Scotland) Act 2000
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Glasgow City Community Health Partnership Service Directory 2014 Content Page
Glasgow City Community Health Partnership Service Directory 2014 Content Page About the CHP 1 Glasgow City CHP Headquarters 2 North East Sector 3 North West Sector 4 South Sector 5 Adult Protection 6 Child Protection 6 Emergency and Out-of-Hours care 6 Addictions 7 - 9 Asylum Seekers 9 Breast Screening 9 Breastfeeding 9 Carers 10 - 12 Children and Families 13 - 14 Dental and Oral Health 15 Diabetes 16 Dietetics 17 Domestic Abuse / Violence 18 Employability 19 - 20 Equality 20 Healthy Living 21 Health Centres 22 - 23 Hospitals 24 - 25 Housing and Homelessness 26 - 27 Learning Disabilities 28 - 29 Mental Health 30 - 40 Money Advice 41 Nursing 41 Physiotherapy 42 Podiatry 42 Respiratory 42 Rehabilitation Services 43 Sexual Health 44 Rape and Sexual Assault 45 Stop Smoking 45 Transport 46 Volunteering 46 Young People 47-49 Public Partnership Forum 50 Comments and Complaints 51-21 About Glasgow City Community Health Partnership Glasgow City Community Health Partnership (GCCHP) was established in November 2010 and provides a wide range of community based health services delivered in homes, health centres, clinics and schools. These include health visiting, health improvement, district nursing, speech and language therapy, physiotherapy, podiatry, nutrition and dietetic services, mental health, addictions and learning disability services. As well as this, we host a range of specialist services including: Specialist Children’s Services, Homeless Services and The Sandyford. We are part of NHS Greater Glasgow & Clyde and provide services for 584,000 people - the entire population living within the area defined by the LocalAuthority boundary of Glasgow City Council. Within our boundary, we have: 154 GP practices 136 dental practices 186 pharmacies 85 optometry practices (opticians) The CHP has more than 3,000 staff working for it and is split into three sectors which are aligned to local social work and community planning boundaries. -

Mental Health Bed Census
Scottish Government One Day Audit of Inpatient Bed Use Definitions for Data Recording VERSION 2.4 – 10.11.14 Data Collection Documentation Document Type: Guidance Notes Collections: 1. Mental Health and Learning Disability Bed Census: One Day Audit 2. Mental Health and Learning Disability Patients: Out of Scotland and Out of NHS Placements SG deadline: 30th November 2014 Coverage: Census date: Midnight, 29th Oct 2014 Page 1 – 10 Nov 2014 Scottish Government One Day Audit of Inpatient Bed Use Definitions for Data Recording VERSION 2.4 – 10.11.14 Document Details Issue History Version Status Authors Issue Date Issued To Comments / changes 1.0 Draft Moira Connolly, NHS Boards Beth Hamilton, Claire Gordon, Ellen Lynch 1.14 Draft Beth Hamilton, Ellen Lynch, John Mitchell, Moira Connolly, Claire Gordon, 2.0 Final Beth Hamilton, 19th Sept 2014 NHS Boards, Ellen Lynch, Scottish John Mitchell, Government Moira Connolly, website Claire Gordon, 2.1 Final Ellen Lynch 9th Oct 2014 NHS Boards, Further clarification included for the following data items:: Scottish Government Patient names (applicable for both censuses) website ProcXed.Net will convert to BLOCK CAPITALS, NHS Boards do not have to do this in advance. Other diagnosis (applicable for both censuses) If free text is being used then separate each health condition with a comma. Mental Health and Learning Disability Bed Census o Data item: Mental Health/Learning Disability diagnosis on admission Can use full description option or ICD10 code only option. o Data item: Last known Mental Health/Learning Disability diagnosis Can use full description option or ICD10 code only option. -

