Serous Membranes & Cavities
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Te2, Part Iii
TERMINOLOGIA EMBRYOLOGICA Second Edition International Embryological Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TE2, PART III Contents Caput V: Organogenesis Chapter 5: Organogenesis (continued) Systema respiratorium Respiratory system Systema urinarium Urinary system Systemata genitalia Genital systems Coeloma Coelom Glandulae endocrinae Endocrine glands Systema cardiovasculare Cardiovascular system Systema lymphoideum Lymphoid system Bibliographic Reference Citation: FIPAT. Terminologia Embryologica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, February 2017 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Embryologica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: ORGANOGENESIS Chapter 5: ORGANOGENESIS -
The Structure and Function of Breathing
CHAPTERCONTENTS The structure-function continuum 1 Multiple Influences: biomechanical, biochemical and psychological 1 The structure and Homeostasis and heterostasis 2 OBJECTIVE AND METHODS 4 function of breathing NORMAL BREATHING 5 Respiratory benefits 5 Leon Chaitow The upper airway 5 Dinah Bradley Thenose 5 The oropharynx 13 The larynx 13 Pathological states affecting the airways 13 Normal posture and other structural THE STRUCTURE-FUNCTION considerations 14 Further structural considerations 15 CONTINUUM Kapandji's model 16 Nowhere in the body is the axiom of structure Structural features of breathing 16 governing function more apparent than in its Lung volumes and capacities 19 relation to respiration. This is also a region in Fascla and resplrstory function 20 which prolonged modifications of function - Thoracic spine and ribs 21 Discs 22 such as the inappropriate breathing pattern dis- Structural features of the ribs 22 played during hyperventilation - inevitably intercostal musculature 23 induce structural changes, for example involving Structural features of the sternum 23 Posterior thorax 23 accessory breathing muscles as well as the tho- Palpation landmarks 23 racic articulations. Ultimately, the self-perpetuat- NEURAL REGULATION OF BREATHING 24 ing cycle of functional change creating structural Chemical control of breathing 25 modification leading to reinforced dysfunctional Voluntary control of breathing 25 tendencies can become complete, from The autonomic nervous system 26 whichever direction dysfunction arrives, for Sympathetic division 27 Parasympathetic division 27 example: structural adaptations can prevent NANC system 28 normal breathing function, and abnormal breath- THE MUSCLES OF RESPIRATION 30 ing function ensures continued structural adap- Additional soft tissue influences and tational stresses leading to decompensation. -
The Subperitoneal Space and Peritoneal Cavity: Basic Concepts Harpreet K
ª The Author(s) 2015. This article is published with Abdom Imaging (2015) 40:2710–2722 Abdominal open access at Springerlink.com DOI: 10.1007/s00261-015-0429-5 Published online: 26 May 2015 Imaging The subperitoneal space and peritoneal cavity: basic concepts Harpreet K. Pannu,1 Michael Oliphant2 1Department of Radiology, Memorial Sloan Kettering Cancer Center, 1275 York Avenue, New York, NY 10065, USA 2Department of Radiology, Wake Forest University School of Medicine, Winston-Salem, NC, USA Abstract The peritoneum is analogous to the pleura which has a visceral layer covering lung and a parietal layer lining the The subperitoneal space and peritoneal cavity are two thoracic cavity. Similar to the pleural cavity, the peri- mutually exclusive spaces that are separated by the toneal cavity is visualized on imaging if it is abnormally peritoneum. Each is a single continuous space with in- distended by fluid, gas, or masses. terconnected regions. Disease can spread either within the subperitoneal space or within the peritoneal cavity to Location of the abdominal and pelvic organs distant sites in the abdomen and pelvis via these inter- connecting pathways. Disease can also cross the peri- There are two spaces in the abdomen and pelvis, the toneum to spread from the subperitoneal space to the peritoneal cavity (a potential space) and the subperi- peritoneal cavity or vice versa. toneal space, and these are separated by the peritoneum (Fig. 1). Regardless of the complexity of development in Key words: Subperitoneal space—Peritoneal the embryo, the subperitoneal space and the peritoneal cavity—Anatomy cavity remain separated from each other, and each re- mains a single continuous space (Figs. -
