Cladribine Injection
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Application of a Characterized Pre-Clinical
THE APPLICATION OF A CHARACTERIZED PRE-CLINICAL GLIOBLASTOMA ONCOSPHERE MODEL TO IN VITRO AND IN VIVO THERAPEUTIC TESTING by Kelli M. Wilson A dissertation submitted to Johns Hopkins University in conformity with the requirements for the degree of Doctor of Philosophy Baltimore, Maryland March, 2014 ABSTRACT Glioblastoma multiforme (GBM) is a lethal brain cancer with a median survival time (MST) of approximately 15 months following treatment. A serious challenge facing the development of new drugs for the treatment of GBM is that preclinical models fail to replicate the human GBM phenotype. Here we report the Johns Hopkins Oncosphere Panel (JHOP), a panel of GBM oncosphere cell lines. These cell lines were validated by their ability to form tumors intracranially with histological features of human GBM and GBM variant tumors. We then completed whole exome sequencing on JHOP and found that they contain genetic alterations in GBM driver genes such as PTEN, TP53 and CDKN2A. Two JHOP cell lines were utilized in a high throughput drug screen of 466 compounds that were selected to represent late stage clinical development and a wide range of mechanisms. Drugs that were inhibitory in both cell lines were EGFR inhibitors, NF-kB inhibitors and apoptosis activators. We also examined drugs that were inhibitory in a single cell line. Effective drugs in the PTEN null and NF1 wild type cell line showed a limited number of drug targets with EGFR inhibitors being the largest group of cytotoxic compounds. However, in the PTEN mutant, NF1 null cell line, VEGFR/PDGFR inhibitors and dual PIK3/mTOR inhibitors were the most common effective compounds. -

Folic Acid Antagonists: Antimicrobial and Immunomodulating Mechanisms and Applications
International Journal of Molecular Sciences Review Folic Acid Antagonists: Antimicrobial and Immunomodulating Mechanisms and Applications Daniel Fernández-Villa 1, Maria Rosa Aguilar 1,2 and Luis Rojo 1,2,* 1 Instituto de Ciencia y Tecnología de Polímeros, Consejo Superior de Investigaciones Científicas, CSIC, 28006 Madrid, Spain; [email protected] (D.F.-V.); [email protected] (M.R.A.) 2 Consorcio Centro de Investigación Biomédica en Red de Bioingeniería, Biomateriales y Nanomedicina, 28029 Madrid, Spain * Correspondence: [email protected]; Tel.: +34-915-622-900 Received: 18 September 2019; Accepted: 7 October 2019; Published: 9 October 2019 Abstract: Bacterial, protozoan and other microbial infections share an accelerated metabolic rate. In order to ensure a proper functioning of cell replication and proteins and nucleic acids synthesis processes, folate metabolism rate is also increased in these cases. For this reason, folic acid antagonists have been used since their discovery to treat different kinds of microbial infections, taking advantage of this metabolic difference when compared with human cells. However, resistances to these compounds have emerged since then and only combined therapies are currently used in clinic. In addition, some of these compounds have been found to have an immunomodulatory behavior that allows clinicians using them as anti-inflammatory or immunosuppressive drugs. Therefore, the aim of this review is to provide an updated state-of-the-art on the use of antifolates as antibacterial and immunomodulating agents in the clinical setting, as well as to present their action mechanisms and currently investigated biomedical applications. Keywords: folic acid antagonists; antifolates; antibiotics; antibacterials; immunomodulation; sulfonamides; antimalarial 1. -

LEUSTATIN (Cladribine) Injection Should Be Administered Under the Supervision of a Qualified Physician Experienced in the Use of Antineoplastic Therapy
LEUSTATIN (cladribine) Injection For Intravenous Infusion Only WARNING LEUSTATIN (cladribine) Injection should be administered under the supervision of a qualified physician experienced in the use of antineoplastic therapy. Suppression of bone marrow function should be anticipated. This is usually reversible and appears to be dose dependent. Serious neurological toxicity (including irreversible paraparesis and quadraparesis) has been reported in patients who received LEUSTATIN Injection by continuous infusion at high doses (4 to 9 times the recommended dose for Hairy Cell Leukemia). Neurologic toxicity appears to demonstrate a dose relationship; however, severe neurological toxicity has been reported rarely following treatment with standard cladribine dosing regimens. Acute nephrotoxicity has been observed with high doses of LEUSTATIN (4 to 9 times the recommended dose for Hairy Cell Leukemia), especially when given concomitantly with other nephrotoxic agents/therapies. DESCRIPTION LEUSTATIN (cladribine) Injection (also commonly known as 2-chloro-2΄-deoxy- β -D-adenosine) is a synthetic antineoplastic agent for continuous intravenous infusion. It is a clear, colorless, sterile, preservative-free, isotonic solution. LEUSTATIN Injection is available in single-use vials containing 10 mg (1 mg/mL) of cladribine, a chlorinated purine nucleoside analog. Each milliliter of LEUSTATIN Injection contains 1 mg of the active ingredient and 9 mg (0.15 mEq) of sodium chloride as an inactive ingredient. The solution has a pH range of 5.5 to 8.0. Phosphoric -

