Implementation of a Comprehensive HIV Prevention Intervention for Men Who Have Sex with Men in Malawi: Assessment of Feasibility and Impact
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

African Dialects
African Dialects • Adangme (Ghana ) • Afrikaans (Southern Africa ) • Akan: Asante (Ashanti) dialect (Ghana ) • Akan: Fante dialect (Ghana ) • Akan: Twi (Akwapem) dialect (Ghana ) • Amharic (Amarigna; Amarinya) (Ethiopia ) • Awing (Cameroon ) • Bakuba (Busoong, Kuba, Bushong) (Congo ) • Bambara (Mali; Senegal; Burkina ) • Bamoun (Cameroons ) • Bargu (Bariba) (Benin; Nigeria; Togo ) • Bassa (Gbasa) (Liberia ) • ici-Bemba (Wemba) (Congo; Zambia ) • Berba (Benin ) • Bihari: Mauritian Bhojpuri dialect - Latin Script (Mauritius ) • Bobo (Bwamou) (Burkina ) • Bulu (Boulou) (Cameroons ) • Chirpon-Lete-Anum (Cherepong; Guan) (Ghana ) • Ciokwe (Chokwe) (Angola; Congo ) • Creole, Indian Ocean: Mauritian dialect (Mauritius ) • Creole, Indian Ocean: Seychelles dialect (Kreol) (Seychelles ) • Dagbani (Dagbane; Dagomba) (Ghana; Togo ) • Diola (Jola) (Upper West Africa ) • Diola (Jola): Fogny (Jóola Fóoñi) dialect (The Gambia; Guinea; Senegal ) • Duala (Douala) (Cameroons ) • Dyula (Jula) (Burkina ) • Efik (Nigeria ) • Ekoi: Ejagham dialect (Cameroons; Nigeria ) • Ewe (Benin; Ghana; Togo ) • Ewe: Ge (Mina) dialect (Benin; Togo ) • Ewe: Watyi (Ouatchi, Waci) dialect (Benin; Togo ) • Ewondo (Cameroons ) • Fang (Equitorial Guinea ) • Fõ (Fon; Dahoméen) (Benin ) • Frafra (Ghana ) • Ful (Fula; Fulani; Fulfulde; Peul; Toucouleur) (West Africa ) • Ful: Torado dialect (Senegal ) • Gã: Accra dialect (Ghana; Togo ) • Gambai (Ngambai; Ngambaye) (Chad ) • olu-Ganda (Luganda) (Uganda ) • Gbaya (Baya) (Central African Republic; Cameroons; Congo ) • Gben (Ben) (Togo -

