Methicillin Resistant Staphylococcus Epidermidis Induced Endogenous Endophthalmitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Village Statistics West Godavari District Madras Presidency
CENSUS OF 1941 VILLAGE STATISTICS WEST GODAVARI DISTRICT MADRAS PRESIDENCY lY THE SUPERI~qTENDENT lERNMENT PRESS MADRAS 1943 ' BHIMAVARAM TALUK. Population. Charge 7-Bhimavaram Town ... 21,023 Do. 8-Undi Town - 6,334 .. Do. 9-Bhimavaram Rural 175,006 NOTE.-Throughout F.P. = Floating population. Fl. = Liable to regularly recurring floods. W. GODA. 2 "x a-lu":: l..~~ ,-tI~l ..... e'I c'!:~ X~ . ..t<....,.C\I r:'I .....,""i"~ CQ C'l,""",~..... ~~ O)OO~('()~CIC ~ ~QQ~ Q ... ~a:t~... ~ '" "",... O~e10~l_.-I :C;:.o"Jrf..·~C \'.0 .,....,~O:O_.~lry_ _. ---t< Co::: l~ ~~~~~~ ~1~~iXl ~ .'"::, OCc.~~ '-tIL~ "'iI~0C;, ,-i' <:-J" "....,- "';,.... i' ,-.i·'~'" c-,f,....,- ~~~~ :~ Q "'d"C'I '1"""'1 \()~~ .... ~Q) ~OOQO¢1~. O .. t--~ll) ~ eo"" 00 :l_r.:lt:lr-4(1:l~e.o C'1r---oocOo:.~ ~ 00 ....-Ic:O::O~ If:I ..... ~rn~ \~ .,...... <::OlDOlO I"""'I~ tOOl!':> U':l ,...i' "';,... f ,.;~ ,...;...; CI';l~OO"-'4~ r-Ie<:lOlt")ooe.o 1-1.OCO~e\1Ct> 'fJ.::T.lOl~~rl r-I cQ"'l.... ~ ~OOo;-,)OOO~ ~~OC'-l eo C'I ~LCQ~ Ocr.l lCOlQ T""i" rl H- ,,,,,.j' rir-i' riM 3 ", .~r-{c:() '''00 00 .... ", e"H()OCl~t'- ~oO::IOI'X>~ ~COO-.:fll'- 000 .(jJ ·00 .(jJ '00"'" .", ·ce~r-f """"", ..... ...... .",,,,, ... .... ~"""~~lO ·,.....~COlO <ot- :~~ .... ..... .", ....a> "".... '"", .... ",ll) M ... f""I4()l"ll!f41'""4 ll) .... "'" .., .... ....... .... .... ""'" M .... .... '" .... ", <>l .... ... "" ","'''' '" '" <>i '" ... '" '" ........ .... ..... ", '<>l00 ·00 !"""It!'1tOctJ~ "'(jJ .eo", 0 ·0 .m .t- ............. '" ....", ", .", ,-hQ,.-4t-1\l:) ..., ..., .... ..... "" '" '" "" .... ... QO~,....~a> eoocC"!l~ .,-.(C'tJl'Q)t-o~ .o'lllfle>lCllc:D t>lco"""o 0"" .. ", ... '0 (00"'0 ... -

International Journal of Advanced Research and Review
IJARR, 5(10), 2020; 40-45 International Journal of Advanced Research and Review www.ijarr.in PHYSICOCHEMICAL ANALYSIS OF WATER SAMPLES IN AND ARROUND ELURU AND THEIR COMPARATIVE STUDY 1N.Madhavi, 2G.Srinivasa Rao, 3B.Anu Radha, 4K.Varalakshmi, 5V.Nagalakshmi 1,2,3,4,5Ch.S.D.St.Theresa’s College for Women(A), Eluru ABSTRACT Water is one of the most valuable of all earth-known natural resources. It is essential to all living species, most environmentally sustainable structures, human health, food production, and economic growth. Drinking water protection is critical to the health. Related pollutants impact the quality of the drinking water .These pollutants cause severe health issues. The Drinking Water quality becomes low due to these pollutants. Such low quality water also causes many diseases in humans. The purpose of this research is to provide information on the physicochemical characteristics to discuss its suitability for human consumption. To determine water quality, physicochemical aspects of the water were investigated. The water quality is