Pubid-1446077038.Pdf
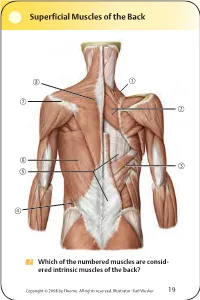
Superficial Muscles of the Back Which of the numbered muscles are consid- ered intrinsic muscles of the back? Copyright © 2008 by Thieme. All rights reserved. Illustrator: Karl Wesker 19 Superficial Muscles of the Back Posterior view. A Levator scapulae S Rhomboideus major D Serratus posterior inferior F Lumbar triangle, internal oblique G Thoracolumbar fascia, superficial layer H Latissimus dorsi J Scapular spine K Trapezius, transverse part Only the serratus posterior inferior is an intrinsic muscle of the back. The trapezius, latissimus dorsi, leva- tor scapulae, and rhomboideus muscles assist in move- ment of the shoulder or arm and are considered muscles of the upper limb. Fig. 2.1. Gilroy, MacPherson, Ross, Atlas of Anatomy, p. 22. Course of the Intercostal Nerves Copyright © 2008 by Thieme. All rights reserved. Illustrator: Markus Voll 39 Course of the Intercostal Nerves Coronal section. Anterior view. A Visceral pleura S Parietal pleura, diaphragmatic part D Diaphragm F Costodiaphragmatic recess G Endothoracic fascia H External intercostal J Costal groove K Intercostal vein, artery, and nerve Abnormal fluid collection in the pleural space (e.g., pleural effusion due to bronchial carcinoma) may necessitate the insertion of a chest tube. Generally, the optimal puncture site in a sitting patient is at the level of the 7th or 8th intercostal space on the posterior axillary line. The drain should always be introduced at the upper margin of a rib to avoid injuring the intercostal vein, artery, and nerve. Fig. 5.24. From Atlas of Anatomy, p. 59. Copyright ©2008 byThieme. Allrightsreserved. Illustrator: Markus Voll Right Lung 74 Right Lung Lateral and medial views. -

Malignant Pleural Mesothelioma
CLINICAL PRACTICE GUIDELINE LU-009 Version 2 MALIGNANT PLEURAL MESOTHELIOMA Effective Date: December, 2012 The recommendations contained in this guideline are a consensus of the Alberta Provincial Thoracic Malignancies Tumour Team synthesis of currently accepted approaches to management, derived from a review of relevant scientific literature. Clinicians applying these guidelines should, in consultation with the patient, use independent medical judgment in the context of individual clinical circumstances to direct care. CLINICAL PRACTICE GUIDELINE LU-009 Version 2 BACKGROUND Mesothelioma is a rare asbestos-related tumour that arises from mesenchymal cells that are found in the lining of the pleural cavity (Malignant Pleural Mesothelioma; MPM) in 70 to 90 percent of cases, and the peritoneal cavity in 10 to 30 percent of cases.1, 2 Due to the long latency period between exposure and disease, which has been reported to be between 30 and 50 years, most cases of mesothelioma being diagnosed today are the result of asbestos exposure in the 1960s and 1970s.3 Although safety measures for the use of asbestos were adopted in most countries several decades ago, the incidence rates, which are highly age-specific, are still rising, and are expected to peak over the next two decades.4-6 In Canada, the number of men diagnosed with mesothelioma has been steadily increasing over the past 20 years: there were 153 cases reported in 1984 versus 344 cases reported in 2003.3 Mesothelioma is less common in women: there were 78 Canadian women diagnosed with mesothelioma in 2003.3 In the United States, the peak mesothelioma incidence occurred in the early to mid-1990s and has possibly started to decline since then. -

Carcinomatous Cirrhosis of the Liver with Sarcomatosis of the Peritoneum 1