Vacancy Bulletin
Vacancy Bulletin Friday 26th October 2012 Unless otherwise stated, all close at NOON on Friday 9th November 2012. Applications submitted after that time may not be processed. Welcome to the NHS Greater Glasgow and Clyde Vacancy Bulletin Inside you will find details of vacancies available across the Greater Glasgow and Clyde Area. To subscribe to the weekly email bulletin simply send an email to [email protected] Management, Administrative and Clerical Page 1 - 2 Allied Health Professionals Page 3 - 4 Medical, Dental and Psychology Page 5 Nursing and Midwifery Page 6 - 10 Pharmacy Page 11 Estates, Porters, Domestics and Catering Page 12 - 13 Medical Director Flyer Page 14 Programme Support Officer Flyer Page 15 - 23 Salary Banding Information Page 24 HOW TO APPLY To download a job pack and application form for any of our vacancies visit www.nhsggc.org.uk/recruitment and follow the links OR send the job ref, closing date and the email address you want the job pack emailed to: [email protected] For more information about working in NHS Greater Glasgow & Clyde visit our website www.nhsggc.org.uk For a list of all vacancies throughout NHS Scotland visit www.jobs.scot.nhs.uk Don’t know what job is right for you? Visit our Careers Website: www.infoscotland.com/nhs MANAGEMENT, ADMINISTRATION AND CLERICAL Job Ref & Job Title Grade Hours Base Type /Salary 27057G/VB Technical Specialist (Microsoft Band 6 37.5 Westward House, PA3 2HJ Infrastructure and Security) PERM Based in the Microsoft Infrastructure and Security Team, this role for a Technical Specialist represents an excellent opportunity to progress your career within Technical Services. -

Sitename Site Info.Address1 Site Info.Address2 Site Info.Town Site Postcode Division Site Info.County Tenure
SiteName Site_Info.Address1 Site_Info.Address2 Site_Info.Town Site PostCode Division Site_Info.County Tenure 2 & 4 Waterloo Close Waterloo Close Kirkintilloch G66 2HL NHS East Dunbartonshire Owned Anvil Resource Centre Salamanca Street Glasgow G31 5BA NHS Glasgow City Owned Aranthrue Centre 103 Paisley Road Renfrew PA4 8LH NHS Renfrewshire Owned Arndale Resource Centre 80-90 Kinfauns Drive Glasgow G15 7TS NHS Glasgow City Owned Arran Resource Centre 121 Orr Street Glasgow G40 2QP NHS Glasgow City Owned Auchinlea Resource Centre Auchinlea House, 11 Auchinlea Road Easterhouse Glasgow G34 9HQ NHS Glasgow City Owned Baillieston Health Centre 20 Muirside Road Baillieston Glasgow G69 7AD NHS North Lanarkshire Owned Barrhead Health & Care Centre 213 Main Street Barrhead G78 1SW NHS East Renfrewshire Owned Bishopton Health Centre Greenock Road Bishopton PA7 5AW NHS Renfrewshire Owned Blytheswood House 4 Fulbar Lane Renfrew PA4 8NT NHS Renfrewshire Owned Brand Street Resource Centre Festival Business Park 150 Brand Street Glasgow G51 1DH NHS Leased Breast Screening Services Stock Exchange Court 77 Nelson Mandela Square Glasgow G2 1QY NHS Glasgow City Leased Bridgeton Health Centre 201 Abercromby Street Glasgow G40 2DA NHS Glasgow City Owned Caledonia House 147 Fifty Pitches Road Cardonald Business Park Glasgow G51 4ED NHS Glasgow City Leased Callander Street Clinic (Woodside) 3 Callender Street Woodside Glasgow G20 7JZ NHS Glasgow City Owned Castlemilk Health Centre 71 Dougrie Drive Castlemilk Glasgow G45 9AW NHS Glasgow City Owned Cathcart Centre -
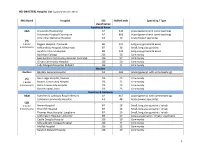
MASTER) Hospital List (Updated October 2015
HEI (MASTER) Hospital List (updated October 2015) NHS Board Hospital ISD Staffed beds Speciality / Type classification Ayrshire & Arran A&A University Hospital Ayr A2 343 Acute (general with some teaching) University Hospital Crosshouse A2 666 Acute (general with some teaching) Arran War Memorial Hospital A3 19 Acute (mixed speciality) (9) 3 acute Biggart Hospital, Prestwick B6 121 Long stay geriatric & acute 6 community Kirklandside Hospital, Kilmarnock B7 36 Small, long stay geriatric Ayrshire Central Hospital B8 142 Long stay geriatric & acute Davidson Cottage J26 26 Community East Ayrshire Community Hospital, Cumnock J26 57 Community Girvan Community Hospital J26 20 Community Lady Margaret Hospital, Millport J26 9 Community Borders Borders Borders General Hospital A2 265 Acute (general, with some teaching) (5) Hay Lodge Hospital, Peebles J26 23 Community 1 acute Hawick Community Hospital J26 22 Community 4 community Kelso Community Hospital J26 23 Community Knoll Hospital, Duns J26 23 Community Dumfries & Galloway D&G Dumfries & Galloway Royal Infirmary A2 367 Acute (general, with some teaching) Galloway Community Hospital A3 48 Acute (mixed speciality) (10) 2 acute Annan Hospital B7 18 Small, long stay geriatric / rehab 8 community Thornhill Hospital B7 13 Small, long stay geriatric / rehab Thomas Hope Hospital, Langholm B7 10 Small, long stay geriatric / rehab Lochmaben Hospital, Lockerbie B9 17 Long stay geriatric / rehab / psychiatry Castle Douglas Hospital J26 19 Community Kirkcudbright Cottage Hospital J26 9 Community Moffat Hospital J26 12 Community Newton Stewart Hospital J26 19 Community 1 HEI (MASTER) Hospital List (updated October 2015) Fife Fife Victoria Hospital, Kirkcaldy A2 621 Acute (general with some teaching) (7) Queen Margaret Hospital, Dunfermline A3 196 Acute (mixed speciality) 2 acute 5 community Cameron Hospital, Leven B7 95 Small, long stay geriatric Adamson Hospital, Cupar J26 19 Community Glenrothes Hospital J26 74 Community Randolph Wemyss Memorial Hospital J26 16 Community St. -