Botswana Ministry of Works and Comwunications
FINAL REPORT REPUBLIC OF BOTSWANA MINISTRY OF WORKS AND COMWUNICATIONS BOTSWANA - ZAMBIA ROAD PROJECT AID LOAN NO. 69o-T001 NATA - KAZUNGU-A I(OAD "PANDAMATENGA ACCESS ROAD CHOBE RIVER BY - PASS ROAD JULY 1978 Iq TA S TIPPET-m-S-ABBETT-MCCARFHY -STRATTON ENGINIEERSAND ARCHITECTS NEW YO:RK GABORONE FINAL REPORT REPUBLIC OF BOTSWANA MINISTRY OF WORKS AND COMMUNICATIONS BOTSWANA -ZAMBIA ROAD PROJECT AID LOAN NO. 690-H-001 NATA - KAZUNGULA ROAD PANDAMATENGA ACCESS ROAD CHOBE RIVER BY - PASS ROAD JULY 1978 TAMS TIPPETTS-ABB ETT-McCARTHY-STRATTON ENGINEERS AND ARCHITECTS NEW YORK GABORONE TABLEOF CONTENTS PAGE I. INTRODUCTION I A. DESCRIPTION OF PROJECT 1 B. FUNDING 2 C. CONTRACTUAL ARRANGEMENTS 2 D. MODIFICATIONS OF CONTRACT 2 II. STAFFING 4 III. TRAINING 4 IV. CONSTRUCTION EQUIPMENT 4 V. MATERIALS UTILIZED 5 A. SOILS 5 B. WATER 5 VI. PROTECT HISTORY 5 A. GENERAL 5 B. SEQUENCE OF EVENTS 6 C. PROJECT SCHEDULING AND DELAYS 9 D. REMEDIAL ACTION 11 E. PICTORIAL HISTORY 11 VII. FINANCIAL SUMMARY 12 APPENDICES A. CONSTRUCTION EQUIPMENT B. SOILS AND MATERIALS C. WATER WELL LOCATIONS D. SYNOPSIS OF KEY CORRESPONDENCE E. PROJECT PHOTOGRAPHS LIST OF FIGURES FIG. 1 ........................ LOCATION MAP FIG. 2 ........................ CONSTRUCTION PROGRESS CHART FIG; B-i THRU B-4 ............. MATERIALS UTILIZATION DIAGRAMS FIG. B-5 THRU B-13 ............ AVERAGE GRADATION CURVES UNITED STATES GOVERNMENT INSTRUCTIONS use routing symbols whenever possible. 2- a emo SENDER: Use brief, informal language. Conserve space. Subject Final Report Botswana -,Zambia Road Project Forward original and one copy. RECEIVER: Reply below the message, keep one copy, return one copy. DATE OF MESSAGE Routing Symbol TO fiS/ENGR kl7 4 C&RSC. -

South Africa and Botswana Troops Arrive MOZAMBIQUE News Reports & Clippings
MOZAMBIQUE News reports & clippings 558 22 July 2021 Editor: Joseph Hanlon ( [email protected]) To subscribe or unsubscribe: https://bit.ly/Moz-sub This newsletter can be cited as "Mozambique News Reports & Clippings" Articles may be freely reprinted but please cite the source. Extensive links and privacy statement at the end of this newsletter. __________________________________________________________________________ In this issue Cabo Delgado + South Africa & Botswana troops arrive + Rwanda troops already in action + Mozambique troops hold Mueda security zone + Unheard warnings from Sahel and Nigeria + US backs land clearance by moving Biibiza + Mine-owners go offshore and secret Other news + 4 South African spies caught + Profiting from a failing state + Guebuza to be witness at debts trial __________________________________________________________________________ South Africa and Botswana troops arrive The first contingent of South African soldiers flew into Pemba Monday (19 July) with Hornet lightweight armoured vehicles used by South African Special Forces. A plane from Botswana also brought troops and equipment. Rwandan troops are already in action. The arrival was confirmed by Defence Ministry spokesman Coronel Omar Saranga, who said these were preparation forces and not the full 3000-soldier SADC contingent. He added that the SADC force commander “is South African and his name is Xolani Mankayi. He is already in Mozambique." (Daily Maverick, DefenceWeb, Radio Moçambique - 21 July; AIM 22 July) The Zimbabwe army has put on standby a contingent of troops to be deployed in Cabo Delgado as part of he SADC force. Military sources told NewZimbabwe.com (22 July) they received a radio communication advising them that they were now on standby and should await deployment orders. -

