High Snakebite Underreporting Rate in the Centre Region of Cameroon
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Review of the Evolution of Insecticide Resistance in Main Malaria Vectors in Cameroon from 1990 to 2017 Christophe Antonio-Nkondjio1,5*, N
Antonio-Nkondjio et al. Parasites & Vectors (2017) 10:472 DOI 10.1186/s13071-017-2417-9 REVIEW Open Access Review of the evolution of insecticide resistance in main malaria vectors in Cameroon from 1990 to 2017 Christophe Antonio-Nkondjio1,5*, N. Sonhafouo-Chiana2, C. S. Ngadjeu3, P. Doumbe-Belisse3, A. Talipouo3, L. Djamouko-Djonkam4, E. Kopya3, R. Bamou4, P. Awono-Ambene1 and Charles S. Wondji5 Abstract Background: Malaria remains a major public health threat in Cameroon and disease prevention is facing strong challenges due to the rapid expansion of insecticide resistance in vector populations. The present review presents an overview of published data on insecticide resistance in the main malaria vectors in Cameroon to assist in the elaboration of future and sustainable resistance management strategies. Methods: A systematic search on mosquito susceptibility to insecticides and insecticide resistance in malaria vectors in Cameroon was conducted using online bibliographic databases including PubMed, Google and Google Scholar. From each peer-reviewed paper, information on the year of the study, mosquito species, susceptibility levels, location, insecticides, data source and resistance mechanisms were extracted and inserted in a Microsoft Excel datasheet. The data collected were then analysed for assessing insecticide resistance evolution. Results: Thirty-three scientific publications were selected for the analysis. The rapid evolution of insecticide resistance across the country was reported from 2000 onward. Insecticide resistance was highly prevalent in both An. gambiae (s.l.) and An. funestus. DDT, permethrin, deltamethrin and bendiocarb appeared as the most affected compounds by resistance. From 2000 to 2017 a steady increase in the prevalence of kdr allele frequency was noted in almost all sites in An. -

MINMAP Région Du Centre SERVICES DECONCENTRES REGIONAUX ET DEPARTEMENTAUX
MINMAP Région du Centre SERVICES DECONCENTRES REGIONAUX ET DEPARTEMENTAUX N° Désignation des MO/MOD Nbre de Marchés Montant des Marchés N° page 1 Services déconcentrés Régionaux 19 2 278 252 000 4 Département de la Haute Sanaga 2 Services déconcentrés départementaux 6 291 434 000 7 3 COMMUNE DE BIBEY 2 77 000 000 8 4 COMMUNE DE LEMBE YEZOUM 8 119 000 000 8 5 COMMUNE DE MBANDJOCK 3 50 000 000 10 6 COMMUNE DE MINTA 5 152 500 000 10 7 COMMUNE DE NANGA-EBOKO 12 139 500 000 11 8 COMMUNE DE NKOTENG 5 76 000 000 13 9 COMMUNE DE NSEM 1 27 000 000 13 TOTAL 42 932 434 000 Département de la Lekié 10 Services déconcentrés départementaux 8 268 357 000 14 11 COMMUNE DE BATCHENGA 2 35 000 000 15 12 COMMUNE DE LOBO 8 247 000 000 15 13 COMMUNE DE MONATELE 11 171 500 000 16 14 COMMUNE DE SA'A 16 384 357 000 18 15 COMMUNE D'ELIG-MFOMO 7 125 000 000 20 16 COMMUNE D'EVODOULA 9 166 250 000 21 17 COMMUNE D'OBALA 14 223 500 000 22 18 COMMUNE D'OKOLA 22 752 956 000 24 19 COMMUNE D’EBEBDA 6 93 000 000 27 TOTAL 103 2 466 920 000 Département du Mbam et Inoubou 20 Services déconcentrés départementaux 4 86 000 000 28 21 COMMUNE DE BAFIA 5 75 500 000 28 22 COMMUNE DE BOKITO 12 213 000 000 29 23 COMMUNE DE KIIKI 4 134 000 000 31 24 COMMUNE DE KONYAMBETA 6 155 000 000 32 25 COMMUNE DE DEUK 2 77 000 000 33 26 COMMUNE DE MAKENENE 3 17 000 000 33 27 COMMUNE DE NDIKINIMEKI 4 84 000 000 34 28 COMMUNE D'OMBESSA 5 91 000 000 34 29 COMMUNE DE NITOUKOU 6 83 000 000 35 TOTAL 51 1 015 500 000 MINMAP/DIVISION DE LA PROGRAMMATION ET DU SUIVI DES MARCHES PUBLICS Page 1 de 88 N° Désignation -