Scotland) 15 June 2021
Version 1.6 (Scotland) 15 June 2021 ISARIC/WHO Clinical Characterisation Protocol UK (Scotland) Recruitment Procedures for FRONTLINE CLINICAL RESEARCH STAFF The most up to date versions of the protocol and case report form are available at isaric4c.net/protocols/ A virtual site visit is available at isaric4c.net/virtual_site_visit/ AIM: Please recruit the following patients only: • Vaccine failure (positive COVID test - rather than displaying symptoms – >28d after having received a vaccine) • Reinfection (proven after proven) • Co-infection (flu/RSV) • COVID associated hyper inflammation (MIS-A/MIS-C/PINS-TS) at any age • Samples from patients with pathogens of public health interest including people identified as infected with SARS-CoV “variants of concern” • All children CONSENT: once the form is signed by a participant it is hazardous. To record consent, we suggest an independent witness observes the completed form then signs a fresh copy outside of the isolation area. Consent can also be obtained by telephone from participants or from relatives for proxy consent. RECRUITMENT PACKS: Sample collection kits will be supplied to sites. Sample collections kits can be requested from: [email protected] Each kit will have a specific kit ID number, with each component within showing this kit ID and its own respective component ID for audit purposes. Pods and bio-bags for shipping will also be supplied to sites. These can be requested from [email protected] OBTAIN SAMPLES according to the schedule. You can find out which tier you are operating at in the front page of the site file. If you have capacity to recruit at TIER 2: Day 1 2 3 4 5 6 7 8 9 28 days after discharge Samples R S S C Sample priority 1 2 3 4 R: recruitment sample; S: serial sample; C: convalescent sample. -

2019/20 Festive Guide to Your Health Services
2019/20 Festive guide to your health services NHS Greater Glasgow and Clyde, getting you to the over the festive period WHEN YOU’RE ILL, KNOW WHO TO TURN TO (ALL YEAR ROUND) Let us get you to the right care, right place, right time. Self Care & NHS inform GP Mental health Dentist For a speedy recovery, self care is the Contact your GP surgery as normal For mental health problems Visit your General Dental Practicioner best option when you have a minor for any illness which requires the contact your GP who can refer for regular check ups, planned illness or injury. services of your GP Practice. If your people to Community Mental routine treatment and emergency A well stocked medicine cabinet condition really can’t wait until your Health Services in local areas. Crisis care. If you have not registered with means you’ll receive the right surgery re-opens, contact services are available for patients who a dentist, please do so as soon as treatment immediately. NHS 24 on 111. are already known to Community possible. Mental Health Services and can be Visit NHS inform for advice when NHS 24 Advice and information is available by contacted on the telephone numbers calling the Dental Advice Helpline you’re feeling unwell: on page 18 of this booklet. www.nhsinform.scot For immediate advice when your on 0141 201 4209. GP surgery or Dental Practice is The out-of-hours Community If your dental condition cannot wait Pharmacist closed and you’re too ill to wait until Psychiatric Nurse service can be until your Dental Practice re-opens, it re-opens call NHS 24. -

