Acute Myeloid Leukemia (AML) Treatment Regimens
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

214120Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 214120Orig1s000 MULTI-DISCIPLINE REVIEW Summary Review Office Director Cross Discipline Team Leader Review Clinical Review Non-Clinical Review Statistical Review Clinical Pharmacology Review NDA Multidisciplinary Review and Evaluation Application Number NDA 214120 Application Type Type 3 Priority or Standard Priority Submit Date 3/3/2020 Received Date 3/3/2020 PDUFA Goal Date 9/3/2020 Office/Division OOD/DHM1 Review Completion Date 9/1/2020 Applicant Celgene Corporation Established Name Azacitidine (Proposed) Trade Name Onureg Pharmacologic Class Nucleoside metabolic inhibitor Formulations Tablet (200 mg, 300 mg) (b) (4) Applicant Proposed Indication/Population Recommendation on Regulatory Regular approval Action Recommended Indication/ For continued treatment of adult patients with acute Population myeloid leukemia who achieved first complete remission (CR) or complete remission with incomplete blood count recovery (CRi) following intensive induction chemotherapy and are not able to complete intensive curative therapy. SNOMED CT for the Recommended 91861009 Indication/Population Recommended Dosing Regimen 300 mg orally daily on Days 1 through 14 of each 28-day cycle Reference ID: 4664570 NDA Multidisciplinary Review and Evaluation NDA 214120 Onureg (azacitidine tablets) TABLE OF CONTENTS TABLE OF CONTENTS ................................................................................................................................... 2 TABLE OF TABLES ....................................................................................................................................... -

A Systematic Review of the Effectiveness of Docetaxel and Mitoxantrone for the Treatment of Metastatic Hormone-Refractory Prostate Cancer
British Journal of Cancer (2006) 95, 457 – 462 & 2006 Cancer Research UK All rights reserved 0007 – 0920/06 $30.00 www.bjcancer.com A systematic review of the effectiveness of docetaxel and mitoxantrone for the treatment of metastatic hormone-refractory prostate cancer *,1 1 1 1 2 3 4 5 R Collins , R Trowman , G Norman , K Light , A Birtle , E Fenwick , S Palmer and R Riemsma 1 2 Centre for Reviews and Dissemination, University of York, Heslington, York YO10 5DD, UK; Rosemere Cancer Centre, Royal Preston Hospital, Sharoe 3 Green Lane North, Fulwood, Preston PR2 9HT, UK; Public Health & Health Policy, Division of Community Based Sciences, University of Glasgow, 4 5 1 Lilybank Gardens, Glasgow G12 8RZ, UK; Centre for Health Economics, University of York, Heslington, York YO10 5DD, UK; Kleijnen Systematic Reviews Ltd, Westminster Business Centre, 10 Great North Way, Nether Poppleton, York YO26 6RB, UK Clinical Studies A systematic review was performed to evaluate the clinical effectiveness of docetaxel in combination with prednisolone (docetaxel is licensed in the UK for use in combination with prednisone or prednisolone for the treatment of patients with metastatic hormone- refractory prostate cancer. Prednisone is not used in the UK, but it is reasonable to use docetaxel plus prednisone data in this review of docetaxel plus prednisolone) for the treatment of metastatic hormone-refractory prostate cancer. A scoping search identified a trial of docetaxel plus prednisone vs mitoxantrone plus prednisone, but did not identify any trials comparing docetaxel plus prednisolone/prednisone with any other treatments. Therefore, we considered additional indirect evidence that would enable a comparison of docetaxel plus prednisolone/prednisone with other chemotherapy regimens and active supportive care. -

The Application of a Characterized Pre-Clinical
THE APPLICATION OF A CHARACTERIZED PRE-CLINICAL GLIOBLASTOMA ONCOSPHERE MODEL TO IN VITRO AND IN VIVO THERAPEUTIC TESTING by Kelli M. Wilson A dissertation submitted to Johns Hopkins University in conformity with the requirements for the degree of Doctor of Philosophy Baltimore, Maryland March, 2014 ABSTRACT Glioblastoma multiforme (GBM) is a lethal brain cancer with a median survival time (MST) of approximately 15 months following treatment. A serious challenge facing the development of new drugs for the treatment of GBM is that preclinical models fail to replicate the human GBM phenotype. Here we report the Johns Hopkins Oncosphere Panel (JHOP), a panel of GBM oncosphere cell lines. These cell lines were validated by their ability to form tumors intracranially with histological features of human GBM and GBM variant tumors. We then completed whole exome sequencing on JHOP and found that they contain genetic alterations in GBM driver genes such as PTEN, TP53 and CDKN2A. Two JHOP cell lines were utilized in a high throughput drug screen of 466 compounds that were selected to represent late stage clinical development and a wide range of mechanisms. Drugs that were inhibitory in both cell lines were EGFR inhibitors, NF-kB inhibitors and apoptosis activators. We also examined drugs that were inhibitory in a single cell line. Effective drugs in the PTEN null and NF1 wild type cell line showed a limited number of drug targets with EGFR inhibitors being the largest group of cytotoxic compounds. However, in the PTEN mutant, NF1 null cell line, VEGFR/PDGFR inhibitors and dual PIK3/mTOR inhibitors were the most common effective compounds. -

