Pyogenic Gram Positive Cocci
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

USMLE – What's It
Purpose of this handout Congratulations on making it to Year 2 of medical school! You are that much closer to having your Doctor of Medicine degree. If you want to PRACTICE medicine, however, you have to be licensed, and in order to be licensed you must first pass all four United States Medical Licensing Exams. This book is intended as a starting point in your preparation for getting past the first hurdle, Step 1. It contains study tips, suggestions, resources, and advice. Please remember, however, that no single approach to studying is right for everyone. USMLE – What is it for? In order to become a licensed physician in the United States, individuals must pass a series of examinations conducted by the National Board of Medical Examiners (NBME). These examinations are the United States Medical Licensing Examinations, or USMLE. Currently there are four separate exams which must be passed in order to be eligible for medical licensure: Step 1, usually taken after the completion of the second year of medical school; Step 2 Clinical Knowledge (CK), this is usually taken by December 31st of Year 4 Step 2 Clinical Skills (CS), this is usually be taken by December 31st of Year 4 Step 3, typically taken during the first (intern) year of post graduate training. Requirements other than passing all of the above mentioned steps for licensure in each state are set by each state’s medical licensing board. For example, each state board determines the maximum number of times that a person may take each Step exam and still remain eligible for licensure. -
Known Infectious Causes of Vasculitis in Man
PATHOGENESIS Known infectious causes of vasculitis in man STANLEY J. NAIDES, MD n array of pathogens is known to cause vasculi- and our ability to intervene in disease processes, have ren- tis in man.1,2 For several of these agents, vas- dered some causes of vasculitis far less common. culitis is the major manifestation of disease. The Amajority, however, typically present as infec- ■ VIRAL CAUSES OF VASCULITIS tious processes in which vasculitis is an occasional mani- Our knowledge of viral pathogenesis has exploded in the festation of disease. For many, vasculitis may be a compo- last quarter of the twentieth century, accelerated in large nent of disease pathogenesis but is not a prominent feature part by epidemics of “emerging” viral diseases. Hepatitis C of the clinical presentation. The various agents—viruses, virus, discovered in 1989, has worldwide prevalence.3 The bacteria, and fungi—share a common target, blood vessels. 10- to 20-year latent period before hepatic or rheumatic The involvement of vessels may be direct, with vascular manifestations of disease explains the increasing number structures serving as targets. Many infectious pathogens of cases of hepatitis C virus–mediated vasculitis currently have tissue tropism that includes endothelium. Other being seen in the United States following the epidemic of agents may bind to the vessel wall because the vascular en- new infections in the 1980s.4 Prior to the discovery and dothelium expresses specific receptors for the pathogen or characterization of hepatitis C virus in the late 1980s, the another moiety with which the pathogen travels. Even triad of arthritis, palpable purpura, and type II cryoglobu- when the agent does not enter the endothelial cell, the im- linemia was given the sobriquet “essential mixed cryo- mune response to the agent may be focused at the vessel globulinemia” and considered an idiopathic vasculitis. -

Identification of Microorganisms Using Nucleic Acid Probes