Synthesis of Ribavirin, Tecadenoson, and Cladribine by Enzymatic Transglycosylation
catalysts Article Synthesis of Ribavirin, Tecadenoson, and Cladribine by Enzymatic Transglycosylation 1, 2 2,3 2 Marco Rabuffetti y, Teodora Bavaro , Riccardo Semproli , Giulia Cattaneo , Michela Massone 1, Carlo F. Morelli 1 , Giovanna Speranza 1,* and Daniela Ubiali 2,* 1 Department of Chemistry, University of Milan, via Golgi 19, I-20133 Milano, Italy; marco.rabuff[email protected] (M.R.); [email protected] (M.M.); [email protected] (C.F.M.) 2 Department of Drug Sciences, University of Pavia, viale Taramelli 12, I-27100 Pavia, Italy; [email protected] (T.B.); [email protected] (R.S.); [email protected] (G.C.) 3 Consorzio Italbiotec, via Fantoli 15/16, c/o Polo Multimedica, I-20138 Milano, Italy * Correspondence: [email protected] (G.S.); [email protected] (D.U.); Tel.: +39-02-50314097 (G.S.); +39-0382-987889 (D.U.) Present address: Department of Food, Environmental and Nutritional Sciences, University of Milan, y via Mangiagalli 25, I-20133 Milano, Italy. Received: 7 March 2019; Accepted: 8 April 2019; Published: 12 April 2019 Abstract: Despite the impressive progress in nucleoside chemistry to date, the synthesis of nucleoside analogues is still a challenge. Chemoenzymatic synthesis has been proven to overcome most of the constraints of conventional nucleoside chemistry. A purine nucleoside phosphorylase from Aeromonas hydrophila (AhPNP) has been used herein to catalyze the synthesis of Ribavirin, Tecadenoson, and Cladribine, by a “one-pot, one-enzyme” transglycosylation, which is the transfer of the carbohydrate moiety from a nucleoside donor to a heterocyclic base. As the sugar donor, 7-methylguanosine iodide and its 20-deoxy counterpart were synthesized and incubated either with the “purine-like” base or the modified purine of the three selected APIs. -

COMPARISON of the WHO ATC CLASSIFICATION & Ephmra/Intellus Worldwide ANATOMICAL CLASSIFICATION
COMPARISON OF THE WHO ATC CLASSIFICATION & EphMRA/Intellus Worldwide ANATOMICAL CLASSIFICATION: VERSION June 2019 2 Comparison of the WHO ATC Classification and EphMRA / Intellus Worldwide Anatomical Classification The following booklet is designed to improve the understanding of the two classification systems. The development of the two systems had previously taken place separately. EphMRA and WHO are now working together to ensure that there is a convergence of the 2 systems rather than a divergence. In order to better understand the two classification systems, we should pay attention to the way in which substances/products are classified. WHO mainly classifies substances according to the therapeutic or pharmaceutical aspects and in one class only (particular formulations or strengths can be given separate codes, e.g. clonidine in C02A as antihypertensive agent, N02C as anti-migraine product and S01E as ophthalmic product). EphMRA classifies products, mainly according to their indications and use. Therefore, it is possible to find the same compound in several classes, depending on the product, e.g., NAPROXEN tablets can be classified in M1A (antirheumatic), N2B (analgesic) and G2C if indicated for gynaecological conditions only. The purposes of classification are also different: The main purpose of the WHO classification is for international drug utilisation research and for adverse drug reaction monitoring. This classification is recommended by the WHO for use in international drug utilisation research. The EphMRA/Intellus Worldwide classification has a primary objective to satisfy the marketing needs of the pharmaceutical companies. Therefore, a direct comparison is sometimes difficult due to the different nature and purpose of the two systems. -

