 7-3/8" (18.5 cm) 357643 : You-Potts Vascular Scissors Narrow, thin blade and round spring handles designed for a more precise and controlled arteriotomy. 357643: Angled 120, 7" (18 cm) 506476 : Jako-Kleinsasser Micro-Laryngeal Scissors These Pilling Micro-laryngeal Scissors were designed specifically for everyday-use micro- surgery. They feature a slender 2 mm diameter stem with miniature distal jaws in the shape of scissors and are made of dull finished... 464610 : Mayo Dissecting Scissors, TC Weck Pattern, bright finish. Round blade. 464610: Straight, 6-1/2" (16.5 cm) 506478 : Jako-Kleinsasser Micro-Laryngeal Scissors These Pilling Micro-laryngeal Scissors were designed specifically for everyday-use micro- surgery. They feature a slender 2 mm diameter stem with miniature distal jaws in the shape of scissors and are made of dull finished... 506475 : Jako-Kleinsasser Micro-Laryngeal Scissors These Pilling Micro-laryngeal Scissors were designed specifically for everyday-use micro- surgery. They feature a slender 2 mm diameter stem with miniature distal jaws in the shape of scissors and are made of dull finished... 352145 : Castroviejo Scissors Spring handle for maximum control. Angled 45, 9 mm blades, 4-1/8" (10.5 cm) 357691 : Micro Vascular Scissors 357691: Angled 120 degrees, 7 mm blades, 6-1/4" (16 cm) 342221 : Jamison-Metzenbaum Tenotomy Scissors Curved, 7" (18.0cm) 464715 : Metzenbaum Scissors Curved, 7" (18.0cm), TC 790315 : Vernon Wire Scissors Straight, Serrated, 7 1/2" (19.0cm) 506477 : Jako-Kleinsasser Micro-Laryngeal Scissors These Pilling Micro-laryngeal Scissors were designed specifically for everyday-use micro- surgery. -
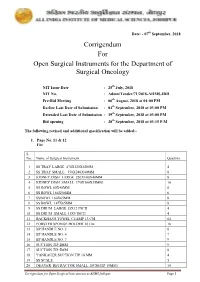
Corrigendum for Open Surgical Instruments for the Department Of
Date: - 07th September, 2018 Corrigendum For Open Surgical Instruments for the Department of Surgical Oncology NIT Issue Date : 25th July, 2018 NIT No. : Admn/Tender/71/2018-AIIMS.JDH Pre-Bid Meeting : 06th August, 2018 at 04:00 PM Earlier Last Date of Submission : 04th September, 2018 at 03:00 PM Extended Last Date of Submission : 19th September, 2018 at 03:00 PM Bid opening : 20th September, 2018 at 03:15 P.M The following revised and additional specification will be added:- 1. Page No. 11 & 12 For S. No. Name of Surgical Instrument Quantity 1 SS TRAY LARGE 470X320X50MM 4 2 SS TRAY SMALL 350X240X40MM 8 3 KIDNEY DISH LARGE 250X140X40MM 8 4 KIDNEY DISH SMALL 170X100X35MM 10 5 SS BOWL 80X40MM 6 6 SS BOWL 166X50MM 6 7 SSBOWL 160X65MM 8 8 SS BOWL 147X65MM 8 9 SS DRUM LARGE 15X12 INCH 4 10 SS DRUM SMALL 11X9 INCH 4 11 BACKHAUS TOWEL CLAMP 13 CM 64 12 FORSTER SPONGE HOLDER 18 Cm 18 13 BP HANDLE NO. 3 8 14 BP HANDLE NO. 4 7 15 BP HANDLE NO. 7 9 16 SUCTION TIP 2MM 9 17 SUCTION TIP 5MM 8 18 YANKAUER SUCTION TIP 10 MM 4 19 SS SCALE 5 20 DEAVER RETRACTOR SMALL 18CM(TIP 19MM) 14 Corrigendum for Open Surgical Instruments at AIIMS Jodhpur Page 1 21 DEAVER RETRACTOR MEDIUM 30.5CM (TIP 25 MM) 10 22 DEAVER RETRACTOR LARGE 31.5CM (TIP 50MM) 10 23 DOYEN’S RETRACTOR 4 24 MORRIS RETRACTOR 25cm ( BLADE 7x4cm) 6 25 SKIN HOOK 32 26 LANGENBECK RETRACTOR SMALL 16cm (TIP 21x 8mm) 16 27 LANGENBECK RETRACTOR MEDIUM 22cm (TIP 50x11mm) 16 28 LANGENBECK RETRACTOR LARGE 22.5cm (TIP 85x15mm) 14 29 C ZERNY RETRACTOR 17.2 cm 14 30 VEIN RETRACTOR 18 31 BALFOUR ABDOMINAL RETRACTOR 20cm 3 32 MASTOID RETRACTOR 4 33 PERIOSTEUM ELEVATOR SHARP 4 34 PERIOSTEUM ELEVATOR BLUNT 4 35 DISSECTING TOOTH FORCEPS 15 CM 16 36 DISSECTING PLAIN FORCEPS 18 CM 16 37 ARTERY FORCEPS CVD 15 CM 36 38 ARTERY FORCEPS ST. -