determined in neighbouring villages in 11 areas of Eluru. Samples of water taken from Madhepalli, NTR Colony, Pathebadha, Ponangi, Satrampadu, Shanti nagar, Tangellamudi, Vempadu, Vanguru, Vatluru and Vasantawada. Then each water sample is under study for water samples' physico- chemical status. In physico-chemical research, different consistency parameters are calculated including pH, Basic conductivity (SP), total dissolved solids (TDS), total hardness according to WHO water quality standards; the pH of all water samples was found to be nearly neutral. All the Parameters were within the limits permitted. Stated and explained the findings. Keywords: Physico-chemical analysis, water analysis, water samples, Total hardness of water, INTRODUCTION Water is a product of universe use. -

Of the Revenue Divisional Fficer, Jangareddigudem
Collectorate Roc.No. 1791 7l2O2OlDr West Godavari Eluru., datedl7 .O7 .2O2O. PRO INGS OT THE COLLECTOR & DISTRICT MAGISTRATE' WEST GODAVARI' ELURU PRESENT: SRI MUTYALA RAJU RE\It,I'A'S.' *** ve cau onary & Sub: C VI D :19 w St Godavarl D IStric L Pre enti Pre ti 1 7 for paredneSS measure S under Epidemlc DiSC ase S Act 89 1 Spread n of co tainme nt ntro 1 & prevention c) f CoVI D 9 Fast o C VI D pOSItive case S n ULB S illage S Imp1e mentation f re trictionS w.e.f. 2 5-07 co20 to J 1 07 2020 orderS I SSued Read: I G. O.R.T.No. 280, dated: 3 1. 05.2O2O of Government of AP' . COVID Instant Order No.2O, 43 & 50, dated:O9'04'2020, 3.O5.2O2O & 18.05.2020 of Special Chief Secretary to overnment, HM & FW DePt. J G.O.R.T.No.288, Dated: 05.06'2O2O of Government of AP' 4 Proceedings in Roc.No.1791367 I 2O2O lDl, Dated: 30-06-2020 ot.o7.2020 5 Roc.No.569/2O2OlD, dated: 23.07.2O2O of the Sub Collector aSApuram ) 6 Roc.no. 179186L l2O2O D dated 2 J 07 20 0 of th Rev nue ivisional Office, Kowur. 7 Roc.No. l2O2O, dated: .O7.2O2O of the Revenue Divisional fficer, Jangareddigudem. 8 Roc.No.682l2O2Ol A, dated: 23.O7.2O2O of the Revenue ivisional Oflicer, Eluru. 7 Record Received from Revenue Divisional Office, Kukunoor' ORDER: In view of the fast spreading of the CORONA virus in certain places in West Godav District and to control the spreading of the positive cases and to reduce death cases, it has been decided to implement the instructions issued in the refere 4th read above in the following UlBs/Villages w.e.f 25.O7.2O2O to 31.O7 .2O2 Name of the Name -

District Census Handbook, West Godavari, Part X
CENSUS 1971 SERIES 1 ANDHRA PRADESH DISTRICT CENSUS HANDBOOK WEST GODAVARI PART X-A VILLAGE & TOWN DIRECTORY PAR.T X-B VILLAGE & TOWN PRIMARY CENSUS ABSTRACT T. VEDANTAM OF THI INDIAN ADMINISTRATIVE SERVIC! DIRECTOR OF CENSUS OPERATIONS ANDHRA PRADESH- PUII.ISIiIIO IT TMI ~VERNMENT Of ANOHRA PRADI!SH 1973 INTENSIVE AGRICULTURAL DEVELOPMENT PROGRAMME IN WEST GODAVARI DISTRICT West Godavari District irrigated by the waters of river Godavari is one of the [ most progressive districts for agriculture and other agro~based industries and