Monitoring of HIV Viral Load, CD4 Cell Count, and Clinical Assessment
Articles Monitoring of HIV viral load, CD4 cell count, and clinical assessment versus clinical monitoring alone for antiretroviral therapy in low-resource settings (Stratall ANRS 12110/ESTHER): a cost-eff ectiveness analysis Sylvie Boyer, Laura March, Charles Kouanfack, Gabrièle Laborde-Balen, Patricia Marino, Avelin Fobang Aghokeng, Eitel Mpoudi-Ngole, Sinata Koulla-Shiro, Eric Delaporte, Maria Patrizia Carrieri, Bruno Spire, Christian Laurent, Jean-Paul Moatti, on behalf of the Stratall ANRS 12110/ESTHER Study Group* Summary Background In low-income countries, the use of laboratory monitoring of patients taking antiretroviral therapy Lancet Infect Dis 2013; (ART) remains controversial in view of persistent resource constraints. The Stratall trial did not show that clinical 13: 577–86 monitoring alone was non-inferior to laboratory and clinical monitoring in terms of immunological recovery. We Published Online aimed to evaluate the costs and cost-eff ectiveness of the ART monitoring approaches assessed in the Stratall trial. April 18, 2013 http://dx.doi.org/10.1016/ S1473-3099(13)70073-2 Methods The randomised, controlled, non-inferiority Stratall trial was done in a decentralised setting in Cameroon. See Comment page 560 Between May 23, 2006, and Jan 31, 2008, ART-naive adults were randomly assigned (1:1) to clinical monitoring *Members listed at end of paper (CLIN) or viral load and CD4 cell count plus clinical monitoring (LAB) and followed up for 24 months. We INSERM, UMR912 (SESSTIM), calculated costs, number of life-years saved (LYS), and incremental cost-eff ectiveness ratios (ICERs) with data Marseille, France (S Boyer PhD, from patients who had been followed up for at least 6 months. -

GEF Prodoc TRI Cameroon 28 02 18
International Union for the Conservation of Nature Country: Cameroon PROJECT DOCUMENT Project Title: Supporting Landscape Restoration and Sustainable Use of local plant species and tree products (Bambusa ssp, Irvingia spp, etc) for Biodiversity Conservation, Sustainable Livelihoods and Emissions Reduction in Cameroon BRIEF DESCRIPTION OF THE PROJECT The Republic of Cameroon has a diverse ecological landscape, earning her the title “Africa in Miniature”. The southern portions of Cameroon’s forests are part of the Congo Basin forest ecosystem, the second largest remaining contiguous block of rainforest on Earth, after the Amazon. In addition to extensive Mangrove belts, Cameroon also holds significant portions of the Lower Guinea Forest Ecosystems and zones of endemism extending into densely settled portions of the Western Highlands and Montagne forests. The North of the country comprising the Dry Sudano-Sahelian Savannah Zones is rich in wildlife, and home to dense human and livestock populations. Much of the population residing in these areas lives in extreme poverty. This diversity in biomes makes Cameroon one of the most important and unique hotspots for biodiversity in Africa. However, human population growth, migrations, livelihoods strategies, rudimentary technologies and unsustainable land use for agriculture and small-scale forestry, energy and livestock, are contributing to biodiversity