CARCINOMATOUS CIRRHOSIS OF THE LIVER WITH SARCOMATOSIS OF THE PERITONEUM 1 S. SANES, M.D., AND K. TERPLAN, M.D. (From tile Pathological Laboratory of the Buffalo General Hospital and School of Medicine, University of Buffalo) The following case is reported because of the occurrence of two different types of malignant neoplasm with typical portal cirrhosis of the liver. That a pathogenetic relationship exists between Laennec's cirrhosis and primary carcinoma of the liver is generally recognized. Whether the association of a peritoneal sarcoma with the cirrhosis in this case was more than a coincidence seemed an interesting point for discussion. REPORT OF CASE E. G., 11 white Italian male fifty-seven years old, was admitted to the Buffalo General Hospital on the service of Drs. N. G. Russell and A. H. Aaron, Nov. 25, 1934. He died Nov. 29, 1934. All his adult life he had partaken of large amounts of wine and whiskey daily. At the age of seventeen years he had suffered an attack of jaundice of several weeks' duration. The patient first began to lose weight and strength in 1932 and noticed that his skin was becoming dark. In March 1934 he complained of cramp-like abdominal pain, diarrhea, and bloating. The stools were watery. There was no nausea or vomiting. Upon hos pitalization, April 9, 1934, physical examination revealed that the pupils reacted to light and accommodation. The chest was emphysematous; breath sounds were diminished in both bases. The heart was regular; a systolic murmur was heard. The blood pressure was 118/70. The liver and spleen were palpable three finger breadths below the costal margin. -

7) Anatomy of OMENTUM
OMENTUM ANATOMY DEPARTMENT DR.SANAA AL-SHAARAWY Dr. Essam Eldin Salama OBJECTIVES • At the end of the lecture the students must know: • Brief knowledge about peritoneum as a thin serous membrane and its main parts; parietal and visceral. • The peritonial cavity and its parts the greater sac and the lesser sac (Omental bursa). • The peritoneal folds : omenta, mesenteries, and ligaments. • The omentum, as one of the peritonial folds • The greater omentum, its boundaries, and contents. • The lesser omentum, its boundaries, and contents. • The omental bursa, its boundaries. • The Epiploic foramen, its boundaries. • Mesentery of the small intestine, and ligaments of the liver. • Nerve supply of the peritoneum. • Clinical points. The peritoneum vIs a thin serous membrane, §Lining the wall of the abdominal and pelvic cavities, (the parietal peritoneum). §Covering the existing organs, (the visceral peritoneum). §The potential space between the two layers is the peritoneal cavity. Parietal Visceral The peritoneal Cavity vThe peritoneal cavity is the largest one in the body. vDivisions of the peritoneal cavity : §Greater sac; extends from Lesser Sac diaphragm down to the pelvis. §Lesser sac; lies behind the stomach. §Both cavities are interconnected through the epiploic foramen. §In male : the peritoneum is a closed sac . §In female : the sac is not completely closed because it Greater Sac communicates with the exterior through the uterine tubes, uterus and vagina. The peritoneum qIntraperitoneal and Intraperitoneal viscera retroperitoneal organs; describe the relationship between various organs and their peritoneal covering; §Intraperitonial structure; which is nearly totally covered by visceral peritoneum. §Retroperitonial structure; lies behind the peritoneum, and partially covered by visceral peritoneum. -

BODY CAVITIES and MESENTERY
73: BODY CAVITIES and MESENTERY We've already mentioned that all the organs in the body are wrapped in "bags" made of thin layers of connective tissue. These bags are often inside of other bags, or even inside of several bags. The largest bags define areas that we call body cavities. There are three main cavities: the thoracic cavity, the abdominal cavity and the pelvic cavity. The thoracic cavity is subdivided into three smaller cavities: the pleural cavity (containing the lungs), the mediastinum(in the middle), and the pericardial cavity (containing the heart). The pleural cavity is easy to understand because it simply contains the lungs. The pericardial cavity contains not only the heart itself, but the large blood vessels that come out of it, such as the aorta. The pericardial cavity is inside of the third cavity, the mediastinum. ("Media" means "middle" and "stinum" can refer to the "sternum," which is the bone that runs down the center of the ribcage.) The mediastinum contains not only the pericardial cavity but also part of the esophagus and trachea, the thymus (remember this