trade. More than three fourths of the total cropped area is under assured irrigation. The cultivators in this district are by and large fertiliser minded and educated for preventing pests and disease attacks of crops both by cultural and chemical methods. The farmers in this district have long experience in improved methods of cultivation and produce sizeable marketable surplus every year. It is, for these reasons that the Intensive Agricultural Divtrict programme known as the Package Programme was started first in West Godavari District in 1960 aiming at further increasing the production offood and important commercial crops. West Godavari District ranks first among the rice growing districts in the State, both in regard to area under crop and in respect of production. The area under rice in 1970-71 in this district is 384,367 hectares constituting 70.5% of the total cropped area in the district and 10.9% of the total area under the crop in Andhra Pradesh State. The annual outturn of rice in this district is 659,078 tonnes which forms 13.8% of the total outturn in the State. -

S.No Ht No S Name Mob Number Address DISTRICT Course Name Inst Name
S.No ht_no s_name mob_number Address DISTRICT course_name inst_name Vijaya Nagesh Institute of H, No: 1-5, (po&m) Diploma in Medical Medical Sciences (Denduluru V V Gopala Krishna Denduluru, ,Dt: Lab Technician Development Society Instute) , 1 0904035-S Basava 1111111111 West Godavari.,A.P West Godavari (Two Years) Course Denduluru , West Godavari H, No: 24 C-12/30, R M S Colony,,Etigattu, 34th Division, Eluru Diploma in Medical Padinjaraveedu ( P & M),,West Lab Technician Andhra Medical College , 2 1002020 Sowmya 7396343535 Godavari Dist. West Godavari (Two Years) Course Visakhapatnam , Visakhapatnam D No 2-129, Kesavaram Vill ,Ganapavaram ( Diploma in Medical Raghava Institute of Medical M),West Godavari Lab Technician Sciences (DMLT) , Kakinada , East 3 1003101 Rayala Rajesh 9603489196 Dist., A.P West Godavari (Two Years) Course Godavari Dist, A.P. Plat No: 103, Sajapuram, ,Harichandra Diploma in Towers, Phase- Opthalmic GSL Ophthalmic Assistant Course 2,(po&m) Tuni,,Dt: Assistant (Two , Rajanagaram Mandal , East 4 917014 Gorley Madhuri 9705404402 West Godavari. West Godavari Years) Course Godavari Dist, A.P. Page 1 S.No ht_no s_name mob_number Address DISTRICT course_name inst_name D No 5-124, Brahminstreet,Ach Diploma in anta(P&M), West Perfusion Swatantra Para Medical Satishkumar Godavari - Technician (Two Institutions , Rajahmundry , East 5 1103115 Banda 9959208202 534123,A.P West Godavari Years) Course Godavari Dist, A.P. Kovvali(v),Dendulur Diploma in Medical u(m),West Lab Technician Sri Sai DMLT Institution , 6 905053 Baby Andugula -

30-03-2019 NMMS MERIT LIST.Pdf