Identification of Microorganisms Using Page 1 of 45 Nucleic Acid Probes Medical Policy An Independent Licensee of the Blue Cross and Blue Shield Association Title: Identification of Microorganisms Using Nucleic Acid Probes See Also: Influenza Virus Diagnostic Testing and Treatment in the Outpatient Setting Professional Institutional Original Effective Date: July 8, 2008 Original Effective Date: July 16, 2009 Revision Date(s): June 16, 2009; Revision Date(s): March 1, 2012; March 1, 2012; June 5, 2012; June 5, 2012; November 19, 2012; November 19, 2012; January 15, 2013; January 15, 2013; November 12, 2013 November 12, 2013 Current Effective Date: November 12, 2013 Current Effective Date: November 12, 2013 State and Federal mandates and health plan member contract language, including specific provisions/exclusions, take precedence over Medical Policy and must be considered first in determining eligibility for coverage. To verify a member's benefits, contact Blue Cross and Blue Shield of Kansas Customer Service. The BCBSKS Medical Policies contained herein are for informational purposes and apply only to members who have health insurance through BCBSKS or who are covered by a self-insured group plan administered by BCBSKS. Medical Policy for FEP members is subject to FEP medical policy which may differ from BCBSKS Medical Policy. The medical policies do not constitute medical advice or medical care. Treating health care providers are independent contractors and are neither employees nor agents of Blue Cross and Blue Shield of Kansas and are solely responsible for diagnosis, treatment and medical advice. If your patient is covered under a different Blue Cross and Blue Shield plan, please refer to the Medical Policies of that plan. -

Syphilis As Seen by a Hospital Physician
284 Prof. Monro?Syphilis as seen by a Hospital Physician. SYPHILIS AS SEEN BY A HOSPITAL PHYSICIAN* By T. K. MONRO, M.A., M.D., Professor of Medicine, University of Glasgow. \ " / Mr. President and Gentlemen,?I thank you heartily for the honour you have done me in inviting me to be Honorary President of this Faculty for the session which is now opening. I was duly informed by Dr. Wardlaw that my principal duty as incumbent of this honourable office was to deliver an address to the Faculty, and as his invitation reached me while I was on holiday, with other objects in view, I had time to contemplate the responsibility I had undertaken, and to consider how I was to face it. In getting over the usual initial difficulty as to the choice of a subject, some assistance was afforded me by the President's instruction that the address ought to be one for the general practitioner. Quite a number of subjects would be appropriate from this point of view. I should have been glad to say some- thing on oral sepsis, a condition often spoken of, and no doubt often wrongly blamed, but also apt to be overlooked. Dentists do not always realise how completely one may be misled by the absence of subjective and objective evidence; so that even an experienced man may pass as innocuous a tooth which subse- quent extraction shows to have disease at its root. Medical men sometimes make a mistake in the opposite direction, by insisting, without sufficient justification, on the removal of teeth, e.g., in epileptiform neuralgia. -

Immunology of Tuberculosis
Color code: Important in red Extra in blue Immunology of Tuberculosis Editing file Objectives ➢ To know how M. tuberculosis infection is contracted and its initial encounter with the immune system ➢ To understand the delayed type of hypersensitivity reaction against M. tuberculosis ➢ To be familiar with the possible outcomes of the infection with M. tuberculosis in immunocompetent and immunocompromised hosts ➢ To understand the basis of the tuberculin test and its importance in gauging immunity against M. tuberculosis Introduction to Tuberculosis ➢ Mycobacterium tuberculosis is the second most common infectious cause of death in adults worldwide, with an increasing incidence due to HIV. ➢ TB is transmitted through aerosols (airborne transmission) by coughing or sneezing and acquired mainly through inhalation. ➢ The clinical development of the disease depends solely on the effectiveness of the host’s innate and adaptive immune response to the infection. If the immune response is functioning well, the clinical disease has little to no chance of developing. Tuberculosis is able to withstand the body’s immune response after being phagocytosed by several ways, including: Virulence factors Host factors The lipid-rich Waxy outer coat blocks Resistance to reactive oxygen intermediates. phagocytic enzymes. Catalase-peroxidase resists the host cell Inhibition of phagosome-lysosome fusion oxidative response. The glycolipid Lipoarabinomannan (LAM) Inhibition of phagosome acidification. Stimulates cytokines, resists the host oxidative (prevents digestion -

