UK Vaccination Policy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Meningitis: Immunizations on Pennsylvania College
JOINT STATE GOVERNMENT COMMISSION General Assembly of the Commonwealth of Pennsylvania MENINGITIS: IMMUNIZATIONS ON PENNSYLVANIA COLLEGE AND UNIVERSITY CAMPUSES APRIL 2020 Serving the General Assembly of the Commonwealth of Pennsylvania Since 1937 - 1 - REPORT Meningitis: Immunizations on Pennsylvania College and University Campuses Project Manager: Susan Elder, Fiscal Analyst Allison Kobzowicz, Public Policy Analyst Stephen Kramer, Staff Attorney Project Staff: Wendy Baker, Executive Assistant Kahla Lukens, Administrative Assistant (Dec. 2019) Maureen Hartwell, Public Policy Analyst Intern (Aug. 2019) The report is also available at http://jsg.legis.state.pa.us - 0 - JOINT STATE GOVERNMENT COMMISSION Telephone: 717-787-4397 Room 108 Finance Building Fax: 717-783-9380 613 North Street E-mail: [email protected] Harrisburg, PA 17120-0108 Website: http://jsg.legis.state.pa.us The Joint State Government Commission was created in 1937 as the primary and central non- partisan, bicameral research and policy development agency for the General Assembly of Pennsylvania.1 A fourteen-member Executive Committee comprised of the leadership of both the House of Representatives and the Senate oversees the Commission. The seven Executive Committee members from the House of Representatives are the Speaker, the Majority and Minority Leaders, the Majority and Minority Whips, and the Majority and Minority Caucus Chairs. The seven Executive Committee members from the Senate are the President Pro Tempore, the Majority and Minority Leaders, the Majority and Minority Whips, and the Majority and Minority Caucus Chairs. By statute, the Executive Committee selects a chairman of the Commission from among the members of the General Assembly. Historically, the Executive Committee has also selected a Vice-Chair or Treasurer, or both, for the Commission. -

A Brief History of Vaccines & Vaccination in India
[Downloaded free from http://www.ijmr.org.in on Wednesday, August 26, 2020, IP: 14.139.60.52] Review Article Indian J Med Res 139, April 2014, pp 491-511 A brief history of vaccines & vaccination in India Chandrakant Lahariya Formerly Department of Community Medicine, G.R. Medical College, Gwalior, India Received December 31, 2012 The challenges faced in delivering lifesaving vaccines to the targeted beneficiaries need to be addressed from the existing knowledge and learning from the past. This review documents the history of vaccines and vaccination in India with an objective to derive lessons for policy direction to expand the benefits of vaccination in the country. A brief historical perspective on smallpox disease and preventive efforts since antiquity is followed by an overview of 19th century efforts to replace variolation by vaccination, setting up of a few vaccine institutes, cholera vaccine trial and the discovery of plague vaccine. The early twentieth century witnessed the challenges in expansion of smallpox vaccination, typhoid vaccine trial in Indian army personnel, and setting up of vaccine institutes in almost each of the then Indian States. In the post-independence period, the BCG vaccine laboratory and other national institutes were established; a number of private vaccine manufacturers came up, besides the continuation of smallpox eradication effort till the country became smallpox free in 1977. The Expanded Programme of Immunization (EPI) (1978) and then Universal Immunization Programme (UIP) (1985) were launched in India. The intervening events since UIP till India being declared non-endemic for poliomyelitis in 2012 have been described. Though the preventive efforts from diseases were practiced in India, the reluctance, opposition and a slow acceptance of vaccination have been the characteristic of vaccination history in the country. -