Resistance to Antifolates
Oncogene (2003) 22, 7431–7457 & 2003 Nature Publishing Group All rights reserved 0950-9232/03 $25.00 www.nature.com/onc Resistance to antifolates Rongbao Zhao1 and I David Goldman*,1 1Departments of Medicine and Molecular, Pharmacology, Albert Einstein College of Medicine, Bronx, New York, USA The antifolates were the first class of antimetabolites to the kinetics of the interaction between MTX and DHFR enter the clinics more than 50 years ago. Over the was fully understood, and not until the late 1970s and following decades, a full understanding of their mechan- early 1980s when polyglutamate derivatives of MTX were isms of action and chemotherapeutic potential evolved detected and their pharmacologic importance clarified. along with the mechanisms by which cells develop Likewise, an understanding of tumor cell resistance to resistance to these drugs. These principals served as a antifolates evolved slowly, often paralleling the emergence basis for the subsequent exploration and understanding of of new molecular concepts. As the mechanisms of the mechanisms of resistance to a variety of diverse resistance to antifolates were characterized, this provided antineoplastics with different cellular targets. This section insights and principles that were broadly applicable to describes the bases for intrinsic and acquired antifolate other antineoplastics. Ultimately, this knowledge led to the resistance within the context of the current understanding development of a new generation of antifolates, in the late of the mechanisms of actions and cytotoxic determinants 1980s and 1990s, which are potent direct inhibitors of of these agents. This encompasses impaired drug transport tetrahydrofolate (THF)-cofactor-dependent enzymes. Sev- into cells, augmented drug export, impaired activation of eral of these drugs are now in clinical trials, and the antifolates through polyglutamylation, augmented hydro- activity of one, pemetrexed, has been confirmed in a large lysis of antifolate polyglutamates, increased expression Phase III trial (Vogelzang et al., 2003). -
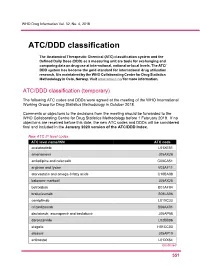
ATC/DDD Classification
WHO Drug Information Vol. 32, No. 4, 2018 ATC/DDD classification The Anatomical Therapeutic Chemical (ATC) classification system and the Defined Daily Dose (DDD) as a measuring unit are tools for exchanging and comparing data on drug use at international, national or local levels. The ATC/ DDD system has become the gold standard for international drug utilization research. It is maintained by the WHO Collaborating Centre for Drug Statistics Methodology in Oslo, Norway. Visit www.whocc.no/ for more information. ATC/DDD classification (temporary) The following ATC codes and DDDs were agreed at the meeting of the WHO International Working Group for Drug Statistics Methodology in October 2018. Comments or objections to the decisions from the meeting should be forwarded to the WHO Collaborating Centre for Drug Statistics Methodology before 1 February 2019. If no objections are received before this date, the new ATC codes and DDDs will be considered final and included in the January 2020 version of the ATC/DDD Index. New ATC 5th level codes ATC level name/INN ATC code acalabrutinib L01XE51 amenamevir J05AX26 amlodipine and celecoxib C08CA51 arginine and lysine V03AF11 atorvastatin and omega-3 fatty acids C10BA08 baloxavir marboxil J05AX25 betrixaban B01AF04 brolucizumab S01LA06 cemiplimab L01XC33 crizanlizumab B06AX01 daclatasvir, asunaprevir and beclabuvir J05AP58 darolutamide L02BB06 elagolix H01CC03 elbasvir J05AP10 entinostat L01XX64 Continued 5 51 ATC/DDD classification WHO Drug Information Vol. 32, No. 4, 2018 New ATC 5th level codes (continued) -