A Review of Primary Vasculitis Mimickers Based on the Chapel Hill Consensus Classification
Hindawi International Journal of Rheumatology Volume 2020, Article ID 8392542, 11 pages https://doi.org/10.1155/2020/8392542 Review Article A Review of Primary Vasculitis Mimickers Based on the Chapel Hill Consensus Classification Farah Zarka ,1 Charles Veillette ,1 and Jean-Paul Makhzoum 2 1Hôpital du Sacré-Cœur de Montreal, University of Montreal, Canada 2Vasculitis Clinic, Department of Internal Medicine, Hôpital du Sacré-Coeur de Montreal, University of Montreal, Canada Correspondence should be addressed to Jean-Paul Makhzoum; [email protected] Received 10 July 2019; Accepted 7 January 2020; Published 18 February 2020 Academic Editor: Charles J. Malemud Copyright © 2020 Farah Zarka et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Primary systemic vasculitides are rare diseases that may manifest similarly to more commonly encountered conditions. Depending on the size of the vessel affected (large vessel, medium vessel, or small vessel), different vasculitis mimics must be considered. Establishing the right diagnosis of a vasculitis mimic will prevent unnecessary immunosuppressive therapy. 1. Introduction 2. Large-Vessel Vasculitis Mimics Vasculitides are rare heterogenous diseases that affect vessel Large-vessel vasculitis (LVV) is an inflammatory vascu- walls as the main site of inflammation. Organs affected vary lopathy affecting large arteries; giant cell arteritis (GCA) depending on the type and size of blood vessels involved and Takayasu’s arteritis (TAK) are the two main docu- [1]. Autoimmune vasculitis can be primary (idiopathic) or mented variants, each with their own characteristic fea- secondary to an underlying disease. -
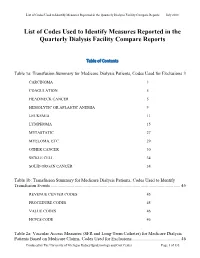
List of Codes Used to Identify Measures Reported in the QDFC
List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports July 2018 List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports Table of Contents Table 1a: Transfusion Summary for Medicare Dialysis Patients, Codes Used for Exclusions 3 CARCINOMA 3 COAGULATION 5 HEAD/NECK CANCER 5 HEMOLYTIC OR APLASTIC ANEMIA 9 LEUKEMIA 11 LYMPHOMA 15 METASTATIC 27 MYELOMA, ETC. 29 OTHER CANCER 30 SICKLE CELL 34 SOLID ORGAN CANCER 34 Table 1b: Transfusion Summary for Medicare Dialysis Patients, Codes Used to Identify Transfusion Events .................................................................................................................. 45 REVENUE CENTER CODES 45 PROCEDURE CODES 45 VALUE CODES 46 HCPCS CODE 46 Table 2a: Vascular Access Measures (SFR and Long-Term Catheter) for Medicare Dialysis Patients Based on Medicare Claims, Codes Used for Exclusions ........................................... 46 Produced by The University of Michigan Kidney Epidemiology and Cost Center Page 1 of 135 List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports July 2018 COMA 46 END STAGE LIVER DISEASE 48 METASTATIC CANCER 48 Table 2b: Standardized Fistulae Rate (SFR) for Medicare Dialysis Patients Based on Medicare Claims, Codes Used for Prevalent Comorbidities Adjusted in Model .................................... 50 ANEMIA 50 CORONARY ARTERY DISEASE 52 CONGESTIVE HEART FAILURE 55 CEREBROVASCULAR DISEASE 56 CHRONIC OBSTRUCTIVE PULMONARY DISEASE 68 DIABETES 69 DRUG DEPENDENCE 79 INFECTIONS (NON-VASCULAR ACCESS-RELATED): 93 PERIPHERAL VASCULAR DISEASE (INCLUDES ARTERIAL, VENOUS AND NONSPECIFIC DISEASES) 124 Table 3: Dialysis Adequacy ................................................................................................... -
Lecture 1 ― INTRODUCTION INTO MICROBIOLOGY