The Clinical Management of Chronic Myelomonocytic Leukemia Eric Padron, MD, Rami Komrokji, and Alan F
The Clinical Management of Chronic Myelomonocytic Leukemia Eric Padron, MD, Rami Komrokji, and Alan F. List, MD Dr Padron is an assistant member, Dr Abstract: Chronic myelomonocytic leukemia (CMML) is an Komrokji is an associate member, and Dr aggressive malignancy characterized by peripheral monocytosis List is a senior member in the Department and ineffective hematopoiesis. It has been historically classified of Malignant Hematology at the H. Lee as a subtype of the myelodysplastic syndromes (MDSs) but was Moffitt Cancer Center & Research Institute in Tampa, Florida. recently demonstrated to be a distinct entity with a distinct natu- ral history. Nonetheless, clinical practice guidelines for CMML Address correspondence to: have been inferred from studies designed for MDSs. It is impera- Eric Padron, MD tive that clinicians understand which elements of MDS clinical Assistant Member practice are translatable to CMML, including which evidence has Malignant Hematology been generated from CMML-specific studies and which has not. H. Lee Moffitt Cancer Center & Research Institute This allows for an evidence-based approach to the treatment of 12902 Magnolia Drive CMML and identifies knowledge gaps in need of further study in Tampa, Florida 33612 a disease-specific manner. This review discusses the diagnosis, E-mail: [email protected] prognosis, and treatment of CMML, with the task of divorcing aspects of MDS practice that have not been demonstrated to be applicable to CMML and merging those that have been shown to be clinically similar. Introduction Chronic myelomonocytic leukemia (CMML) is a clonal hemato- logic malignancy characterized by absolute peripheral monocytosis, ineffective hematopoiesis, and an increased risk of transformation to acute myeloid leukemia. -
Idamycin PFS® Idarubicin Hydrochloride Injection
Idamycin PFS® idarubicin hydrochloride injection Rx only FOR INTRAVENOUS USE ONLY WARNINGS 1. IDAMYCIN PFS Injection should be given slowly into a freely flowing intravenous infusion. It must never be given intramuscularly or subcutaneously. Severe local tissue necrosis can occur if there is extravasation during administration. 2. As is the case with other anthracyclines the use of IDAMYCIN PFS can cause myocardial toxicity leading to congestive heart failure. Cardiac toxicity is more common in patients who have received prior anthracyclines or who have pre- existing cardiac disease. 3. As is usual with antileukemic agents, severe myelosuppression occurs when IDAMYCIN PFS is used at effective therapeutic doses. 4. It is recommended that IDAMYCIN PFS be administered only under the supervision of a physician who is experienced in leukemia chemotherapy and in facilities with laboratory and supportive resources adequate to monitor drug tolerance and protect and maintain a patient compromised by drug toxicity. The physician and institution must be capable of responding rapidly and completely to severe hemorrhagic conditions and/or overwhelming infection. 5. Dosage should be reduced in patients with impaired hepatic or renal function. (See DOSAGE AND ADMINISTRATION.) DESCRIPTION IDAMYCIN PFS Injection contains idarubicin hydrochloride and is a sterile, semi- synthetic, preservative-free solution (PFS) antineoplastic anthracycline for intravenous use. Chemically, idarubicin hydrochloride is 5, 12-Naphthacenedione, 9-acetyl-7-[(3- amino-2,3,6-trideoxy-α-L-lyxo-hexopyranosyl)oxy]-7,8,9,10-tetrahydro-6,9,11- trihydroxyhydrochloride, (7S-cis). The structural formula is as follows: C26 H27 NO9 .HCL M.W. 533.96 1 Reference ID: 3668307 IDAMYCIN PFS is a sterile, red-orange, isotonic parenteral preservative-free solution, available in 5 mL (5 mg), 10 mL (10 mg) and 20 mL (20 mg) single-use-only vials. -

