Senior Resident Dermpath Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Rare Skin Cancers in General Practice
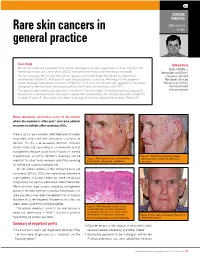
CLINICAL PRACTICE Skin cancer Rare skin cancers in series general practice Case study Anthony Dixon Mr LA has long been troubled with actinic damage to his skin, especially his face. He has had MBBS, FACRRM, is many squamous cell carcinomas (SCCs) removed and many solar keratoses managed. dermasurgeon and Director On this occasion Mr LA had two actinic lesions on his left cheek that failed to respond to of Research, Skin Alert cryotherapy (Figure 1). A biopsy of each site produced a surprise. Histology of the superior Skin Cancer Clinics and lesion revealed sebaceous carcinoma (Figure 2). This is an uncommon yet aggressive cutaneous Skincanceronly, Belmont, malignancy derived from sebaceous glands. The 5 year survival rate is 60–70%. Victoria. anthony@ The tumour was widely excised with a minimum 10 mm margin. A multidisciplinary approach skincanceronly.com resulted in a decision not to proceed to adjunctive radiotherapy. The wound was well healed by 8 weeks (Figure 3). Four years on there is no sign of local or regional recurrence (Figure 4). Many sebaceous carcinomas occur on the eyelids where the outcome is often poor;1 and some patients are prone to multiple other cutaneous SCCs. There is also a rare syndrome called Muir-torre of visceral neoplasms associated with sebaceous carcinoma on the skin.2 As this is an autosomal dominant condition, family history and counselling is an esssential part of management (enquire about family history of internal malignancies). A family member's diagnosis can be Figure 3. Satisfactory healing 8 weeks Figure 1. Two actinic lesions on the left face following wide excision of sebaceous important for other family members and offers screening have failed to respond to cryotherapy carcinoma for internal and cutaneous malignancies. -

Multiple Asymptomatic Papules on the Back of the Right Side of the Chest Angoori Gnaneshwar Rao
QUIZ Multiple Asymptomatic Papules on the Back of the Right Side of the Chest Angoori Gnaneshwar Rao A 43-year-old male presented with multiple asymptomatic complete blood picture, blood sugar, complete urine examination, papules on the back of the right side of the chest of 1 year blood urea, serum creatinine, liver function tests and serum duration. He was asymptomatic a year back then he developed lipid profile were normal. Fundus was normal. A slit skin smear small papules on the right side of the front of the chest initially for acid fast bacilli was negative. A punch biopsy from the and later on involved the front and back of the chest. No representative lesion subjected to histopathological examination history was suggestive of leprosy and hyperlipidemias. Family revealed a cyst with an intricately folded wall, lined by two to history was negative for similar problem. Examination revealed three layers of flattened squamous epithelium and the absence multiple skin-colored to yellowish papules distributed on the of the granular layer. Lobules of sebaceous glands were found front and back of the chest and shoulder region on the right embedded in cyst lining. The lumen was filled with amorphous side [Figure 1]. Also, there were multiple hyperpigmented eosinophilic material and multiple hair shafts [Figures 2-4]. macules on the right infrascapular region. There was no nerve thickening and no sensory deficit and there were no Question hypopigmented or anesthetic patches. Systemic examination did not reveal any abnormality. Routine investigations including What is your diagnosis? (Original) Multiple skin-colored to yellowish papules on the back of chest Figure 1: Figure 2: (Original) Histopathology of skin showing a cyst with an intricately folded and shoulder region on the right side wall lined by two to three layers of flattened squamous epithelium and the absence of granular layer. -

Atypical Compound Nevus Arising in Mature Cystic Ovarian Teratoma
J Cutan Pathol 2005: 32: 71–123 Copyright # Blackwell Munksgaard 2005 Blackwell Munksgaard. Printed in Denmark Journal of Cutaneous Pathology Abstracts of the Papers Presented at the 41st Annual Meeting of The American Society of Dermatopathology Westin Copley Place Boston, Massachusetts, USA October 14–17, 2004 These abstracts were presented in oral or poster format at the 41st Annual Meeting of The American Society of Dermatopathology on October 14–17, 2004. They are listed on the following pages in alphabetical order by the first author’s last name. 71 Abstracts IN SITU HYBRIDIZATION IS A VALUABLE DIAGNOSTIC A 37-year-old woman with diagnosis of Sjogren’s syndrome (SS) TOOL IN CUTANEOUS DEEP FUNGAL INFECTIONS presented with asymptomatic non-palpable purpura of the lower J.J. Abbott1, K.L. Hamacher2,A.G.Bridges2 and I. Ahmed1,2 extremities. Biopsy of a purpuric macule revealed a perivascular Departments of Laboratory Medicine and Pathology1 and and focally nodular lymphocytic infiltrate with large numbers of Dermatology2, plasma cells, seemingly around eccrine glands. There was no vascu- litis. The histologic findings in the skin were strikingly similar to those Mayo Clinic and Mayo Foundation, Rochester, MN, USA of salivary, parotid, and other ‘‘secretory’’ glands affected in SS. The cutaneous manifestations of SS highlighted in textbooks include Dimorphic fungal infections (histoplasmosis, blastomycosis, coccidiomy- xerosis, annular erythema, small-vessel vasculitis, and pigmented cosis, and cryptococcosis) can occur in immunocompromised and purpura. This case illustrates that purpura in skin of patients with healthy individuals. Cutaneous involvement is often secondary and SS may be caused by a peri-eccrine plasma-rich infiltrate. -