loss and landscape degradation in Cameroon. Despite strong institutional frameworks, forest and environmental policies/legislation, and a human resource capital, Cameroon’s network of biomes that include all types of forests, tree-systems, savannahs, agricultural mosaics, drylands, etc., are progresively confronted by various forms of degradation. Degradation, which is progressive loss of ecosystem functions (food sources, water quality and availability, biodversity, soil fertility, etc), now threatens the livelihoods of millions of Cameroonians, especially vulnerable groups like women, children and indigenous populations. -

Dictionnaire Des Villages Du Mbam P
OFFICE DE LA RECHERCHE REPUBliQUE FEDERALE SCIENTIFIQUE ET TECHNIQUE DU OUT,RE·MER CAMEROUN CENTRE OR5TOM DE YAOUNDE DICTIONNAIRE DES _VILLAGES DU MBAM D'après la documentation réunie par ~la Section de Géographie de l'I.R.CAM.3 REPERTQIRE GEOGRAPHIQUE DU CAMEROUN FASCICULE n° 1 1 rR-GAM 8. P. '9J SH. n° 31 YAOUNDÉ Mai 1966 REPERTOIRE GEOGRAPHIQUE DU CAMEROUN Fasc. Tableau de la population du Cameroun, 68 p. Fév. 1965 SH, N° 17 Fasc. 2 Dictionnaire des villages du Dia et Lobo, 89 p. Juin 1965 SH. N° 22 Fasc. 3 Dictionnaire des villages de la Haute-Sanaga, 53 p. Août 1965 SH. N° 23 Fasc. 4 Dictionnaire des villages du Nyong et Mfoumou, 49 p. Octobre 1965 SH. N° 24 Fasc. 5 Dictionnaire des villages du Nyong et Soo 45 p. Novembre 1965 SH. N° 25 Fasc. 6 Dictionnaire des villages du Ntem 126 p. Décembre 1965 SH. N° 26 Fasc. 7 Dictionnaire- des villages de la Mefou 108 p. Janvier 1966 SH. N° 27 Fasc. 8 Dictionnaire des villages du Nyong et Kellé 51 p. Février 1966 SH. N° 28 Fasc. 9 Dictionnaire des villages de la Lékié 71 p. Mars 1966 SH. N° 29 Fasc. 10 Dictionnaire des villages de Kribi P. Mars 1966 SH. N° 30 Fasc. 11 Dictionnaire des villages du Mbam P. 60 Mai 1966 SH. N° 31 Fasc. 12 Dictionnaire des villages de Boumba Ngoko (en préparation) Fasc. 13 ùictionnaire des villages de Lom-et-Diérem (en préparation! omCE DE LA RECHERCHE SCIENTIFIQUE RERJBLlQUE FEDERALE ET TECHNI~E OUmE-MER ID CAMEROUN _ • _cee- -- - CENTRE ORSTOM DE YAOUNDE DICTIONNAIRE ~ VILLAGES DU ...........M B A M MAI 1!66 S.R. -

Centre Region Classifications
Centre Region Classifications Considering the World Bank list of economies (June 2020) OTHM centres have been classified into three separate regions: • Region 1: High income economies; • Region 2: Upper middle income economies; and • Region 3: Lower middle income and low income economies. Centres in the United Kingdom falls into Region 1 along with other high-income economies – (normal fees apply for all Region 1 Centres). Prospective centres and learners should visit www.othm.org.uk to find which region their centre falls into and pay the appropriate fees. Economy Income group Centre class Afghanistan Low income Region 3 Albania Upper middle income Region 2 Algeria Lower middle income Region 3 American Samoa Upper middle income Region 2 Andorra High income Region 1 Angola Lower middle income Region 3 Antigua and Barbuda High income Region 1 Argentina Upper middle income Region 2 Armenia Upper middle income Region 2 Aruba High income Region 1 Australia High income Region 1 Austria High income Region 1 Azerbaijan Upper middle income Region 2 Bahamas, The High income Region 1 Bahrain High income Region 1 Bangladesh Lower middle income Region 3 Barbados High income Region 1 Belarus Upper middle income Region 2 Belgium High income Region 1 Belize Upper middle income Region 2 Benin Lower middle income Region 3 Bermuda High income Region 1 Bhutan Lower middle income Region 3 Bolivia Lower middle income Region 3 Bosnia and Herzegovina Upper middle income Region 2 Botswana Upper middle income Region 2 Brazil Upper middle income Region 2 British -