Fludarabine Phosphate Powder for Solution for Injection Or Infusion
For the use only of a Registered Medical Practitioner or a Hospital or a Laboratory This package insert is continually updated. Please read carefully before using a new pack. Fludarabine Phosphate Powder for Solution for Injection or Infusion FLUDARA® NAME OF THE MEDICINAL PRODUCT Fludara 50 mg powder for solution for injection/infusion COMPOSITION Active ingredient: Each vial contains 50 mg fludarabine phosphate I.P. 1 ml of reconstituted solution for injection/infusion contains 25 mg fludarabine phosphate. Excipients: Mannitol, Sodium hydroxide (to adjust the pH to 7.7). INDICATIONS Fludara is indicated for the treatment of patients with B -cell chronic lymphocytic leukemia (CLL) who have not responded to at least one standard alkylating-agent containing regimen. DOSAGE AND METHOD OF ADMINISTRATION Method of administration Fludara must be administered only intravenously. No cases have been reported in which paravenously administered Fludara led to severe local adverse reactions. However, unintentional paravenous administration must be avoided. Dosage regimen Adults Fludara solution for injection/infusion should be administered under the supervision of a qualified physician experienced in the use of antineoplastic therapy. The recommended dose is 25 mg fludarabine phosphate/m² body surface given daily for 5 consecutive days every 28 days by the intravenous route. Each vial is to be made up in 2 ml water for injection. Each ml of the resulting solution for injection/infusion will contain 25 mg fludarabine phosphate (see section ‘Instructions for use/handling’). The required dose (calculated on the basis of the patient's body surface) is drawn up into a syringe. For intravenous bolus injection, this dose is further diluted into 10 ml of 0.9 % sodium chloride. -

SYN-40585 SYNRIBO Digital PI, Pil and IFU 5/2021 V3.Indd
SYN-40585 CONTRAINDICATIONS HIGHLIGHTS OF PRESCRIBING INFORMATION None. These highlights do not include all the information needed to use SYNRIBO safely and WARNINGS AND PRECAUTIONS effectively. See full prescribing information for SYNRIBO. • Myelosuppression: Severe and fatal thrombocytopenia, neutropenia and anemia. Monitor SYNRIBO® (omacetaxine mepesuccinate) for injection, for subcutaneous use hematologic parameters frequently (2.3, 5.1). Initial U.S. Approval: 2012 • Bleeding: Severe thrombocytopenia and increased risk of hemorrhage. Fatal cerebral hemorrhage and severe, non-fatal gastrointestinal hemorrhage (5.1, 5.2). INDICATIONS AND USAGE Hyperglycemia: Glucose intolerance and hyperglycemia including hyperosmolar non-ketotic SYNRIBO for Injection is indicated for the treatment of adult patients with chronic or accelerated • hyperglycemia (5.3). phase chronic myeloid leukemia (CML) with resistance and/or intolerance to two or more Embryo-Fetal Toxicity: Can cause fetal harm. Advise females of reproductive potential of the tyrosine kinase inhibitors (TKI) (1). • potential risk to a fetus and to use an effective method of contraception (5.4, 8.1, 8.3). DOSAGE AND ADMINISTRATION ADVERSE REACTIONS Induction Dose: 1.25 mg/m2 administered by subcutaneous injection twice daily for • Most common adverse reactions (frequency ≥ 20%): thrombocytopenia, anemia, neutropenia, 14 consecutive days of a 28-day cycle (2.1). diarrhea, nausea, fatigue, asthenia, injection site reaction, pyrexia, infection, and lymphopenia Maintenance Dose: 1.25 mg/m2 administered by subcutaneous injection twice daily for • (6.1). 7 consecutive days of a 28-day cycle (2.2). • Dose modifications are needed for toxicity (2.3). To report SUSPECTED ADVERSE REACTIONS, contact Teva Pharmaceuticals at 1-888-483-8279 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. -