Organic Anion Transporting Polypeptides: Emerging Roles in Cancer Pharmacology
Molecular Pharmacology Fast Forward. Published on February 19, 2019 as DOI: 10.1124/mol.118.114314 This article has not been copyedited and formatted. The final version may differ from this version. MOL # 114314 Organic Anion Transporting Polypeptides: Emerging Roles in Cancer Pharmacology Rachael R. Schulte and Richard H. Ho Department of Pediatrics, Division of Pediatric Hematology-Oncology, Vanderbilt University Medical Center, Nashville, TN (R.R.S., R.H.H.) Downloaded from molpharm.aspetjournals.org at ASPET Journals on September 28, 2021 1 Molecular Pharmacology Fast Forward. Published on February 19, 2019 as DOI: 10.1124/mol.118.114314 This article has not been copyedited and formatted. The final version may differ from this version. MOL # 114314 OATPs and Cancer Pharmacology Corresponding Author: Richard H. Ho, MD MSCI 397 PRB 2220 Pierce Avenue Vanderbilt University Medical Center Nashville, Tennessee 37232 Downloaded from Tel: (615) 936-2802 Fax: (615) 875-1478 Email: [email protected] molpharm.aspetjournals.org Number of pages of text: 24 Number of tables: 3 Number of figures: 1 References: 204 at ASPET Journals on September 28, 2021 Number of words: Abstract: 201 Introduction: 1386 Discussion: 7737 ABBREVIATIONS: ASBT, apical sodium dependent bile acid transporter; AUC, area under the plasma time:concentration curve; BCRP, breast cancer related protein; BSP, bromosulfophthalein; CCK-8, cholecystokinin octapeptide; DHEAS, dehydroepiandrosterone sulfate; DPDPE, [D-penicillamine2,5] enkephalin; E2G, estradiol-17ß-glucuronide; E3S, estrone-3-sulfate; ENT, equilibrative nucleoside transporter; GCA, glycocholate; HEK, human embryonic kidney; IVS, intervening sequence (notation for intronic mutations); LD, linkage disequilibrium; MATE, multidrug and toxic compound extrusion; MCT, monocarboxylate 2 Molecular Pharmacology Fast Forward. -

Original Article Treatment of Hairy Cell Leukemia with Cladribine
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by RERO DOC Digital Library Annals of Oncology 13: 1641–1649, 2002 Original article DOI: 10.1093/annonc/mdf272 Treatment of hairy cell leukemia with cladribine (2-chlorodeoxyadenosine) by subcutaneous bolus injection: a phase II study A. von Rohr1*, S.-F. H. Schmitz2, A. Tichelli3, U. Hess4, D. Piguet5, M. Wernli6, N. Frickhofen7, G. Konwalinka8, G. Zulian9, M. Ghielmini10, B. Rufener2, C. Racine1, M. F. Fey1, T. Cerny1, D. Betticher1 & A. Tobler11 On Behalf of the Swiss Group for Clinical Cancer Research (SAKK), Bern, Switzerland 1Institute of Medical Oncology, Inselspital, Bern; 2SIAK Coordinating Center, Bern; 3Division of Hematology, Kantonsspital, Basel; 4Department of Internal Medicine, Kantonsspital, St Gallen; 5Department of Internal Medicine, Hôpital des Cadolles, Neuchâtel; 6Department of Internal Medicine, Kantonsspital, Aarau, Switzerland; 7Department of Internal Medicine, University Hospital, Ulm, Germany; 8Department of Internal Medicine, University Hospital, Innsbruck, Austria; 9Department of Internal Medicine, University Hospital, Geneva; 10Oncology Institute of Southern Switzerland, Bellinzona; 11Central Hematology Laboratory, University Hospital, Bern, Switzerland Received 8 January 2002; revised 11 April 2002; accepted 24 April 2002 Background: To assess the activity and toxicity of 2-chlorodeoxyadenosine (cladribine, CDA) given by subcutaneous bolus injections to patients with hairy cell leukemia (HCL). Patients and methods: Sixty-two eligible patients with classic or prolymphocytic HCL (33 non- pretreated patients, 15 patients with relapse after previous treatment, and 14 patients with progressive disease during a treatment other than CDA) were treated with CDA 0.14 mg/kg/day by subcutaneous bolus injections for five consecutive days. -