МИНИСТЕРСТВО ЗДРАВООХРАНЕНИЯ РЕСПУБЛИКИ БЕЛАРУСЬ УЧРЕЖДЕНИЕ ОБРАЗОВАНИЯ «ГОМЕЛЬСКИЙ ГОСУДАРСТВЕННЫЙ МЕДИЦИНСКИЙ УНИВЕРСИТЕТ» Кафедра микробиологии, вирусологии и иммунологии А. И. КОЗЛОВА, Д. В. ТАПАЛЬСКИЙ МИКРОБИОЛОГИЯ, ВИРУСОЛОГИЯ И ИММУНОЛОГИЯ Учебно-методическое пособие для студентов 2 и 3 курсов факультета по подготовке специалистов для зарубежных стран медицинских вузов MICROBIOLOGY, VIROLOGY AND IMMUNOLOGY Teaching workbook for 2 and 3 year students of the Faculty on preparation of experts for foreign countries of medical higher educational institutions Гомель ГомГМУ 2015 УДК 579+578+612.017.1(072)=111 ББК 28.4+28.3+28.073(2Англ)я73 К 59 Рецензенты: доктор медицинских наук, профессор, заведующий кафедрой клинической микробиологии Витебского государственного ордена Дружбы народов медицинского университета И. И. Генералов; кандидат медицинских наук, доцент, доцент кафедры эпидемиологии и микробиологии Белорусской медицинской академии последипломного образования О. В. Тонко Козлова, А. И. К 59 Микробиология, вирусология и иммунология: учеб.-метод. пособие для студентов 2 и 3 курсов факультета по подготовке специалистов для зарубежных стран медицинских вузов = Microbiology, virology and immunology: teaching workbook for 2 and 3 year students of the Faculty on preparation of experts for foreign countries of medical higher educa- tional institutions / А. И. Козлова, Д. В. Тапальский. — Гомель: Гом- ГМУ, 2015. — 240 с. ISBN 978-985-506-698-0 В учебно-методическом пособии представлены тезисы лекций по микробиоло- гии, вирусологии и иммунологии, рассмотрены вопросы морфологии, физиологии и генетики микроорганизмов, приведены сведения об общих механизмах функциони- рования системы иммунитета и современных иммунологических методах диагности- ки инфекционных и неинфекционных заболеваний. Приведены сведения об этиоло- гии, патогенезе, микробиологической диагностике и профилактике основных бакте- риальных и вирусных инфекционных заболеваний человека. Может быть использовано для закрепления материала, изученного в курсе микро- биологии, вирусологии, иммунологии. -

Tabes Dorsalis and Perforated Duodenal Ulcer J
i6o Postgrad Med J: first published as 10.1136/pgmj.37.425.160 on 1 March 1961. Downloaded from POSTGRAD. MED. J. (1961), 37, i60 TABES DORSALIS AND PERFORATED DUODENAL ULCER J. P. LAWSON, M.B., Ch.B. Late Senior House Officer in Medicine, Crumpsall Hospital, Manchester Senior House Oficer in Radiology, David Lewis Northern Hospital, Liverpool 3 IT is well recorded that tabes dorsalis can mask between the shoulder blades whilst standing in a bus serious visceral disease. Wilson mentions queue. This was shortly followed by a bout of vomiting (1954) and sweating. There was no dyspncea, pain in the chest that tabes can disrupt nervous pathways so as to or abdominal pain. The patient was able to make his produce a visceral analgesia capable of masking own way home on foot. serious abdominal disease. At home he took a Sedlitz powder, which was followed by three further attacks of vomiting and four Connor (I91o) published a case of a brakeman, loose bowel actions. There was no blood in either aged 42, who died in hospital following an acute vomitus or faeces. The pain spread to both shoulder febrile attack and vomiting. There had been no tips, where it persisted and was the cause of his attend- abdominal tenderness or to ance at the casualty department. pain, rigidity explain Four years previously he had developed a similar the condition but autopsy revealed a perforated attack of sweating and stated that he had also vomited appendix abscess and peritonitis. blood. At this time he was apparently found to be from and was trans- Hanser (I9I9) recorded the case of a tabetic suffering pulmonary tuberculosis, by copyright. -

Diagnosis One To
Diagnosis One-to-One I9cm I9 Long Desc I10cm I10 Long Desc 0010 Cholera due to vibrio cholerae A000 Cholera due to Vibrio cholerae 01, biovar cholerae 0011 Cholera due to vibrio cholerae el tor A001 Cholera due to Vibrio cholerae 01, biovar eltor 0019 Cholera, unspecified A009 Cholera, unspecified 0021 Paratyphoid fever A A011 Paratyphoid fever A 0022 Paratyphoid fever B A012 Paratyphoid fever B 0023 Paratyphoid fever C A013 Paratyphoid fever C 0029 Paratyphoid fever, unspecified A014 Paratyphoid fever, unspecified 0030 Salmonella gastroenteritis A020 Salmonella enteritis 0031 Salmonella septicemia A021 Salmonella sepsis 00320 Localized salmonella infection, unspecified A0220 Localized salmonella infection, unspecified 00321 Salmonella meningitis A0221 Salmonella meningitis 00322 Salmonella pneumonia A0222 Salmonella pneumonia 00323 Salmonella arthritis A0223 Salmonella arthritis 00324 