organ from module 2 on the immune system?), and quite a few nerves and lymph nodes. The thin layers of connective tissues that surround these cavities are made primarily of collagen and elastin (produced by fibroblast cells) but they also contain some very tiny nerves and blood vessels, as well as cells that make serous fluid. As we've seen in the past few lessons, the diaphragm separates the thoracic cavity from the abdominal cavity. The abdominal cavity contains the stomach, the spleen, the tail of the pancreas, the last half of the duodenum, the small intestines, most of the large intestines, and the mesentery (thin layers of connective tissue that anchor the intestines to the back wall of the abdominal cavity). -

THORAX ANATOMY LAB 1: LEARNING OBJECTIVES Thoracic Wall, Pleural Cavities, and Lungs
THORAX ANATOMY LAB 1: LEARNING OBJECTIVES Thoracic Wall, Pleural Cavities, and Lungs Primary Learning Objectives 1. Define thorax and state the structures that form its anatomical boundaries. 2. Describe the locations and boundaries of the superior thoracic aperture (clinical: thoracic outlet) and the inferior thoracic aperture. Identify the costal arch (margin) and state the ribs that form the arch. 3. Identify and palpate the bones that compose the sternum (manubrium, body, and xiphoid process) and associated osteological features: jugular notch, clavicular notch, and sternal angle. 4. For the sternal angle, identify its associated vertebral level, state its anatomical relationship to the trachea and aorta, state its significance in creating an anatomical division of the mediastinum, and identify the ribs that join the sternum at its location. 5. Identify and palpate the clavicle, sternum, ribs, costal cartilages, intercostal spaces, and thoracic vertebrae. 6. Differentiate true ribs from false and floating ribs. 7. Identify the following osseous features on a rib: head, necK, rib (costal) tubercle, body, shaft, and the costal groove. 8. State the weaKest region of the rib that is commonly fractured and describe the anatomy and physiology involving flail chest. 9. Describe the possible clinical manifestations of supernumerary ribs. 10. Identify the following rib joints: costovertebral (costotransverse joint and vertebral body joint) and sternocostal. 11. Identify the transversus thoracis muscle, the external, internal, and innermost intercostal muscles, and state their innervation, blood supply, and functions. 12. State the structures that compose the neurovascular bundle within each intercostal space and identify each neurovascular bundle by number. 13. Identify the neurovascular bundle inferior to the twelfth rib and state the names of each structure composing the bundle (subcostal artery, subcostal vein, and subcostal nerve). -

Nasal Cavity Trachea Right Main (Primary) Bronchus Left Main (Primary) Bronchus Nostril Oral Cavity Pharynx Larynx Right Lung
Nasal cavity Oral cavity Nostril Pharynx Larynx Trachea Left main Right main (primary) (primary) bronchus bronchus Left lung Right lung Diaphragm © 2018 Pearson Education, Inc. 1 Cribriform plate of ethmoid bone Sphenoidal sinus Frontal sinus Posterior nasal aperture Nasal cavity • Nasal conchae (superior, Nasopharynx middle, and inferior) • Pharyngeal tonsil • Nasal meatuses (superior, middle, and inferior) • Opening of pharyngotympanic • Nasal vestibule tube • Nostril • Uvula Hard palate Oropharynx • Palatine tonsil Soft palate • Lingual tonsil Tongue Laryngopharynx Hyoid bone Larynx Esophagus • Epiglottis • Thyroid cartilage Trachea • Vocal fold • Cricoid cartilage (b) Detailed anatomy of the upper respiratory tract © 2018 Pearson Education, Inc. 2 Pharynx • Nasopharynx • Oropharynx • Laryngopharynx (a) Regions of the pharynx © 2018 Pearson Education, Inc. 3 Posterior Mucosa Esophagus Submucosa Trachealis Lumen of Seromucous muscle trachea gland in submucosa Hyaline cartilage Adventitia (a) Anterior © 2018 Pearson Education, Inc. 4 Intercostal muscle Rib Parietal pleura Lung Pleural cavity Trachea Visceral pleura Thymus Apex of lung Left superior lobe Right superior lobe Oblique Horizontal fissure fissure Right middle lobe Left inferior lobe Oblique fissure Right inferior lobe Heart (in pericardial cavity of mediastinum) Diaphragm