PAGE : 1 ANDHRA PRADESH::NATIONAL MEANS-CUM-MERIT SCHOLARSHIP SCHEME EXAMINATION,NOVEMBER-2018 COMMUNITY WISE LIST OF SELECTED CANDIDATES FOR AWARD OF SCHOLARSHIPS DISTRICT :05-WEST GODAVARI CATEGORY : GENERAL -------------------------------------------------------------------------------------------------------------------------------------------- S.No Roll.No NAME OF THE CANDIDATE SEX COMM PHC DOB SAREA MED FATHER MOTHER INC MAT **** SAT **** TOT MOBILE NO. FATHER's NAME Sc_Code EDU OCP EDU OCP ---------------------------------------------------------------------------------------------------------------------------------------------- 1 340180528195 BUDIDA VARSHITHA F BC-B 4 17/11/2005 Urban 2 1 7 1 8 1 74 46 120 6281169847 ELLAPPA 28152390290 SESD MPL HS, 35TH DIV, ELURU ---------------------------------------------------------------------------------------------------------------------------------------------- 2 340180529220 KAKKALA SAI NAGA DURGA PRASAD M BC-B 4 22/10/2004 Rural 2 3 7 2 7 1 63 54 117 7337405376 KAKKALA SIVA SHANKAR 28152300404 ZPHS, SATRAMPADU ---------------------------------------------------------------------------------------------------------------------------------------------- 3 340180522200 PITHANI SAI KRISHNA M BC-B 4 09/12/2005 Rural 2 1 7 1 8 1 65 49 114 7893276971 PITHANI VENKATARATNAM 28154200908 ZPHS, JINNURU ---------------------------------------------------------------------------------------------------------------------------------------------- 4 340180529129 GOLLA DHANA SWAROOP M BC-C 4 11/09/2005 -
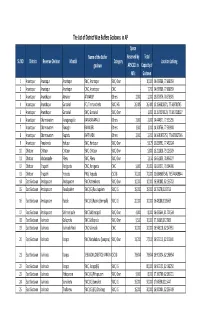
The List of District Wise Buffers Godowns in AP
The List of District Wise Buffers Godowns in AP Space Name of the Buffer Reserved by Total SL.NO District Revenue Division Mandal Category Location Latlong godown APSCSCL in Capacity of MTs Godown 1 Anantapur Anantapur Anantapur SWC, Anantapur SWC, Own ‐ 10,000 14.695586, 77.608059 2 Anantapur Anantapur Anantapur CWC, Anantapur CWC ‐ 7,700 14.695586, 77.608059 3 Anantapur Ananthapur Atmakur ATMAKUR Others 2,000 2,000 15.873576, 78.578505 4 Anantapur Ananthapur Guntakal FCI, Timmancherla SWC, HG 26,485 26,480 15.1593818971, 77.389781745 5 Anantapur Ananthapur Guntakal SWC, Guntakal SWC, Own ‐ 1,000 15.1575278129, 77.3857258627 6 Anantapur Dharmavaram Kanaganapalle KANAGANAPALLI Others 2,000 2,000 14.444371, 77.525255 7 Anantapur Dharmavaram Ramagiri RAMAGIRI Others 1,000 1,000 14.308766, 77.500908 8 Anantapur Dharmavaram Raptadu RAPTHADU Others 2,000 2,000 14.5681075753, 77.6472027346 9 Anantapur Penukonda Hidupur SWC, Hindupur SWC, Own ‐ 5,175 13.829591, 77.492024 10 Chittoor Chittoor Chittoor SWC, Chittoor SWC, Own ‐ 5,800 13.221828, 79.123509 11 Chittoor Madanapalle Pileru SWC, Pileru SWC, Own ‐ 2,150 13.651839, 78.936077 12 Chittoor Tirupathi Renigunta CWC, Renigunta CWC 5,000 20,000 13.631071, 79.504996 13 Chittoor Tirupathi Yerpedu PWS, Yerpedu CSC IG 70,000 70,000 13.6849607545, 79.5746439844 14 East Godavari Amalapuram Amalapuram SWC Katrenikona SWC, Own 10,000 10,000 16.580802, 82.153702 15 East Godavari Amalapuram Ravulapalem SWC (IG) Ravulapalem SWC, IG 15,000 15,000 16.75270,81.83716 16 East Godavari Amalapuram Razole SWC (IG) -