Practical Aspects of the Use of Intrathecal Chemotherapy
Farmacia Hospitalaria ISSN: 1130-6343 ISSN: 2171-8695 Aula Médica Ediciones (Grupo Aula Médica S.L.) Practical aspects of the use of intrathecal chemotherapy Olmos-Jiménez, Raquel; Espuny-Miró, Alberto; Cárceles-Rodríguez, Carlos; Díaz-Carrasco, María Sacramento Practical aspects of the use of intrathecal chemotherapy Farmacia Hospitalaria, vol. 41, no. 1, 2017 Aula Médica Ediciones (Grupo Aula Médica S.L.) Available in: http://www.redalyc.org/articulo.oa?id=365962303008 DOI: 10.7399/fh.2017.41.1.10616 PDF generated from XML JATS4R by Redalyc Project academic non-profit, developed under the open access initiative REVISIONES Practical aspects of the use of intrathecal chemotherapy Aspectos prácticos de la utilización de quimioterapia intratecal Raquel Olmos-Jiménez 1 Universidad de Murcia, Spain Alberto Espuny-Miró 1 Universidad de Murcia, Spain Carlos Cárceles-Rodríguez 1 Universidad de Murcia, Spain María Sacramento Díaz-Carrasco 2 Hospital Clínico Universitario Virgen de la Arrixaca, Spain Farmacia Hospitalaria, vol. 41, no. 1, Abstract 2017 Introduction: Intrathecal chemotherapy is frequently used in clinical practice for treatment and prevention of neoplastic meningitis. Despite its widespread use, there is Aula Médica Ediciones (Grupo Aula Médica S.L.) little information about practical aspects such as the volume of drug to be administered or its preparation and administration. Received: 28 July 2016 Accepted: 15 October 2016 Objective: To conduct a literature review about practical aspects of the use of intrathecal chemotherapy. DOI: 10.7399/.2017.41.1.10616 Materials: Search in PubMed/ Medline using the terms “chemotherapy AND intrathecal”, analysis of secondary and tertiary information sources. CC BY-NC-ND Results: e most widely used drugs in intrathecal therapy are methotrexate and cytarabine, at variable doses. -
Preoperative Medication Directive a Clinical Practice Protocol Practitioner Information
Preoperative Medication Directive A Clinical Practice Protocol Practitioner Information Please note: this is a living document subject to change. We recommend that this not be printed but rather accessed on line for the most current information. Nov 2017 Table of Contents Regional practice protocol for Preoperative Medication Page Directives Purpose & Intent 1 Practice Outcomes 1 Background 2 Components 2 References 3 Authors 4 Guidelines- Section A (for select Nurses) 5 Guidelines- Section B (for Surgeons) 12 Guidelines- Section C (for Anaesthesiologists) pending PURPOSE AND INTENT Who this document is for: These sectioned documents are a resource and an information source for Preoperative Assessment/Anaesthesia Clinic Staff, Surgeons and Anaesthesiologists. Each Section (A, B, etc...) was created for a primary user group. Users of this document shall always employ critical thinking and seek additional guidance from the appropriate colleagues (ie: anaesthesiologist and/or surgeon/prescribing physician) when concerns or variances arise. 1. Practice Outcomes How to use this document: This tool is to supplement the practice at each site. Implementation of this document will be at the discretion of the site leaders, however the directions provided to patients regarding preoperative medications should be consistent with this document (under the consideration of critical thinking). Clinical judgment, critical thinking and patient specific needs & concerns should always be employed, considered and addressed for all parts of the document. Any care provider with a Preoperative Medication Directive medication question is asked to submit in writing the medication in question (along with any supporting evidence if available) to the PAC Working Group (chair) [email protected] for consideration. -

Cladribine (Leustatin®) Pronounced: “KLAD-Rih-BEAN”
Cladribine Chemotherapy: Cladribine (Leustatin®) Pronounced: “KLAD-rih-BEAN” How drug is given: By vein (IV) Purpose: To treat hairy cell leukemia, non-Hodgkin lymphoma, chronic lymphocytic leukemia (CLL), and other cancers Things that may occur during or within hours of treatment • Facial flushing (warmth or redness of the face), itching, or a skin rash could occur. These symptoms are due to an allergic response and should be reported to your cancer care team right away. Things that may occur days to weeks after drug is given • Your blood cell counts may drop. This is known as bone marrow suppression. This includes a decrease in your: o Red blood cells, which carry oxygen in your body to help give you energy o White blood cells, which fight infection in your body o Platelets, which help clot the blood to stop bleeding This may happen 7 to 14 days after the drug is given and then blood counts should return to normal. If you have a fever of 100.5°F (38°C) or higher, chills, a cough, or any bleeding problems, tell your cancer care team right away. • Some patients may feel very tired, also known as fatigue. You may need to rest or take naps more often. Mild to moderate exercise can also be helpful in maintaining your energy. • Some patients may have mild nausea. You may be given medicine to help with this. • You may get a headache. Please talk to your doctor or nurse about what you can take for this. • In rare cases, nerves can be affected by this medicine.