Base of lung (a) Anterior view. The lungs flank mediastinal structures laterally. © 2018 Pearson Education, Inc. 5 Posterior Vertebra Esophagus (in posterior mediastinum) Root of lung at hilum Right lung • Left main bronchus Parietal pleura • Left pulmonary artery • Left pulmonary vein Visceral pleura Pleural cavity Left lung Thoracic wall Pulmonary trunk Pericardial membranes Heart (in mediastinum) Sternum Anterior mediastinum Anterior (b) Transverse section through the thorax, viewed from above © 2018 Pearson Education, Inc. 6 Alveolar duct Alveoli Respiratory bronchioles Alveolar duct Terminal bronchiole Alveolar sac (a) Diagrammatic view of respiratory bronchioles, alveolar ducts, and alveoli © 2018 Pearson Education, Inc. -

Colon & Rectum Staging Form
Colon & Rectum Staging Form CLINICAL PATHOLOGIC Extent of disease before STAGE CATEGORY DEFINITIONS Extent of disease through any treatment completion of definitive surgery y clinical – staging completed TUMOR SIZE: LATERALITY: y pathologic – staging complet- after neoadjuvant therapy but ed after neoadjuvant therapy before subsequent surgery left right bilateral AND subsequent surgery PRIMARY TUMOR (T) TX Primary tumor cannot be assessed TX T0 No evidence of primary tumor T0 Tis Carcinoma in situ: intraepithelial or invasion of lamina propria* Tis T1 Tumor invades submucosa T1 T2 Tumor invades muscularis propria T2 T3 Tumor invades through the muscularis propria into pericolorectal tissues T3 T4a Tumor penetrates to the surface of the visceral peritoneum** T4a T4b Tumor directly invades or is adherent to other organs or structures^,** T4b *Note: Tis includes cancer cells confined within the glandular basement membrane (intraepithelial) or mucosal lamina propria (intramucosal) with no extension through the muscularis mucosae into the submucosa. ^Note: Direct invasion in T4 includes invasion of other organs or other segments of the colorectum as a result of direct extension through the serosa, as confirmed on microscopic examination (for example, invasion of the sigmoid colon by a carcinoma of the cecum) or, for cancers in a retro-peritoneal or subperitoneal location, direct invasion of other organs or structures by virtue of extension beyond the muscularis propria (i.e., respectively, a tumor on the posterior wall of the descending colon invading the left kidney or lateral abdominal wall; or a mid or distal rectal cancer with invasion of prostate, seminal vesicles, cervix or vagina). **Tumor that is adherent to other organs or structures, grossly, is classified cT4b. -

The Digestive System
69 chapter four THE DIGESTIVE SYSTEM THE DIGESTIVE SYSTEM The digestive system is structurally divided into two main parts: a long, winding tube that carries food through its length, and a series of supportive organs outside of the tube. The long tube is called the gastrointestinal (GI) tract. The GI tract extends from the mouth to the anus, and consists of the mouth, or oral cavity, the pharynx, the esophagus, the stomach, the small intestine, and the large intes- tine. It is here that the functions of mechanical digestion, chemical digestion, absorption of nutrients and water, and release of solid waste material take place. The supportive organs that lie outside the GI tract are known as accessory organs, and include the teeth, salivary glands, liver, gallbladder, and pancreas. Because most organs of the digestive system lie within body cavities, you will perform a dissection procedure that exposes the cavities before you begin identifying individual organs. You will also observe the cavities and their associated membranes before proceeding with your study of the digestive system. EXPOSING THE BODY CAVITIES should feel like the wall of a stretched balloon. With your skinned cat on its dorsal side, examine the cutting lines shown in Figure 4.1 and plan 2. Extend the cut laterally in both direc- out your dissection. Note that the numbers tions, roughly 4 inches, still working with indicate the sequence of the cutting procedure. your scissors. Cut in a curved pattern as Palpate the long, bony sternum and the softer, shown in Figure 4.1, which follows the cartilaginous xiphoid process to find the ventral contour of the diaphragm.