Sa;Irff'$O *Gn' 5Eu6' ,Fr6
Agr p6S $OoID udrf5 atl,6s0, e0 scrselolrsD 3?letdcr:5O ag., 5ey6r. SSbgqS 3o.1/?o2o, 66:lz.o3.zozl. a17 p6$ sroob erdrf aer6so ir?;$ffcr$o agr Seudr yo er6$Suef goO EeDrb 56fu ef d,er U$ erb6eJ6 lf6oerS 6der6D 6no$5 dr$) cqpe, oar55 Tentative Merit List agp E€5 Qe5 $odr $oaraOSapSa u of,r:g5 arary $odt Kr$Oo6a-SS a.t9.O3.2o2l s)oa 25.03.2021 66 )o$o$o 5.OO rto.erd4y 8gl" p6J $OolD udrt5 earoso ro se5e.nIci> ge7g6 Sevdr Sod$ 33 6$iloet bir$or1$er5,$arr ag," oo s6ii>er psdil agr D6S $ooo1D udr$ aar6s'O, e.3.J50.tu$o6 rp6 a0br6. SSdiDerSr www.westgodavari.org E?5 p€ S> 6o6o;otl$O$. b6535.$ur: SS ro.ggs955s788. rftt \ (1 Eer E6t $r0o1> erdrt5 OLU t' sa;irff'$o *gn' 5eu6' ,fr6 ) DATA ENTRY OPERATOR APPLICATIONS DATA UNDER NPCB PHC (VH/HH/OH) Month Maxi Marks Weight PGDCA Percen Certificate and mum age Computer Appli Date of Local/ Educational tage Name of Candidate and Age as on Gen issued by Year of Mark Secur Marks Total certificate Sl.No catio Mobile No Birth(as Date Caste Non qualification of Remarks Address 21.12.2020 der SADARAM in Passing s ed (Limit Marks issued n no. per SSC) Local (Degree) Marks case of of (Degr (Degr ed to regonsized (90%) claiming the Degree ee) ee) 10) institution reservation PARAVADA RAVI TEJA,S/O B.SC (BIO INELIGIBLE DUE TO NO 1 13 VENKATESWARA RAO,MONDURI 9030747244 9/13/1989 12/21/2020 31Y,3M,8D M BC-D LOCAL NO Apr-10 4700 3603 68.994 10 78.9936 MDTP CHEMISTRY) REQUIRED QUALIFICATION STREET,ELURU,W.G.DIST NETHALA SIRISHA,D/O B.SC(STATISTIC DHANAMJAYA,ASHOK 2 7 7013456065 6/28/1996 12/21/2020 24Y,5M,23D F SC LOCAL NO S AND Apr-17 10 8.23 74.07 3 77.07 PGDCA NAGAR,ROAD.NO.3.ELURU,W.G.D COMPUTER)) IST SHAIK SUBHANI,S/O SK.ABDUL NABI JOHNY,MUSLIM 3 15 9491034155 6/5/1995 12/21/2020 25Y,6M,16D M BC-E LOCAL NO BA May-17 10 8.18 73.62 3 76.62 PGDCA STREET,KOYYALAGUDEM,W.G.DIS T VOMMI DAVID KUMAR,S/O DCA,TALLY,DTP SATYANARAYANA,THIMMARUSU B.COM CASTE CERTIFICATE NOT 4 37 8328477819 5/18/1992 12/21/2020 28Y,7M,3D M BC-A LOCAL NO Mar-12 10 7.4 66.6 8 74.6 ,INTERNET ENCLOSED ONLINE RECEIPT STREET,ASHOK (COMPUTERS) APPLICATIONS ENCLOSED . -
The Andhra Pradesh Reorganisation Act 2014
jftLVªh lañ Mhñ ,yñ—(,u)04@0007@2003—14 REGISTERED NO. DL—(N)04/0007/2003—14 vlk/kkj.k EXTRAORDINARY Hkkx II — [k.M 1 PART II — Section 1 izkf/kdkj ls izdkf'kr PUBLISHED BY AUTHORITY lañ 6] ubZ fnYyh] 'kfuokj] ekpZ 1] 2014@ QkYxqu 10] 1935 ¼'kd½ No. 6] NEW DELHI, SATURDAY, MARCH 1, 2014/PHALGUNA 10, 1935 (SAKA) bl Hkkx esa fHkUu i`"B la[;k nh tkrh gS ftlls fd ;g vyx ladyu ds :i esa j[kk tk ldsA Separate paging is given to this Part in order that it may be filed as a separate compilation. MINISTRY OF LAW AND JUSTICE (Legislative Department) New Delhi, the 1st March, 2014/Phalguna 10, 1935 (Saka) The following Act of Parliament received the assent of the President on the 1st March, 2014, and is hereby published for general information:— THE ANDHRA PRADESH REORGANISATION ACT, 2014 NO. 6 OF 2014 [1st March, 2014.] An Act to provide for the reorganisation of the existing State of Andhra Pradesh and for matters connected therewith. BE it enacted by Parliament in the Sixty-fifth Year of the Republic of India as follows:— PART I PRELIMINARY 1. This Act may be called the Andhra Pradesh Reorganisation Act, 2014. Short title. 