Salmonella osteomyelitis A0224 Salmonella osteomyelitis 0038 Other specified salmonella infections A028 Other specified salmonella infections 0039 Salmonella infection, unspecified A029 Salmonella infection, unspecified 0040 Shigella dysenteriae A030 Shigellosis due to Shigella dysenteriae 0041 Shigella flexneri A031 Shigellosis due to Shigella flexneri 0042 Shigella boydii A032 Shigellosis due to Shigella boydii 0043 Shigella sonnei A033 Shigellosis due to Shigella sonnei 0048 Other specified shigella infections A038 Other shigellosis 0049 Shigellosis, unspecified A039 Shigellosis, unspecified 0050 Staphylococcal food poisoning A050 Foodborne staphylococcal -
Lesson 20. Mycobacterium
Mycobacterium MODULE Microbiology 20 MYCOBACTERIUM Notes 20.1 INTRODUCTION Mycobacterium are slender rods that sometimes show branching filamentous forms resembling fungal mycelium. In liquid cultures they form a mould-like pellicle. Hence the name ‘mycobacteria’, meaning fungus like bacteria. They do not stain readily, but once stained, resist decolourisation with dilute mineral acids. Hence they are called ‘Acid fast bacilli’. They are aerobic, nonmotile, noncapsulated and nonsporing. OBJECTIVES After reading this lesson, you will be able to: z describe the morphology of Mycobacterium tuberculosis & M. leprae z describe the characteristics of Mycobacterium tuberculosis & M. leprae z explain about pathogenesis of Mycobacterium tuberculosis & M. leprae z explain the laboratory diagnosis Mycobacterium tuberculosis & M. leprae The first member of this genus to be identified was Lepra bacillus discovered by Hansen. Koch (1882) isolated the mammalian tubercle bacillus and proved its causative role in tuberculosis. In humans tuberculosis is caused by mycobacterium tuberculosis and also by bovine type called Mycobacterium bovis. The second human pathogenic mycobacterium is the lepra bacillus causing Leprosy. The third group of mycobacterium is a mixed group from varied sources like birds, cold-blooded and warm blooded animals, from skin ulcers, soil, water and other environmental sources. They are called as atypical mycobacteria. They are opportunistic pathogens and can cause many types of diseases. MICROBIOLOGY 203 MODULE Mycobacterium Microbiology 20.2 MYCOBACTERIUM TUBERCULOSIS Morphology M tuberculosis is a straight or slightly curved rod, about 3 X 0.3 µm in size, occurring singly, in pairs or as small clumps. M bovis is usually straighter, shorter and stouter. Tubercle bacilli have been described as Gram positive, even though after Notes staining with basic dyes they resist decolourisation by alcohol even without the effect of iodine. -

BQI Icare HIV/AIDS
RESOURCE AND PATIENT MANAGEMENT SYSTEM iCare Population Management GUI (BQI) HIV/AIDS Management User Manual Version 2.6 July 2017 Office of Information Technology (OIT) Division of Information Technology iCare Population Management GUI (BQI) Version 2.6 Table of Contents 1.0 Introduction ......................................................................................................... 1 1.1 Key Functional Features .......................................................................... 1 1.2 Sensitive Patient Data ............................................................................. 2 2.0 Patient Management ........................................................................................... 3 2.1 Data Specifically Related to HIV/AIDS ..................................................... 3 2.2 Search for and View a Patient Record ..................................................... 6 2.2.1 Using a Panel ........................................................................................ 6 2.2.2 Using Quick Search ............................................................................... 7 2.3 Displaying Care Management as Default Tab ......................................... 8 2.4 Add/Edit Care Management Data ............................................................ 8 2.4.1 Entering Data on the General Area ....................................................... 9 2.4.2 Entering Data on the Partner Notification Area .................................... 11 2.4.3 Entering Data on the Antiretroviral