Philadelphia Chromosome Unmasked As a Secondary Genetic Change in Acute Myeloid Leukemia on Imatinib Treatment
Letters to the Editor 2050 The ELL/MLLT1 dual-color assay described herein entails 3Department of Cytogenetics, City of Hope National Medical Center, Duarte, CA, USA and co-hybridization of probes for the ELL and MLLT1 gene regions, 4 each labeled in a different fluorochrome to allow differentiation Cytogenetics Laboratory, Seattle Cancer Care Alliance, between genes involved in 11q;19p chromosome translocations Seattle, WA, USA E-mail: [email protected] in interphase or metaphase cells. In t(11;19) acute leukemia cases, gain of a signal easily pinpoints the specific translocation breakpoint to either 19p13.1 or 19p13.3 and 11q23. In the References re-evaluation of our own cases in light of the FISH data, the 19p breakpoints were re-assigned in two patients, underscoring a 1 Harrison CJ, Mazzullo H, Cheung KL, Gerrard G, Jalali GR, Mehta A certain degree of difficulty in determining the precise 19p et al. Cytogenetic of multiple myeloma: interpretation of fluorescence in situ hybridization results. Br J Haematol 2003; 120: 944–952. breakpoint in acute leukemia specimens in the context of a 2 Thirman MJ, Levitan DA, Kobayashi H, Simon MC, Rowley JD. clinical cytogenetics laboratory. Furthermore, we speculate that Cloning of ELL, a gene that fuses to MLL in a t(11;19)(q23;p13.1) the ELL/MLLT1 probe set should detect other 19p translocations in acute myeloid leukemia. Proc Natl Acad Sci 1994; 91: 12110– that involve these genes with partners other than MLL. Accurate 12114. molecular classification of leukemia is becoming more im- 3 Tkachuk DC, Kohler S, Cleary ML. -

Fludarabine Phosphate (NSC 312878) Infusions for the Treatment of Acute Leukemia: Phase I and Neuropathological Study1
[CANCER RESEARCH 46, 5953-5958, November 1986] Fludarabine Phosphate (NSC 312878) Infusions for the Treatment of Acute Leukemia: Phase I and Neuropathological Study1 David R. Spriggs,2 Edward Stopa, Robert J. Mayer, William Schoene, and Donald W. Kufe3 Dana Farber Cancer Institute [D. R. S., R. J. M.. D. W. K.J and Department ofPathology, Brigham and Women 's Hospital [E. S., W. SJ, Boston, Massachusetts 0211S ABSTRACT a relationship between dose and lethargy. The schedule of drug administration in these studies was not a 5-day infusion. A Fludarabine phosphate (NSC 312878), an adenosine deaminase resist ant analogue of 9-/9-D-arabinofuranosyladenine, has entered clinical trials. single bolus was used in one study while the other used a single bolus followed by a 48-h infusion. Eleven patients with acute leukemia in relapse received 14 courses of fludarabine phosphate as a 5-day continuous infusion administered at Based on the myelosuppressive effects of fludarabine phos doses of 40 to 100 mg/m2/day. Toxicity was characterized by uniform phate in Phase I testing, we instituted a Phase I and II trial to myelosuppression, as well as occasional nausea, vomiting, and hepato- identify the toxicity and efficacy of fludarabine phosphate in toxicity. Three episodes of metabolic acidosis and lactic acidemia were the treatment of acute leukemia. The drug was administered as noted. In addition, three patients suffered neurotoxicity. Two of these a 5-day continuous infusion at a starting dose equivalent to the three patients had a severe neurotoxicity syndrome characterized by maximum tolerated dose reached in patients with solid tumors. -

NOVANTRONE (Mitoxantrone for Injection Concentrate) in Patients with Hepatic Insufficiency Is Not Established (See CLINICAL PHARMACOLOGY)
NOVANTRONE® mitoXANTRONE for injection concentrate WARNING NOVANTRONE® (mitoxantrone for injection concentrate) should be administered under the supervision of a physician experienced in the use of cytotoxic chemotherapy agents. NOVANTRONE® should be given slowly into a freely flowing intravenous infusion. It must never be given subcutaneously, intramuscularly, or intra-arterially. Severe local tissue damage may occur if there is extravasation during administration. (See ADVERSE REACTIONS, General, Cutaneous and DOSAGE AND ADMINISTRATION, Preparation and Administration Precautions). NOT FOR INTRATHECAL USE. Severe injury with permanent sequelae can result from intrathecal administration. (See WARNINGS, General) Except for the treatment of acute nonlymphocytic leukemia, NOVANTRONE® therapy generally should not be given to patients with baseline neutrophil counts of less than 1,500 cells/mm3. In order to monitor the occurrence of bone marrow suppression, primarily neutropenia, which may be severe and result in infection, it is recommended that frequent peripheral blood cell counts be performed on all patients receiving NOVANTRONE®. Cardiotoxicity: Congestive heart failure (CHF), potentially fatal, may occur either during therapy with NOVANTRONE® or months to years after termination of therapy. Cardiotoxicity risk increases with cumulative NOVANTRONE dose and may occur whether or not cardiac risk factors are present. Presence or history of cardiovascular disease, radiotherapy to the mediastinal/pericardial area, previous therapy with other anthracyclines or anthracenediones, or use of other cardiotoxic drugs may increase this risk. In cancer patients, the risk of symptomatic CHF was estimated to be 2.6% for patients receiving up to a cumulative dose of 140 mg/m2. To mitigate the cardiotoxicity risk with NOVANTRONE, prescribers should consider the following: NOVANTRONE mitoXANTRONE for injection 1 All Patients: - All patients should be assessed for cardiac signs and symptoms by history, physical examination, and ECG prior to start of NOVANTRONE® therapy. -