2. In this Act, unless the context otherwise requires,— Definitions. (a) “appointed day” means the day which the Central Government may, by notification in the Official Gazette, appoint; (b) “article” means an article of the Constitution; (c) “assembly constituency”, “council constituency” and “parliamentary constituency” have the same meanings as in the Representation of the People 43 of 1950. -

S.No. State Name State Code District Name District Code Sub District
Sub State District Village/Town S.no. State Name District Name Sub District Name District Village/Town Name Name of DA Code Code Code Code 1 Andhra Pradesh 28 Ananthapur 553 Ananthapuram 5330 A.Narayanapuramu 595096 Anantapur–Hindupur Urban Development Authority 2 Andhra Pradesh 28 Ananthapur 553 Penukonda 5356 Adadakulapalli 595434 Anantapur–Hindupur Urban Development Authority 3 Andhra Pradesh 28 Ananthapur 553 Ananthapuram 5330 Alamuru 595088 Anantapur–Hindupur Urban Development Authority 4 Andhra Pradesh 28 Ananthapur 553 Uravakonda 5317 Amidala 594897 Anantapur–Hindupur Urban Development Authority 5 Andhra Pradesh 28 Ananthapur 553 Ananthapuram 5330 Anantapur (CT) 595098 Anantapur–Hindupur Urban Development Authority 6 Andhra Pradesh 28 Ananthapur 553 Beluguppa 5318 Ankampalli 594908 Anantapur–Hindupur Urban Development Authority 7 Andhra Pradesh 28 Ananthapur 553 Bathalapalli 5337 Apparacheruvu 595170 Anantapur–Hindupur Urban Development Authority 8 Andhra Pradesh 28 Ananthapur 553 Beluguppa 5318 Avulenna 594910 Anantapur–Hindupur Urban Development Authority 9 Andhra Pradesh 28 Ananthapur 553 Bukkarayasamudram 5329 B.K.Samudram 595075 Anantapur–Hindupur Urban Development Authority 10 Andhra Pradesh 28 Ananthapur 553 Kothacheruvu 5346 Bandlapalle 595304 Anantapur–Hindupur Urban Development Authority 11 Andhra Pradesh 28 Ananthapur 553 Bathalapalli 5337 Bathalapalli 595169 Anantapur–Hindupur Urban Development Authority 12 Andhra Pradesh 28 Ananthapur 553 Beluguppa 5318 Beluguppa 594905 Anantapur–Hindupur Urban Development Authority -

Vijayawada Delhi Lucknow Bhopal Raipur Chandigarh Assault on Privacy Union Cabinet for Approval Sindhu Bhubaneswar Ranchi Dehradun Hyderabad *Late City Vol
Follow us on: @TheDailyPioneer facebook.com/dailypioneer RNI No.APENG/2018/764698 Established 1864 ANALYSIS 7 MONEY 8 SPORTS 11 Published From PEGASUS AFFAIR IS AN ELECTRICITY BILL MAY COME BEFORE CAKE WALK FOR VIJAYAWADA DELHI LUCKNOW BHOPAL RAIPUR CHANDIGARH ASSAULT ON PRIVACY UNION CABINET FOR APPROVAL SINDHU BHUBANESWAR RANCHI DEHRADUN HYDERABAD *LATE CITY VOL. 3 ISSUE 251 VIJAYAWADA, MONDAY, JULY 26, 2021; PAGES 12 `3 *Air Surcharge Extra if Applicable MADHAVAN ON THE