Modernising and Improving Mental Health Services in Clyde
EMBARGOED UNTIL MEETING NHS Greater Glasgow and Clyde NHS Board Meeting th Tuesday, 19 August, 2008 Board Paper No Director of Mental Health Partnership 08/36 Modernising and Improving Mental Health Services across Clyde Outcome of Public Consultation 1. RECOMMENDATIONS 1.1 It is recommended that the Health Board endorse the following public consultation ‘significant service change’ proposals for submission to the Cabinet Secretary for Health & Well Being’s approval:- • Replacing a significant number of adult mental health continuing care beds at Dykebar Hospital with alternative forms of care accommodation and supports in the community. • Transferring adult acute mental health admission beds from the Royal Alexandra Hospital to more modern, purpose built, single room accommodation at Dykebar Hospital. • Re-providing older people’s mental health continuing care beds from Dykebar Hospital to higher quality accommodation within an NHS Partnership bed model with the independent sector. • Transferring low secure learning disability forensic services from Dykebar Hospital to Leverndale Hospital. 1.2 In light of responses and feedback from the consultation, it is recommended that the Health Board: • endorses the proposed commitment to consult on the Health Board’s vision for the future of the Vale of Leven site and that consultation on the various elements, including mental health, should be integrated within that process • notes the further work being undertaken to explore the mental health proposals in the light of the issues raised through -

*** JAN 07 LAYOUT.Indd
HEALTH NEWS DELIVERING BETTER HEALTH IN GREATER GLASGOW AND CLYDE FEBRUARY/MARCH 2007 Wash away Check out Hundreds of NHS jobs Taking services those germs NHS listings on our new website to the people PAGE 4 PAGE 9 PAGE 11 PAGE 12 New Beatson Cancer 2006 - a year Centre set to open of major THE new world-class West of Scotland Cancer Centre in progress Glasgow is set to launch a new era LAST year saw major in cancer care for thousands of progress in the patients. development of health services with the HAVE A LOOK INSIDE landmark start to works THE NEW BEATSON on two new long awaited hospital developments SEE PAGES 5,6,7 AND 8. at the Victoria and Stobhill. Bringing Clyde services into Greater Glasgow brought new security to key services at Inverclyde Royal Hospital. Two major mental health developments took major strides forward - The Rowanbank secure care centre started to take shape at Stobhill and plans were approved for Skye House which boats purpose built facilities for young people. We also saw the delivery of inpatient and day case waiting time targets a full year early. LOOK BACK AT A YEAR OF CHALLENGE AND SUCCESS PAGES 2 AND 3 Fast forward with pride ALL SYSTEMS GO FOR BETTER HEALTH IN 2007 HIS year will see child health and protection modernisation of NHS services through Health News, our newly further major ● The unveiling of plans for a both in acute hospitals and re-designed public focussed developments in new South Glasgow Hospital locally with powerful new local website, Our Health events and T and Children’s Hospital in Govan organisations. -