Dictionnaire Des Villages De La Haute Sanaga a Été Entièrement Remise À Jour Et Corrigée En Fonction Des Derniers Renseignements Que Nous Possédons
OFFICE DE LA RECHERCHE REPUBLIQUE FEDEIlA~ SCIENTIFIQUE ET TECHNIQUE DU OUTRE-MER CAMEROUN CENTRE ORSTOM DE YAOUNDE DICTIONNAIR'E DES VILLAGES DE LA HAUTE SANAGA (2ème Editan) ~aprèS la documentation réunie ~-:-l ~ection de Géographie de l' ORST~ "~fUTOJkGEOGRAPHIQUE DU CAMEROUN FASCICULE N° 3 B. P. 193 SH. n° 50 YAOUNDE Août 1968 REPERTOIRE GEOGRAPHIQUE DU CAMEROUN Fasc. Tableau de la population du Cameroun, 68 p. Fév. 1965 SH. N° 17 Fasc. 2 Dictionnaire des villages du Dia et lobo, 89 p. Juin 1965 SH. N° 22 Fasc. 3 Dictionnaire des villages de la Haute-Sanaga, 44 p. Août 1968 SH. N° 50 (2éme édition) Fasc. 4 Dictionnaire des villages du Nyong et Mfoumou, 49 p. Octobre 1965 SH. N° 24 ~: Fasc. 5 Dictio~riaire des villages du Nyong et Soo 45 p. Novembre 1965 SH. N° 25 Fasc. 6 Dictionnaire des villages du Ntem 102 p. Juin 1968 SH. N° 46 (2ème édition) Fasc. 7 Dictionnaire des villages de la Mefou 108 p. Janvier 1966 SH. N° 27 Fa sc. 8 Dictionnaire des villages du Nyong et Kellé 51 p. Février 1966 SH. N° 28 Fa sc. 9 Dictionnaire des villages de la lékié 71 p. Mars 1966 SH. N° 29 Fasc. 10 Dictionnaire des villages de Kribi P. Mars 1966 SH. N° 30 Fasc. 11 Dictionnaire des villages du Mbam 60 P. Mai 1966 SH. N° 31 Fasc. 12 Dictionnaire des villages de Boumba Ngoko 34 p. Juin 1966 SH. 39 Fasc. 13 Dictionnaire des villages de lom-et-Djérem 35 p. Juillet 1967 SH. 40 Fasc. 14 Dictionnaire des villages de la Kadei 52 p. -

Typologie Des Planteurs Talba Nanga Eboko (À Dire D’Experts Et Basée Sur La Surface Possédée En Cacao) Bokito Mbandjok
Colloque de Dijon 20 et 21 novembre 2013 Nouvelles formes d’agriculture : pratiques ordinaires , débats publics et critique sociale T Heur et malheur d’une transition capitaliste : l’exemple des planteurs de cacao du Centre Cameroun Philippe Pédelahore Cirad, Dpt ES, UMR Innovation 1 Une étude sur les dynamiques de changement dans les systèmes agroforestiers à base de cacao du Cameroun Entre 1995 et 2013 la production de cacao a été multipliée par 2 (110.000 à 220.000 T) Que s’est-il passé ? 2 Depuis la libéralisation de la filière (1990) pas de données statistiques : enquêtes dans le principal bassin cacaoyer : deux zones représentatives Bassin cacaoyer historique Extension des SAF cacao (fronts pionniers) Talba Obala Echelle : 100 km Deux sites d’étude dans la province du Centre Obala Talba habitants/km2 111 < à 8 Dynamiques Anciennes Front Plantations 1910-1970 pionnier Yoko cacaoyères 1970-2010 Mbam Mobilité spatiale Zone de départ Zone et Kim des planteurs d’arrivée Ngoro Bafia Typologie des planteurs Talba Nanga Eboko (à dire d’experts et basée sur la surface possédée en cacao) Bokito Mbandjok La Lékié Obala Obala 2010 Yaoundé Ayos Akonolinga N Mbalmayo 0 50 km Talba ,2010 Densité population en 1998 Légende Choix de 82 planteurs < 8 habitants/km2 2 : capitale d’Etat (Echantillonnage stratifié) 8 à 16 habitants / km Yaoundé 16 à 35 habitants / km2 Ayos : ville secondaire Entretiens semi-directifs 35 à 100 habitants / km2 Talba : site d’étude Parcours de vie sur trois générations : 100 à 1500 habitants / km2 Stratégies et trajectoires d’accumulation > à 1500 habitants / km2 Mbam et Kim : département Résultats 5 Des trajectoires d’accumulation en surfaces cacaoyères différentes. -