Intravesical Instillation of Azacitidine Suppresses Tumor Formation Through TNF-R1 and TRAIL-R2 Signaling in Genotoxic Carcinogen-Induced Bladder Cancer
cancers Article Intravesical Instillation of Azacitidine Suppresses Tumor Formation through TNF-R1 and TRAIL-R2 Signaling in Genotoxic Carcinogen-Induced Bladder Cancer Shao-Chuan Wang 1,2,3, Ya-Chuan Chang 2, Min-You Wu 2, Chia-Ying Yu 2, Sung-Lang Chen 1,2,3 and Wen-Wei Sung 1,2,3,* 1 Department of Urology, Chung Shan Medical University Hospital, Taichung 40201, Taiwan; [email protected] (S.-C.W.); [email protected] (S.-L.C.) 2 School of Medicine, Chung Shan Medical University, Taichung 40201, Taiwan; [email protected] (Y.-C.C.); [email protected] (M.-Y.W.); [email protected] (C.-Y.Y.) 3 Institute of Medicine, Chung Shan Medical University, Taichung 40201, Taiwan * Correspondence: [email protected] or fl[email protected]; Tel.: +886-4-2473-9595 Simple Summary: Approximately 70% of all bladder cancer is diagnosed as non-muscle invasive bladder cancer and can be treated by transurethral resection of the bladder tumor, followed by intravesical instillation chemotherapy. Bacille Calmette-Guérin (BCG) is the first-line agent for intravesical instillation, but its accessibility has been limited for years due to a BCG shortage. Here, our aim was to evaluate the therapeutic role of intravesical instillation of azacitidine, a DNA methyltransferase inhibitor, in bladder cancer. Cell model experiments showed that azacitidine inhibited TNFR1 downstream pathways to downregulate HIF-1α, claspin, and survivin. Concomitant Citation: Wang, S.-C.; Chang, Y.-C.; upregulation of the TRAIL R2 pathway by azacitidine ultimately drove the tumor cells to apoptosis. Wu, M.-Y.; Yu, C.-Y.; Chen, S.-L.; Sung, Rats with genotoxic carcinogen-induced bladder cancer showed a significantly reduced in vivo tumor W.-W. -