Evolution of the EU List of Tax Havens
Evolution of the EU list of tax havens 22 February 2021 12 jurisdictions 9 jurisdictions American Samoa, Anguilla, Australia, Barbados, Botswana, Eswatini, Jamaica, Jordan, Maldives, Dominica, Fiji, Guam, Palau, Thailand, Turkey Panama, Samoa, Seychelles, Trinidad and Tobago, Vanuatu, US Virgin Islands Moved from black list to grey list Barbados Added to the black list Removed from the grey list Dominica Morocco, Namibia and Saint Lucia 6 October 12 jurisdictions 2020 10 jurisdictions American Samoa, Anguilla, Australia, Botswana, Eswatini, Jordan, Maldives, Morocco, Namibia, Barbados, Fiji, Guam, Palau, Saint Lucia, Thailand, Turkey Panama, Samoa, Seychelles, Trinidad and Tobago, Vanuatu, US Virgin Islands 9 jurisdictions Moved from grey list to black list Anguilla American Samoa, Belize, Fiji, Guam, Oman, Samoa, Trinidad and Tobago, Vanuatu, Added to the black list Removed from the grey list US Virgin Islands Barbados Bosnia and Herzegovina, Mongolia Removed from the blacklist Cayman Islands, Oman Taxation and Customs Union 18 February 12 jurisdictions 2020 13 jurisdictions American Samoa, Cayman Anguilla, Australia, Bosnia and Herzegovina, Botswana, Eswatini, Jordan, Islands, Fiji, Guam, Palau, Maldives, Morocco, Mongolia, Namibia, Saint Lucia, Thailand and Turkey Panama, Samoa, Seychelles, Oman, Trinidad and Tobago, Vanuatu, US Virgin Islands Moved from grey list to black list Cayman Islands, Palau and Seychelles Added to the black list Removed from the grey list Panama Antigua and Barbuda, Armenia, Bahamas, Barbados, Belize, Bermuda, -
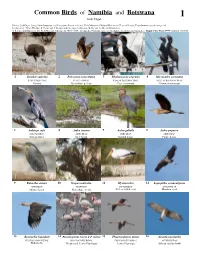
Common Birds of Namibia and Botswana 1 Josh Engel
Common Birds of Namibia and Botswana 1 Josh Engel Photos: Josh Engel, [[email protected]] Integrative Research Center, Field Museum of Natural History and Tropical Birding Tours [www.tropicalbirding.com] Produced by: Tyana Wachter, R. Foster and J. Philipp, with the support of Connie Keller and the Mellon Foundation. © Science and Education, The Field Museum, Chicago, IL 60605 USA. [[email protected]] [fieldguides.fieldmuseum.org/guides] Rapid Color Guide #584 version 1 01/2015 1 Struthio camelus 2 Pelecanus onocrotalus 3 Phalacocorax capensis 4 Microcarbo coronatus STRUTHIONIDAE PELECANIDAE PHALACROCORACIDAE PHALACROCORACIDAE Ostrich Great white pelican Cape cormorant Crowned cormorant 5 Anhinga rufa 6 Ardea cinerea 7 Ardea goliath 8 Ardea pupurea ANIHINGIDAE ARDEIDAE ARDEIDAE ARDEIDAE African darter Grey heron Goliath heron Purple heron 9 Butorides striata 10 Scopus umbretta 11 Mycteria ibis 12 Leptoptilos crumentiferus ARDEIDAE SCOPIDAE CICONIIDAE CICONIIDAE Striated heron Hamerkop (nest) Yellow-billed stork Marabou stork 13 Bostrychia hagedash 14 Phoenicopterus roseus & P. minor 15 Phoenicopterus minor 16 Aviceda cuculoides THRESKIORNITHIDAE PHOENICOPTERIDAE PHOENICOPTERIDAE ACCIPITRIDAE Hadada ibis Greater and Lesser Flamingos Lesser Flamingo African cuckoo hawk Common Birds of Namibia and Botswana 2 Josh Engel Photos: Josh Engel, [[email protected]] Integrative Research Center, Field Museum of Natural History and Tropical Birding Tours [www.tropicalbirding.com] Produced by: Tyana Wachter, R. Foster and J. Philipp, -