Adults with Incapacity(Scotland) Act 2000 Management of Residents Funds Register of Authorised Establishments 1
ADULTS WITH INCAPACITY(SCOTLAND) ACT 2000 MANAGEMENT OF RESIDENTS FUNDS REGISTER OF AUTHORISED ESTABLISHMENTS 1 Adult Mental Health, Learning Disability, Senior Officer Dr Michael Smith Forensic, Addictions and Adolescent Deputising Officer Anne Hawkins Mari Brannigan In-Patient Area Authorised Responsible for Authorised Establishment Manager/Deputy North West Glasgow AMH Colin McCormack Gartnavel Royal Hospital All Adult MH in- Colin McCormack Head of Mental Health 1055 Great Western Rd patient services GRH Tom McKay Glasgow G12 0XH site North East Glasgow AMH David McCrae Stobhill Hospital, a) Adult Wards - David McCrae Head of Mental Health Mackinnon House MacKinnon House, a) & b) Mary 133 Balornock Road Stobhill O’Donnell Glasgow G21 3UZ The Orchards (formerly b) Adult Wards – Ruchhill Hospital) Orchards (formally 153, Panmuir Street, Ruchill Hospital) Glasgow Parkhead Hospital c) Adult Wards - c) Bob Gillies 81 Salamanca Street Parkhead Hospital Glasgow G31 5ES South Glasgow AMH Calum MacLeod Leverndale Hospital All adult admission Calum MacLeod Head of Mental Health 510 Crookston Road long stay & rehab. June MacLeod Glasgow G53 7TU Wards, Leverndale, (to 30th April 2013) Southern Gen. Hospital Ward 32.& 1345 Govan Road Mother & Baby Glasgow G42 9TY Unit Renfrew AMH Fiona McNeill Dykebar Hospital, a) all adult Katrina Phillips General Manager – Clyde MH Grahamston Road, admissions Alexander Buchanan Paisley, continuing care & Caroline Burling Renfrewshire Rehabilitation wards- PA2 7DE Dykebar Royal Alexandra Hospital, b) all adult -

Partnership Improvement and Outcomes Division.Dot
Balance of Care / Continuing Care Census Definitions and data recording manual Revised September 2009 CONTENTS 1 Introduction 1.1 Purpose of this Paper 3 1.2 Background 3 1.3 Coverage and context of census 3 2 Data Requirements 2.1 Census Data 4 2.2 Census Date 4 2.3 Data Quality 4 2.4 Guidance for Data Input 4 2.4.1 Example of Excel Spreadsheet 4 3 NHS Continuing Care Census Data Items 3.1 Location Code 5 3.2 Location Name 5 3.3 CHI (Community Health Index) 6 3.4 Patient Identifier 6 3.5 Patient Name 7 3.6 Gender 7 3.7 Date of Birth 7 3.8 Date of Admission 8 3.9 Ethnicity 9 3.10 Speciality 10 3.11 Patient’s Postcode of Home address 12 3.12 Patient’s town/city of residence (if postcode unavailable) 12 3.13 Patient’s area of town/city (only required for larger cities, only required if postcode unavailable) 13 3.14 Delayed Discharge check (Y/N) 13 4 Submissions of Data 4.1 Census Data Collection 14 4.2 Date of Submission 14 4.3 Method of Submission 14 5 Contacts 5.1 NHS National Services Scotland 15 6 Appendix 1 What is NHS Continuing Health care Appendix 2 Location codes reported at previous census Version 3.3, September 2009 2 1 Introduction 1.1 Purpose of this Paper This paper provides guidance to NHS Boards on definitions, procedures and information concerning the Balance of Care / Continuing Care Census. 1.2 Background There is no method for identifying all patients who are receiving NHS care that is on-going non-acute care, delivered as an inpatient, and often over an extended period, in whatever setting (including hospice or care home). -
Vision for the Vale of Leven Hospital
Vision for the Vale of Leven Hospital Consultation Document October 2008 – January 2009 1 Foreword The Vale of Leven Hospital plays an important role in the provision of health services to the West Dunbartonshire, Helensburgh and the Lochside communities. For the past 10 years the future of the hospital has been subject to much debate and considerable concern as services have had to change for a number of reasons. We are now able to describe a Vision for the Vale of Leven which we hope will end the uncertainty faced by our patients, by our staff and by the wider community. Our Vision for the future of the Vale of Leven Hospital is that it will continue to be a vibrant and busy NHS site and that it will continue to play the central role in the provision of NHS care to the local communities. One of our key principles in developing the Vision for the Vale has been to aim to provide high quality and safe services as locally as possible. This is the challenge that has been presented to us by the groups of independent experts that have considered the services offered at the Vale, by community groups in frequent discussions during the past two years, and by our staff who will strive to ensure that anything we do is safe and provides excellent care. We firmly believe that the Vision we describe in this document represents the best possible balance between providing local access to high quality services and a requirement to travel for more specialist or intensive care on the occasions when it is required.