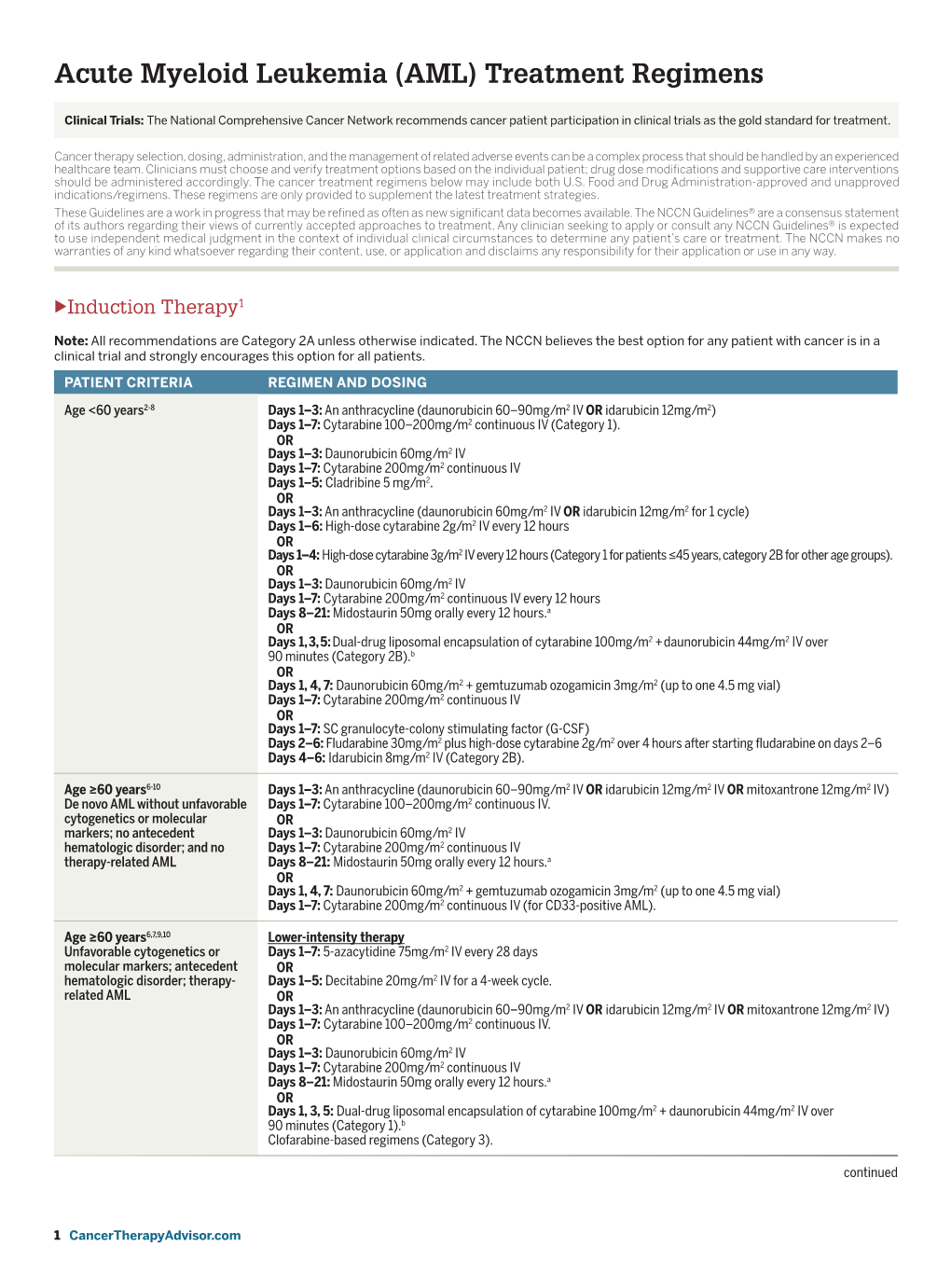
LEUKEMIA CHEMOTHERAPY REGIMENS (Part 1 of 2) the Selection, Dosing, and Administration of Anti-Cancer Agents and the Management of Associated Toxicities Are Complex
LEUKEMIA CHEMOTHERAPY REGIMENS (Part 1 of 2) The selection, dosing, and administration of anti-cancer agents and the management of associated toxicities are complex. Drug dose modifications and schedule and initiation of supportive care interventions are often necessary because of expected toxicities and because of individual patient variability, prior treatment, and comorbidities. Thus, the optimal delivery of anti-cancer agents requires a healthcare delivery team experienced in the use of such agents and the management of associated toxicities in patients with cancer. The chemotherapy regimens below may include both FDA-approved and unapproved uses/regimens and are provided as references only to the latest treatment strategies. Clinicians must choose and verify treatment options based on the individual patient. REGIMEN DOSING Acute Myeloid Leukemia (AML) Induction Therapy Cytarabine (Cytosar-U; ARA-C) + Days 1–3: An anthracycline (eg, daunorubicin at least 60mg/m2/day IV, an anthracycline idarubicin 10–12mg/m2/day IV, or mitoxantrone 10–12mg/m2/day IV), plus (daunorubicin [Cerubidine], Days 1–7: Cytarabine 100–200mg/m2/day continuous IV infusion. idarubicin [Idamycin], OR mitoxantrone [Novantrone])1, 2 Days 1–3: An anthracycline (eg, daunorubicin 45mg/m2/day IV, idarubicin 12mg/m2/day IV, or mitoxantrone 12mg/m2/day IV), plus Days 1–7: Cytarabine 100mg/m2/day continuous IV infusion. Intermediate-dose cytarabine3 Cycle 1 Days 1–7: Cytarabine 200mg/m2/day continuous IV infusion, plus Days 5–6: Idarubicin 12mg/m2/day IV. Cycle 2 Days 1–6: Cytarabine 1,000mg/m2 continuous IV infusion for 3 hrs twice daily, plus Days 3, 5 and 7: Amsacrine 120mg/m2/day.