Introduction
CHAPTER ONE: Introduction 1.1: General introduction Your Committee having carefully considered the Message of His Excellency the Lieutenant-Governor, and having also communicated with the principal Medical Practitioners in Hobart Town, Launceston, and other parts of the country, and ascertained their opinions as to the best mode of promoting vaccination, (which is admitted by all competent authorities to be extremely desirable, as affording the best protection against the ravages of that dreadful disease the Small-pox), have arrived at the unanimous conclusion that the most, if not the only effectual means of rendering vaccination general throughout the Island, will be by passing an Act of the Legislature imposing a pecuniary penalty on the parent or guardian of any child, above the age of six months and under that of fourteen years, who shall, without reasonable cause or excuse, be found after the 1st day of April next not to have been vaccinated.1 With this seemingly uncontroversial recommendation in September 1853, the chairman of the Tasmanian Select Committee on Smallpox and Colonial Secretary, William Champ, set into motion the first Compulsory Vaccination Act in the Australian colonies. Carefully considered in light of expert opinion and local conditions, it also represents an early instance of the extension of state authority into the private lives of citizens and an integral component of the development of public health in the colonies. The presence of smallpox in Sydney caused this exotic and terrible disease to appear immediately threatening, making the widespread implementation of preventive measures reasonable. When Champ was writing the above statement, vaccination was not a new technology. -
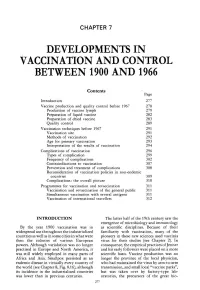
Chapter 7. Developments in Vaccination and Control Between
CHAPTER 7 DEVELOPMENTS IN VACCINATION AND CONTROL BETWEEN 1900 AND 1966 Contents Page Introduction 277 Vaccine production and quality control before 1967 278 Production of vaccine lymph 279 Preparation of liquid vaccine 282 Preparation of dried vaccine 283 Quality control 289 Vaccination techniques before 1967 291 Vaccination site 291 Methods of vaccination 292 Age for primary vaccination 293 Interpretation of the results of vaccination 294 Complications of vaccination 296 Types of complication 299 Frequency of complications 302 Contraindications to vaccination 307 Prevention and treatment of complications 308 Reconsideration of vaccination policies in non-endemic countries 309 Complications : the overall picture 310 Programmes for vaccination and revaccination 311 Vaccination and revaccination of the general public 311 Simultaneous vaccination with several antigens 311 Vaccination of international travellers 312 INTRODUCTION The latter half of the 19th century saw the emergence of microbiology and immunology By the year 1900 vaccination was in as scientific disciplines . Because of their widespread use throughout the industrialized familiarity with vaccination, many of the countries as well as in some cities in what were pioneers in these new sciences used vaccinia then the colonies of various European virus for their studies (see Chapter 2) . In powers . Although variolation was no longer consequence, the empirical practices of Jenner practised in Europe and North America, it and his early followers were placed on a more was still widely employed in many parts of scientific basis . Vaccine production was no Africa and Asia . Smallpox persisted as an longer the province of the local physician, endemic disease in virtually every country of who had maintained the virus by arm-to-arm the world (see Chapter 8, Fig. -

Reassessing Vaccination in England, 1796-1853
International Social Science Review Volume 95 Issue 3 Article 2 “A Splendid Delusion:” Reassessing Vaccination in England, 1796-1853 Kaitlyn Akel Follow this and additional works at: https://digitalcommons.northgeorgia.edu/issr Part of the Anthropology Commons, Communication Commons, Economics Commons, Geography Commons, International and Area Studies Commons, Political Science Commons, and the Public Affairs, Public Policy and Public Administration Commons Recommended Citation Akel, Kaitlyn () "“A Splendid Delusion:” Reassessing Vaccination in England, 1796-1853," International Social Science Review: Vol. 95 : Iss. 3 , Article 2. Available at: https://digitalcommons.northgeorgia.edu/issr/vol95/iss3/2 This Article is brought to you for free and open access by Nighthawks Open Institutional Repository. It has been accepted for inclusion in International Social Science Review by an authorized editor of Nighthawks Open Institutional Repository. “A Splendid Delusion:” Reassessing Vaccination in England, 1796-1853 Cover Page Footnote Kaitlyn Akel holds a B.A. in History and a B.S. in Biology from the University of Arkansas, and is currently a MPH candidate at the University of Michigan School of Public Health. This article is available in International Social Science Review: https://digitalcommons.northgeorgia.edu/issr/vol95/ iss3/2 Akel: “A Splendid Delusion:” Reassessing Vaccination in England, 1796-1853 “A Splendid Delusion:” Reassessing Vaccination in England, 1796-1853 Public health interventions integrate into our present-day habits to the point of imperceptibility. Policies revolve around our speed limits, employee sanitation standards, food preparation policies, immunization mandates: all with the encompassing intent to increase our fitness in society. This was not the case in nineteenth century England. -