Healthcare Product Description Guideline
Canadian Healthcare Product Description Standardization Implementation Guidelines Version: 1.1 Updated: 2018 March Canadian Healthcare Product Description Standardization Implementation Guidelines Document Summary Document Item Current Value Document Name Canadian Healthcare Product Description Standardization Implementation Guidelines Document Version 1.1 Document Status Initial Publication December, 2010 Update formatting and appendix June 2016 Errata in abbreviation list “Universal” March 2018 Document Status FINAL Document Description Supplements the formal GS1 Canada Healthcare Supply Chain Guidelines January 2010 Version 1.0 providing information on the standardization of the short product description for the healthcare supply chain in Canada. Content Developers Organization Name 3M Canada Company Content Developer Ruth Wisotzki 3M Canada Company Content Developer Marilyn Piper HealthPRO Procurement Services Content Developer Ronda Harris HealthPRO Procurement Services Content Developer Tricia Cooper Medtronic Canada Inc. Content Developer Alain Boutin North Bay General Hospital Content Developer Lise Morris North York General Hospital Content Developer Marty McKinlay Ontario Hospital Association (OHA) Content Developer Peter Roman Source Medical Content Developer Anne Griffin Source Medical Content Developer Phil Kelly St. Michael’s Hospital Content Developer Diane Eley Toronto General Hospital (UHN) Content Developer Maria Masella Toronto General Hospital (UHN) Content Developer Wendy Watson Toronto Western Hospital (UHN) Content -

Equine Catalog
Dear Customer, Sontec Instruments, Inc. is a family owned & operated medical company, providing personalized service featuring the finest in surgical instrumentation for over half a century. Our surgical instruments encompass the entire human anatomy including specialty products specific to small and large animal surgery. Owner of Sontec Instruments, Dennis Russell Scanlan III and his sons, Johann, Stefan and Angus Scanlan bring with them a lifetime of experience creating the highest quality products made by the world’s leading manufacturing facilities featuring, cutting edge robotic technology, handmade workmanship combined with an understanding how to make exactly what our valued customers have come to expect. Dennis R. Scanlan, III President & CEO and his wife Caron C. Scanlan thank you, for the opportunity to present our specialty Equine catalog. Sincerely, Dennis Russell Scanlan III Printed 8/20 Colorado, USA / 1.800.821.7496 / www.SontecInstruments.com 1 Table of Contents Important Information . 4 Rongeurs ..............33 Equine Specialty . 55 Forceps . 121 Retractors ............149 Scissors. 159 Needle Holders . 209 Index ................228 Colorado, USA / 1.800.821.7496 / www.SontecInstruments.com 3 IMPORTANT INFORMATION Troubleshooting Guide Guarantee & Repairs Policy System Needle Holders • Equine (Arthroscopic) • Repair is necessary when needle holder Problem Cause Solution Sontec® surgical instruments are guaran- • Eye no longer securely holds needle when teed to be free of defects in materials and • Neurology & Orthopedic locked on the second ratchet tooth, and workmanship. Any Sontec® instrument that • Orthopedic & Arthroscopic needle turns easily by hand Rust Worn chrome plating on Be aware of plating condition and remove from is defective will be repaired or replaced at our • Urology brass instruments service when wear is visible.