Botswana Stability in Sub-Saharan Africa
Botswana Stability in Sub-Saharan Africa Botswana has transitioned from a dependent aid recipient to middle-income status with a small aid portfolio. Today it is now one of the most stable and economically prosperous nations in sub-Saharan Africa. However, when it gained independence in 1966, Botswana had a GDP per capita that ranked among the lowest in the world. Subsistence farming made up a large portion of the country’s economy. At the time, the United States provided it with approximately $10 million per year in foreign assistance, with that number reaching a high of over $100 million in 1972, largely in economic and agricultural development aid. In addition, shortly after independence, Botswana also began a series of reforms that jumpstarted its economy, endowing it with a greater level of economic autonomy. These changes included sweeping liberal economic and political reforms, the cornerstones of which were a democratic government, competitive elections, and strong economic institutions that promoted fair and free market practices. In the 1970s, Botswana became a major exporter of diamonds, and the government claimed 50% ownership over Debswana, the country’s main mining company. Because of this, Botswana experienced a significant boom: from 1966-1990, growth averaged 9% each year, propelling Botswana to become one of the most prosperous nations in sub-Saharan Africa. This economic strength also developed within a system of governance that included low levels of corruption. Diamonds rose to become 85% of total export earnings, over 60% of total exports, a quarter of the nation’s GDP, and the source of one third of government revenue. -

Essential Information Botswana, South Africa, Zambia & Zimbabwe
ESSENTIAL INFORMATION BOTSWANA, SOUTH AFRICA, ZAMBIA & ZIMBABWE PASSPORT AND VISA INFORMATION Your passport needs to be valid for at least six (6) months after your journey ends, and should have a minimum of thirteen (10) blank visa pages for entry and exit stamps. Note: you will need two (2) consecutive blank visa pages for each entry into South Africa. Botswana and South Africa Holders of U.S. and Canadian passports are not required to obtain a tourist visa for entry into either Botswana or South Africa for stays of up to 90 days. Zambia and Zimbabwe A tourist visa is required for U.S. and Canadian passport holders for entry into Zambia and Zimbabwe. A&K recommends obtaining a KAZA UNIVISA (valid for both countries) on arrival. KAZA UNIVISA: Can be obtained on arrival at certain ports of entry in either Zambia or Zimbabwe. It is valid for 30 days and allows multiple entries into either country. The current fee is USD $50 (subject to change without notice). This amount must be paid in cash in U.S. dollars. The allowable ports of entry include: Zambia • KK International Airport Lusaka • Harry Mwaanga International Airport Livingstone • Victoria Falls Land Border with Zimbabwe • Kazangula Land Border with Botswana Zimbabwe • Harare International Airport • Victoria Falls International Airport • Victoria Falls Land Border with Zambia • Kazangula Land Border with Botswana Availability of the KAZA UNIVISA can be sporadic. In the event the KAZA UNIVSA is unavailable, individual visas for Zambia and Zimbabwe can be obtained on arrival in each country as follows: Zambia • Single-entry visa for Zambia: USD $50. -

Inequality, Patronage, Ethnic Politics and Decentralization in Kenya and Botswana: an Analysis of Factors That Increase the Likelihood of Ethnic Conflict
Western Michigan University ScholarWorks at WMU Master's Theses Graduate College 8-2019 Inequality, Patronage, Ethnic Politics and Decentralization in Kenya and Botswana: An Analysis of Factors that Increase the Likelihood of Ethnic Conflict Rei Gordon Follow this and additional works at: https://scholarworks.wmich.edu/masters_theses Part of the Political Science Commons Recommended Citation Gordon, Rei, "Inequality, Patronage, Ethnic Politics and Decentralization in Kenya and Botswana: An Analysis of Factors that Increase the Likelihood of Ethnic Conflict" (2019). Master's Theses. 4722. https://scholarworks.wmich.edu/masters_theses/4722 This Masters Thesis-Open Access is brought to you for free and open access by the Graduate College at ScholarWorks at WMU. It has been accepted for inclusion in Master's Theses by an authorized administrator of ScholarWorks at WMU. For more information, please contact [email protected]. INEQUALITY, PATRONAGE, ETHNIC POLITICS AND DECENTRALIZATION IN KENYA AND BOTSWANA: AN ANALYSIS OF FACTORS THAT INCREASE THE LIKLIHOOD OF ETHNIC CONFLICT IN DIVERSE SOCIETIES by Rei Gordon A thesis submitted to the Graduate College in fulfillment of the requirements for the degree of Master of Arts Political Science Western Michigan University August 2019 Thesis Committee: Jim Butterfield, Ph.D., Chair John Clark, Ph.D. Mahendra Lawoti, Ph.D. Copyright by Rei Gordon 2019 ACKNOWLEDGEMENTS I would like to thank the three members of my committee for their dedication to teaching and to their students. The topic of this thesis is greatly influenced by the courses they have taught and the example they have set as scholars of political science. The subjects of their research and the manner in which they interact with students demonstrates the power of our field to positively impact those around us. -