Volume 1: Issue 2
VOLUME 1: ISSUE 2 || APRIL 2019 || Email: [email protected] Website:www.whiteblacklegal.co.in Page | 1 DISCLAIMER No part of this publication may be reproduced or copied in any form by any means without prior written permission of Editor-in-chief of WhiteBlackLegal – The Law Journal. The Editorial Team of WhiteBlackLegal holds the copyright to all articles contributed to this publication. The views expressed in this publication are purely personal opinions of the authors and do not reflect the views of the Editorial Team of WhiteBlackLegal or Legal Education Awareness Foundation. Though all efforts are made to ensure the accuracy and correctness of the information published, Jurisperitus shall not be responsible for any errors caused due to oversight or otherwise. Page | 2 EDITORIAL TEAM EDITOR IN CHIEF Name - Mr. Varun Agrawal Consultant || SUMEG FINANCIAL SERVICES PVT.LTD. Phone - +91-9990670288 Email - [email protected] EDITOR Name - Mr. Anand Agrawal Consultant|| SUMEG FINANCIAL SERVICES PVT.LTD. Phone - +91-9810767455 Email - [email protected] EDITOR (HONORARY) Name - Smt Surbhi Mittal Manager || PSU Phone - +91-9891639509 Email - [email protected] EDITOR(HONORARY) Name - Mr Praveen Mittal Consultant || United Health Group MNC Phone - +91-9891639509 Email - [email protected] EDITOR Name - Smt Sweety Jain Consultant||SUMEG FINANCIAL SERVICES PVT.LTD. Phone - +91-9990867660 Email - [email protected] EDITOR Name - Mr. Siddharth Dhawan Core Team Member || Legal Education Awareness Foundation Phone - +91 -9013078358 Page | 3 ABOUT US WHITEBLACKLEGAL is an open access, peer-reviewed and refereed journal provide dedicated to express views on topical legal issues, thereby generating a cross current of ideas on emerging matters. -

Queen's Women: the Contagious Diseases Acts of 1866 and 1869 By
Queen’s Women: The Contagious Diseases Acts of 1866 and 1869 By Melissa N. Bettes A Thesis Submitted to the Graduate Faculty in partial fulfillment of the requirements for the degree of MASTERS OF ARTS IN HISTORY University of Central Oklahoma Spring 2017 TABLE OF CONTENTS Acknowledgements i Abstract ii Introduction: An Introduction to the Crusade to Repeal the 1 Contagious Diseases Acts of 1866 and 1869 Chapter 1: Crusade to Control Women: 28 Contagious Diseases Acts of 1866 to 1869 Chapter 2: Crusade to Control 48 "Queen's Women" in the Age of Victoria Chapter 3: Crusade to Control Social Purity 75 Led by Josephine Butler Chapter 4: Stansfeld's "Hysterical Crusade" 94 to Abolish Gendered Legislation Conclusion 132 Bibliography 136 Appendix 1: Contagious Diseases Acts Submission Forms 148 Appendix 2: Table I. Showing the Admissions into Hospital for 152 Primary Venereal Sores and Gonorrhea, at Twenty-Eight Stations Of Troops in the United Kingdom in each Year Appendix 3: Table I. England and Whales. Number of Houses of 153 Known Bad Character as Returned by the Police in each of the undermentioned Years. Appendix 4: London Rescue Society’s Returns Regarding 154 Clandestine Prostitution i ACKNOWLEDGEMENTS First, I would like to thank my advisors for their unflagging support and assistance from the development to the completion of this Master’s thesis. Dr. Jessica A. Sheetz-Nguyen, my committee chair and mentor, provided a continual source of information and guidance. I am extremely grateful for her years of support during the research and developing of this project. Dr. Michael S. -