Evidence of Iron Mineralization Channels in the Messondo Area (Centre-Cameroon) Using Geoelectrical (DC & IP) Methods: a Case Study
International Journal of Geosciences, 2014, 5, 346-361 Published Online March 2014 in SciRes. http://www.scirp.org/journal/ijg http://dx.doi.org/10.4236/ijg.2014.53034 Evidence of Iron Mineralization Channels in the Messondo Area (Centre-Cameroon) Using Geoelectrical (DC & IP) Methods: A Case Study Ngoumou Paul Claude1, Ndougsa-Mbarga Théophile2*, Assembe Stéphane Patrick1, Kofane Timoleon Crepin1 1Department of Physics, Faculty of Science, University of Yaoundé I, Yaoundé, Cameroon 2Department of Physics Advanced Teachers’ Training College, University of Yaoundé I, Yaoundé, Cameroon Email: *[email protected] Received 1 April 2013; revised 2 May 2013; accepted 4 June 2013 Copyright © 2014 by authors and Scientific Research Publishing Inc. This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/ Abstract A geophysical survey was conducted in the Kelle-Bidjocka village, Messondo subdivision, in the Centre Region, Cameroon. The data acquisition was made by combining Schlumberger profiling and electrical soundings along six (06) profiles of 1500 m in length for a total of 64 geoelectrical stations’ survey conducted through a variable mesh 100 m × 200 m, or 100 m × 300 m. The equipment used is the DC resistivimeter Syscal Junior 48 (Iris Instrument). Processing and model- ling of field data are made by using the Res2Dinv, Qwseln and Surfer software. The investigation methods used are electrical resistivity (DC) and induced polarization (IP) methods. The analyses and interpretations have helped to highlight areas of weakness or conductive discontinuities (fractures, faults, shear zones, etc.) in Precambrian gneiss formations, sometimes undergoing weathering processes. -
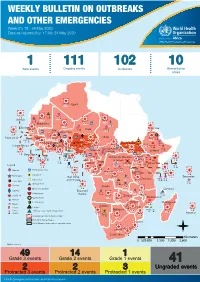
WEEKLY BULLETIN on OUTBREAKS and OTHER EMERGENCIES Week 21: 18 - 24 May 2020 Data As Reported By: 17:00; 24 May 2020
WEEKLY BULLETIN ON OUTBREAKS AND OTHER EMERGENCIES Week 21: 18 - 24 May 2020 Data as reported by: 17:00; 24 May 2020 REGIONAL OFFICE FOR Africa WHO Health Emergencies Programme 1 111 102 10 New events Ongoing events Outbreaks Humanitarian crises 8 306 600 Algeria 25 1 1 0 485 0 237 6 Gambia 7 0 675 60 945 61 Mauritania 13 0 1 030 65 Senegal 304 1 39 0Eritrea 3 047 35 Niger 7 635 37 Mali 380 3 Burkina Faso 95 4 0 3 7 0 Cabo Verdé Guinea 832 52 22 0 Chad 582 5 4 690 18 4 1 7 839 226 29 0 Nigeria 3 275 20Côte d’Ivoire South Sudan 1 873 895 15 604 1 274 3 32 0 Guinea-Bissau Ghana 987 202 4 400 159 7 551 92 381 12 139 0 2 0 4 0 Central African 25 0 Liberia 2 376 30 22 0 655 8 Benin Cameroon 4 732 26 Ethiopia 1 173 6 6 683 32 Republic 1 618 5 21 219 83 Sierra léone Togo 352 14 1 449 71 Uganda 120 18 Democratic Republic 812 3 339 3 14 0 401 3 1 214 51 of Congo 8 4 202 0 505 32 1 1 Congo 304 0 Gabon 3 463 2 280 Kenya 149 3 555 13 Legend 265 26 9 0 95 4 37 0 1 934 12 58 112 748 Rwanda Measles Humanitarian crisis 327 0 487 16 9 018 112 Burundi 299 9 11 0 Hepatitis E Monkeypox 42 1 2 305 66 Seychelles Sao Tome 5 0 Yellow fever Tanzania 857 0 70 0 Lassa fever and Principe 509 21 20 7 79 0 Dengue fever Cholera 1 441 37 1 043 12 Angola Ebola virus disease Comoros cVDPV2 Equatorial 83 4 2 0 Chikungunya Guinea 121 0 696 0 COVID-19 Malawi 69 4 Zambia Mozambique Guinea Worm 920 7 Anthrax Leishmaniasis Zimbabwe 2 305 18 Madagascar Malaria Namibia Floods Plague 286 1 Botswana 56 4 334 10 Cases Crimean-Congo haemorrhagic fever 236 865 226 527 2 Deaths 21 -