Botswana's Success: the Critical Role of Post-Colonial Policy
Working Paper 41 Explaining Botswana’s Success: The Critical Role of Post-Colonial Policy * SCOTT BEAULIER Abstract Development economists are shifting their focus away from cross-country empirical studies (Barro, 1997) towards case studies and “analytic narratives” (Rodrik 2003; Bates et al. 1998). Instead of trying to explain all of sub-Saharan Africa’s problems in one grand sweep, economists are engaging in more focused studies of particular nations. Their hope is that by clearly understanding the particulars, broader conclusions can be drawn. This paper is inspired by the “analytical narrative” turn in economics. The paper seeks to explain the key determinants of Botswana’s economic miracle. As a landlocked country in the middle of sub-Saharan Africa, Botswana should not be growing; yet, Botswana has been one of the fastest growing countries in the world for the past 30 years. Daron Acemoglu, Simon Johnson, and James Robinson (2003) suggest that Botswana’s success can be attributed to Botswana’s “good institutions,” but this explanation begs the question of why Botswana adopted “good institutions” in the first place. To understand why the “good institutions” were established in Botswana, we must look closely at the history of Botswana’s development. By studying the history of Botswana’s development, we can begin to understand what choices other nations must make to truly reform. JEL Classifications: O10, O55, R11 * Scott Beaulier is a PhD candidate in Economics and a Global Prosperity Initiative (GPI) Fellow at the Mercatus Center. He thanks Peter Boettke, Bryan Caplan, Tyler Cowen, Eric Crampton, Benjamin Powell, John Robert Subrick, Richard Wagner, the participants at the 2003 Association of Private Enterprise Education conference in Las Vegas, the participants at the Mercatus Center “brown bag” series, and an anonymous referee for helpful comments and criticism. -

Namibia & Botswana Detailed Itinerary
NAMIBIA & BOTSWANA MAY 16 – 30, 2020 DETAILED ITINERARY Southern Africa is unrivaled in its extreme diversity of eco-systems. Namibia’s Etosha National Park is a literal Noah’s ark, with its many life-sustaining waterholes attracting wildlife from miles around including rhino, elephant, lion, zebra and a wide variety of antelope species. The spectacular beauty of Namibia’s Namib Naukluft National Park astonishes with its landscape of red dunes, where the ever-changing colors create a photographer’s dream. In Botswana’s Okavango Delta, experience an unparalleled safari experience. In this remote and extensive wildlife reserve, a myriad of bird and wildlife awaits, with vast herds of plains game and the predators that follow. Watch a large herd of elephant drink from a river as one of Africa’s spectacular sunsets plays out behind them, then embark on a night game drive in search of nocturnal species and the elusive leopard. Join your Harvard study leader, fellow Harvard alumni and like-minded, sophisticated travelers on this journey through Namibia and Botswana. GROUP SIZE: 8 – 10 guests PRICING: $16,995 per person double occupancy / $18,995 single occupancy STUDY LEADER: Zarin Machanda Associate in the Department of Human Evolutionary Biology at Harvard University and Assistant Professor in Anthropology at Tufts University. Zarin received her PhD from the Department of Human Evolutionary Biology at Harvard University. Her research revolves around understanding the factors that shape the quality and development of social relationships among primates and specifically chimpanzees. Zarin has spent the last 14 years working with both captive and wild chimpanzees. -