ACCESS DENIED the CASE AGAINST a TWO-TIER BRITAIN UNDER COVID CERTIFICATION About
ACCESS DENIED THE CASE AGAINST A TWO-TIER BRITAIN UNDER COVID CERTIFICATION About Big Brother Watch is a civil liberties and privacy campaigning organisation, fighting for a free future. We’re determined to reclaim our privacy and defend freedoms at this time of enormous technological change. We’re a fiercely independent, non-partisan and non-profit group who work to roll back the surveillance state and protect rights in parliament, the media or the courts if we have to. We publish unique investigations and pursue powerful public campaigns. We work relentlessly to inform, amplify and empower the public voice so we can collectively reclaim our privacy, defend our civil liberties and protect freedoms for the future. Contact Silkie Carlo Director Email: [email protected] Jake Hurfurt Head of Research and Investigations Email: [email protected] BigBrotherWatch.org.uk StopVaccinePassports.co.uk @BigBrotherWatch Acknowledgments We would like to thank our supporters who made this thorough and rapid review possible. With thanks to our volunteer researcher Esme Harrington for contributing excellent evidence to this report. ACCESS DENIED: THE CASE AGAINST A TWO-TIER BRITAIN UNDER COVID CERTIFICATION Publication date: 2nd April 2021 1 CONTENTS Introduction………………………………………………………………................………………….4 Recommendations……………………………............……………………………………………...5 Report Summary……………………………...............……………………………………………...6 The COVID-status certificate review…………………........…………………………………….7 Definition of COVID-status -

COVID-19 Vaccine Deployment: Behaviour, Ethics, Misinformation
21 OCTOBER 2020 COVID-19 vaccine deployment: Behaviour, ethics, misinformation and policy strategies This rapid review of science of the behavioural aspects of vaccine uptake and misinformation is from the Royal Society and the British Academy to assist in the understanding of COVID-19. This paper is a pre-print and has been subject to formal peer-review. SUMMARY KEY POINTS • A community-level vaccine coverage of 80+% will be required to protect the community from infection, dependent on the vaccine efficacy and duration of protection. • Public expectations urgently need to be managed to prepare for a longer-term transition where non-pharmaceutical interventions remain in place. • Behavioural factors underpinning vaccine uptake are: (1) complacency, (2) trust and confidence in efficacy and safety, (3) convenience, (4) sources of information; and, (5) socio-demographic variation. • COVID-19 vaccine deployment faces an unprecedented degree of uncertainty and complexity, which is difficult to communicate, such as immune response, duration of immunity, repeated vaccination, transmission dynamics, microbiological and clinical characteristics and multiple vaccines. • Priority groups for vaccine deployment need transparent public debate to build support for ethical principles. • Current seasonal flu uptake is low in certain groups, suggesting vaccination challenges, which include: high risk groups under the age of 65 (40 - 50%), support staff in health care organisations (as low as 37%) and London and even variation amongst key workers such as Doctors (40 - 100%). • Deployment and tracking should build on existing immunisation programmes such as primary care by GPs to identify comorbidities, track vaccinations and reminders for additional boosters. • COVID-19 vaccine deployment faces an infodemic with misinformation often filling the knowledge void, characterised by: (1) distrust of science and selective use of expert authority, (2) distrust in pharmaceutical companies and government, (3) straightforward explanations, (4) use of emotion; and, (5) echo chambers. -

Laws of Foreign Countries
CATALOGUE LAWS OF FOREIGN COUNTRIES STATE LIBRAEY OF MASSACHUSETTS 1911. PREPARED BY ELLEN M. SAWYEE, Principal Assistant. BOSTON: WEIGHT & POTTER PRINTING CO., STATE PRINTERS, 18 Post Office Squabe. 1911. S^^ <f 8S Approved bt The State Boaed of Publication. LAWS OF FOREIGN COUNTRIES. CODES AND COLLECTIONS. American Bar Association. Comparative Laiv Bureau. Annual bulletin, July 1, 1908-10. No. 1-3. Phila- delphia, 1908-10. 8°. Annuaire de Legislation fitrangere, publie par la So- ciete de Legislation Comparee, contenant la traduc- tion des principales lois votees dans les pays etran- gers, [1870J-1908. le-38e annee. Paris, Cotillon, 1872-1909. 38 v. 8°. The title, from 1882, reads " contenant le texte des principales lois," etc. A new series begins with v. 31 which is numbered " 2e serie, le annee." Belgium. Bureau de Legislation. Bibliotheque. Cata- logue, ler Jan. 1902. Bruselles, Hayez, imprimeur des academies royales de Belgiques, 1902. 1. 8°. x, 302 p. Ministere de I'Industrie et du Travail. Office du Travail. Annuaire de la legislation du travail. le-9e annee. 1897-1905. Bruxelles, 1898-1906. 9 V. 8°. Coleccion de codigos civiles americanos y europeos. Tomo 1-3. Madrid, F. Gongora y Compania, 1879- 80. 3 V. 8°. Contents. Vol. 1. Mejioo. 2. La republica oriental del Uruguay. 3. La republica de Guatemala, 1877. Vol. 1 has the title " Biblioteea de la Eeviata de los Tribunales. Legislacion extranjera; coleccion de c6digos civiles," etc. Collection de codes etrangers. 1-23. Paris, A. Durand et Pedone-Lauriel, 1890-1906. 23 v. 8°. Contents. Vol. 1. Spain. Code civil espagnol, promulgue le 24 juillet 1889; tr. -