IMPORTANCE OF BEING KIND, CARING AND COMPASSIONATE { Page 12 } www.dailypioneer.com PRESIDENT KOVIND COMPLETES FOUR WE MUST MOVE FORWARD WITH ‘NATION RAHUL GANDHI SLAMS GOVT FOR PACE KERALA VET DOC GETS PATENT FOR YEARS IN OFFICE FIRST, ALWAYS FIRST' MANTRA:PM MODI OF COVID-19 VACCINATIONS BIODIESEL FROM CHICKEN WASTE resident Ram Nath Kovind on Sunday completed four years in office, tressing on 'Nation First, Always First' mantra, Prime Minister Narendra ongress leader Rahul Gandhi on Sunday questioned the pace of fter waiting for more than seven years, John Abraham, a veterinary- the Rashtrapati Bhavan said, highlighting that he gave assent to 63 Modi said on Sunday that as the country enters its 75th year of COVID-19 vaccination, and said had the country's "Mann ki Baat" been doctor-turned-inventor, has finally received the patents for inventing PBills of the Union and state governments, besides lauding frontline SIndependence, every citizen should lead a "Bharat Jodo Andolan" in the Cunderstood, such would not have been the state. His remarks came Abiodiesel from slaughtered chicken waste that offers mileage of over 38 Covid warriors for saving countess lives across the country among same manner as Mahatma Gandhi had led the "Bharat Chhoro Andolan". -

The Andhra Pradesh Reorganisation Act, 2014
The Andhra Pradesh Reorganisation Act, 2014 Act 6 of 2014 Keyword(s): Telangana, Reorganisation DISCLAIMER: This document is being furnished to you for your information by PRS Legislative Research (PRS). The contents of this document have been obtained from sources PRS believes to be reliable. These contents have not been independently verified, and PRS makes no representation or warranty as to the accuracy, completeness or correctness. In some cases the Principal Act and/or Amendment Act may not be available. Principal Acts may or may not include subsequent amendments. For authoritative text, please contact the relevant state department concerned or refer to the latest government publication or the gazette notification. Any person using this material should take their own professional and legal advice before acting on any information contained in this document. PRS or any persons connected with it do not accept any liability arising from the use of this document. PRS or any persons connected with it shall not be in any way responsible for any loss, damage, or distress to any person on account of any action taken or not taken on the basis of this document. jftLVªh lañ Mhñ ,yñ—(,u)04@0007@2003—14 REGISTERED NO. DL—(N)04/0007/2003—14 vlk/kkj.k EXTRAORDINARY Hkkx II — [k.M 1 PART II — Section 1 izkf/kdkj ls izdkf'kr PUBLISHED BY AUTHORITY lañ 6] ubZ fnYyh] 'kfuokj] ekpZ 1] 2014@ QkYxqu 10] 1935 ¼'kd½ No. 6] NEW DELHI, SATURDAY, MARCH 1, 2014/PHALGUNA 10, 1935 (SAKA) bl Hkkx esa fHkUu i`"B la[;k nh tkrh gS ftlls fd ;g vyx ladyu ds :i esa j[kk tk ldsA Separate paging is given to this Part in order that it may be filed as a separate compilation.