Executive Summary Botswana Is a Stable, Democratic Country Which
Executive Summary Botswana is a stable, democratic country which has historically enjoyed among the highest economic growth rates in the world. Botswana has consistently ranked number one in Africa on Transparency International’s anti-corruption index, and its 56th place ranking on the 2014 annual World Bank/IFC Doing Business compares favorably to all but three other sub-Saharan African countries. Botswana’s per capita income of $16,105 (based on purchasing power parity) makes it an Upper Middle-Income Country according to the World Bank. Botswana’s export-driven economy is highly correlated with global economic trends. In the aftermath of the global financial crisis, Botswana’s economy went into recession, posting a negative GDP growth rate of 4.9%. Weakened demand for mineral resources, particularly diamonds, hampered growth in 2011 and 2012 when GDP growth was 6.1% and 4.2% (est.), respectively. Botswana maintains a conservative fiscal policy and low levels of foreign debt. In February of 2014, the Government of Botswana (GoB) reported an unanticipated $45 million USD surplus for FY 2013. Better-than-expected diamond and customs revenues helped recharge the GoB’s current account, which was projected to be in deficit as late as November of last year. The 4.1% year-end inflation rate in 2013 was the lowest since 1971. Botswana’s trade balance is largely tied to the global demand for diamonds. As of December 31, 2013, Moody’s and S&P rate Botswana’s sovereign debt as A2 and A-, respectively. Government spending has traditionally played a large role in Botswana’s economy. -

Botswana & Namibia 4
©Lonely Planet Publications Pty Ltd Botswana & Namibia Victoria Falls p183 Namibia p215 Botswana p44 Anthony Ham, Trent Holden PLAN YOUR TRIP ON THE ROAD Welcome to Botswana BOTSWANA . 44 Nogatsaa/Tchinga Area . 87 & Namibia . 4 Gaborone . 45 Savuti . 87 Map . 6 Greater Gaborone . 55 Linyanti Marshes . 90 Botswana Matsieng Rock Carvings . 55 Okavango Delta . 93 & Namibia’s Top 16 . 8 Mochudi . 55 Maun . 93 Need to Know . 16 Gabane . .. 56 Shorobe . 105 Eastern Delta . 105 If You Like… . 18 Manyana . 57 Thamaga . 57 Inner Delta . 107 Month by Month . 22 Mokolodi Nature Reserve . 57 Moremi Game Reserve . 112 Itineraries . 24 Otse . 58 Okavango Panhandle . .. 117 Planning a Safari . 29 Kanye . 58 Northwestern Botswana . 121 Eastern Botswana . 58 Regions at a Glance . 39 Tsodilo Hills . 121 Palapye . 58 Lake Ngami . 124 Serowe . 59 Aha Hills . 124 Khama Rhino Sanctuary . 61 Gcwihaba Tswapong Hills . 62 (Drotsky’s Cave) . 124 Francistown . .. 63 Kalahari . 125 CARGE/SHUTTERSTOCK © CARGE/SHUTTERSTOCK Tuli Block . 66 Ghanzi . 125 Makgadikgadi & D’kar . 127 Nxai Pans . 68 Central Kalahari Nata . 68 Game Reserve . 129 Gweta . 70 Khutse Game Reserve . 135 Sowa Pan . 71 Kang . 137 Ntwetwe Pan . 73 Kgalagadi Transfrontier Makgadikgadi Pans Park . 138 National Park . 75 Understand Botswana . 144 Nxai Pans National Park . 77 Botswana Today . 144 OSTRICH, ETOSHA Chobe National Park . 79 History . 146 NATIONAL PARK P250 Kasane . 79 People of Botswana . 150 Chobe Riverfront . 84 Religion . 153 2630BEN/SHUTTERSTOCK © 2630BEN/SHUTTERSTOCK HIMBA WOMAN, NAMIBIA P348 Contents SURVIVAL GUIDE Arts & Crafts . 153 The North . 255 Health . 380 Architecture . 154 Kavango Region . 258 Language . 386 Dance . 154 The Caprivi Strip .