Big Brother Watch Briefing on the Health and Social Care Act 2008 (Regulated Activities) (Amendment) (Coronavirus) Regulations 2021 – House of Lords
Big Brother Watch Briefing on the Health and Social Care Act 2008 (Regulated Activities) (Amendment) (Coronavirus) Regulations 2021 – House of Lords July 2021 1 About Big Brother Watch Big Brother Watch is a civil liberties and privacy campaigning organisation, fighting for a free future. We’re determined to reclaim our privacy and defend freedoms at this time of enormous technological change. We’re a fiercely independent, non-partisan and non-profit group who work to roll back the surveillance state and protect rights in parliament, the media or the courts if we have to. We publish unique investigations and pursue powerful public campaigns. We work relentlessly to inform, amplify and empower the public voice so we can collectively reclaim our privacy, defend our civil liberties and protect freedoms for the future. Contact Silkie Carlo Director Direct line: 020 8075 8478 Email: [email protected] Madeleine Stone Legal & Policy Officer Direct line: 020 8075 8479 Email: madeleine.stone @bigbrotherwatch.org.uk 19th July 2021 2 CONTENTS INTRODUCTION………..…………………………………….……………………………………………………….4 RECOMMENDATIONS……………………………………………………………………………………………….5 Effect of the Regulations……..…………………….…………………………………………………………….6 Impact assessment……...……………………… ………..……………………………………………………….7 Scrutiny “impossible”……………………………………………………………………………………..9 Workers’ rights, beyond care home premises …………….…………………………………………….11 Unnecessary…………………………………………..………………………....………………………………... 12 What coverage is needed?…………………………………………..………………………....….. 12 What coverage -

The Victorian Taxpayer and the Law: a Study in Constitutional Conflict Chantal Stebbings Frontmatter More Information
Cambridge University Press 978-0-521-89924-6 - The Victorian Taxpayer and the Law: A Study in Constitutional Conflict Chantal Stebbings Frontmatter More information THE VICTORIAN TAXPAYER AND THE LAW The central element of the taxpayer’s relationship with the law was the protection it afforded to ensure only the correct amount of tax was paid, that it was legally levied and justly administered. These legal safeguards consisted of the fundamental constitutional provision that all taxes had to be consented to in Parliament, local tax administration, and a power to appeal to specialist tribunals and the courts. The book explains how these legal safeguards were established and how they were affected by changing social, economic and political conditions. They were found to be restrictive and inadequate, and were undermined by the increasing dominance of the executive. Though they were significantly recast, they were not destroyed. They proved flexible and robust, and the challenge they faced in Victorian England revealed that the underlying, pervasive constitutional principle of consent from which they drew their legitimacy provided an enduring protection for the taxpayer. chantal stebbings is Professor of Law and Legal History at the University of Exeter and a Fellow of the Royal Historical Society. She is also a General Commissioner of Income Tax. In the past she has served as Dean of the Faculty of Law at the University of Exeter, Visiting Professor at the University of Rennes, France and a Fellow of the Institute of Taxation. © Cambridge University Press www.cambridge.org Cambridge University Press 978-0-521-89924-6 - The Victorian Taxpayer and the Law: A Study in Constitutional Conflict Chantal Stebbings Frontmatter More information cambridge tax law series Tax law is a growing area of interest, as it is included as a subdivision in many areas of study and is a key consideration in business needs through- out the world.