Programmation De La Passation Et De L'exécution Des Marchés Publics
PROGRAMMATION DE LA PASSATION ET DE L’EXÉCUTION DES MARCHÉS PUBLICS EXERCICE 2021 JOURNAUX DE PROGRAMMATION DES MARCHÉS DES SERVICES DÉCONCENTRÉS ET DES COLLECTIVITÉS TERRITORIALES DÉCENTRALISÉES RÉGION DU CENTRE EXERCICE 2021 SYNTHESE DES DONNEES SUR LA BASE DES INFORMATIONS RECUEILLIES N° Désignation des MO/MOD Nbre de Marchés Montant des Marchés N°Page 1 Services déconcentrés Régionaux 17 736 645 000 3 2 Communauté Urbaine de Yaoundé 62 10 459 000 000 5 Département de la Haute Sanaga 3 Services déconcentrés départementaux 2 24 000 000 10 4 Commune de Bibey 12 389 810 000 10 5 Commune de Lembe Yezoum 17 397 610 000 11 6 Commune de Mbandjock 12 214 000 000 12 7 Commune de Minta 8 184 500 000 12 8 Commune de Nanga Ebogo 21 372 860 000 13 9 Commune de Nkoteng 12 281 550 000 14 10 Commune de Nsem 5 158 050 000 15 TOTAL 89 2 022 380 000 Département de la Lekié 11 Services déconcentrés départementaux 9 427 000 000 16 12 Commune de Batchenga 8 194 000 000 17 13 Commune d'Ebebda 10 218 150 000 18 14 Commune d'Elig-Mfomo 8 174 000 000 19 15 Commune d'Evodoula 10 242 531 952 20 16 Commune de Lobo 11 512 809 000 21 17 Commune de Monatélé 12 288 500 000 22 18 commune d'Obala 11 147 000 000 23 19 commune d'Okola 14 363 657 000 24 20 commune de Sa'a 17 319 500 000 25 TOTAL 110 2 887 147 952 Département du Mbam et Inoubou 21 Services déconcentrés départementaux 6 144 385 000 27 22 Commune Bafia 13 213 500 000 27 23 Commune de Bokito 9 167 500 000 28 24 Commune de DEUK 17 379 500 000 29 25 Commune Kiiki 10 285 000 000 30 26 Commune Konyambeta 12 295 -

CAMEROON Education Environment, Water and Sanitation HIV/AIDS Project Income-Generating Activities
Health Child protection CAMEROON Education Environment, water and sanitation HIV/AIDS project Income-generating activities March 2012 – February 2015 Project overview OBJECTIVE Prevention, comprehensive care and promotion of the rights of the most vulnerable against HIV/AIDS in the health district of Okola, in the Centre Region. Project funded by the Région Ile de France and the city of Paris CONTEXT HIV/AIDS in Cameroon The 2/3 of the HIV positive people in the world live in the Sub-Saharan Africa. In Cameroon, it is estimated that they are 550,000, to which 300,000 HIV orphans must be added. The Centre is one of the most affected Region (out of the 10 Regions composing the country), as it accounts for 20% of the national HIV positive population. The most vulnerable people to the epidemic are : - Women, who for biological and social reasons (less control on their sexuality than men), make up 2/3 of the HIV positive persons in the country, -Young people (amongst the 60,000 affected people each year, half of them is from 15 to 24). The infection level is mainly due to the lack of information about HIV/AIDS. It implies a low condom use in Cameroon, while it is the most effective way to prevent HIV/AIDS. The access to HIV testing is also lacking: in 2004, 80% of women and about 90% of men in the area had never been tested for HIV. The comprehensive care services (therapeutic, psychosocial, economic support, etc.) for people living with HIV are rare, not to say missing in many rural areas.