Soft Tissue Cytopathology: a Practical Approach Liron Pantanowitz, MD
4/1/2020 Soft Tissue Cytopathology: A Practical Approach Liron Pantanowitz, MD Department of Pathology University of Pittsburgh Medical Center [email protected] What does the clinician want to know? • Is the lesion of mesenchymal origin or not? • Is it begin or malignant? • If it is malignant: – Is it a small round cell tumor & if so what type? – Is this soft tissue neoplasm of low or high‐grade? Practical diagnostic categories used in soft tissue cytopathology 1 4/1/2020 Practical approach to interpret FNA of soft tissue lesions involves: 1. Predominant cell type present 2. Background pattern recognition Cell Type Stroma • Lipomatous • Myxoid • Spindle cells • Other • Giant cells • Round cells • Epithelioid • Pleomorphic Lipomatous Spindle cell Small round cell Fibrolipoma Leiomyosarcoma Ewing sarcoma Myxoid Epithelioid Pleomorphic Myxoid sarcoma Clear cell sarcoma Pleomorphic sarcoma 2 4/1/2020 CASE #1 • 45yr Man • Thigh mass (fatty) • CNB with TP (DQ stain) DQ Mag 20x ALT –Floret cells 3 4/1/2020 Adipocytic Lesions • Lipoma ‐ most common soft tissue neoplasm • Liposarcoma ‐ most common adult soft tissue sarcoma • Benign features: – Large, univacuolated adipocytes of uniform size – Small, bland nuclei without atypia • Malignant features: – Lipoblasts, pleomorphic giant cells or round cells – Vascular myxoid stroma • Pitfalls: Lipophages & pseudo‐lipoblasts • Fat easily destroyed (oil globules) & lost with preparation Lipoma & Variants . Angiolipoma (prominent vessels) . Myolipoma (smooth muscle) . Angiomyolipoma (vessels + smooth muscle) . Myelolipoma (hematopoietic elements) . Chondroid lipoma (chondromyxoid matrix) . Spindle cell lipoma (CD34+ spindle cells) . Pleomorphic lipoma . Intramuscular lipoma Lipoma 4 4/1/2020 Angiolipoma Myelolipoma Lipoblasts • Typically multivacuolated • Can be monovacuolated • Hyperchromatic nuclei • Irregular (scalloped) nuclei • Nucleoli not typically seen 5 4/1/2020 WD liposarcoma Layfield et al. -

Well-Differentiated Spindle Cell Liposarcoma
Modern Pathology (2010) 23, 729–736 & 2010 USCAP, Inc. All rights reserved 0893-3952/10 $32.00 729 Well-differentiated spindle cell liposarcoma (‘atypical spindle cell lipomatous tumor’) does not belong to the spectrum of atypical lipomatous tumor but has a close relationship to spindle cell lipoma: clinicopathologic, immunohistochemical, and molecular analysis of six cases Thomas Mentzel1, Gabriele Palmedo1 and Cornelius Kuhnen2 1Dermatopathologie, Friedrichshafen, Germany and 2Institute of Pathology, Medical Center, Mu¨nster, Germany Well-differentiated spindle cell liposarcoma represents a rare atypical/low-grade malignant lipogenic neoplasm that has been regarded as a variant of atypical lipomatous tumor. However, well-differentiated spindle cell liposarcoma tends to occur in subcutaneous tissue of the extremities, the trunk, and the head and neck region, contains slightly atypical spindled tumor cells often staining positively for CD34, and lacks an amplification of MDM2 and/or CDK4 in most of the cases analyzed. We studied a series of well-differentiated spindle cell liposarcomas arising in two female and four male patients (age of the patients ranged from 59 to 85 years). The neoplasms arose on the shoulder, the chest wall, the thigh, the lower leg, the back of the hand, and in paratesticular location. The size of the neoplasms ranged from 1.5 to 10 cm (mean: 6.0 cm). All neoplasms were completely excised. The neoplasms were confined to the subcutis in three cases, and in three cases, an infiltration of skeletal muscle was seen. Histologically, the variably cellular neoplasms were composed of atypical lipogenic cells showing variations in size and shape, and spindled tumor cells with slightly enlarged, often hyperchromatic nuclei. -

The Health-Related Quality of Life of Sarcoma Patients and Survivors In
Cancers 2020, 12 S1 of S7 Supplementary Materials The Health-Related Quality of Life of Sarcoma Patients and Survivors in Germany—Cross-Sectional Results of A Nationwide Observational Study (PROSa) Martin Eichler, Leopold Hentschel, Stephan Richter, Peter Hohenberger, Bernd Kasper, Dimosthenis Andreou, Daniel Pink, Jens Jakob, Susanne Singer, Robert Grützmann, Stephen Fung, Eva Wardelmann, Karin Arndt, Vitali Heidt, Christine Hofbauer, Marius Fried, Verena I. Gaidzik, Karl Verpoort, Marit Ahrens, Jürgen Weitz, Klaus-Dieter Schaser, Martin Bornhäuser, Jochen Schmitt, Markus K. Schuler and the PROSa study group Includes Entities We included sarcomas according to the following WHO classification. - Fletcher CDM, World Health Organization, International Agency for Research on Cancer, editors. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon: IARC Press; 2013. 468 p. (World Health Organization classification of tumours). - Kurman RJ, International Agency for Research on Cancer, World Health Organization, editors. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: International Agency for Research on Cancer; 2014. 307 p. (World Health Organization classification of tumours). - Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs—Part B: Prostate and Bladder Tumours. Eur Urol. 2016 Jul;70(1):106–19. - World Health Organization, Swerdlow SH, International Agency for Research on Cancer, editors. WHO classification of tumours of haematopoietic and lymphoid tissues: [... reflects the views of a working group that convened for an Editorial and Consensus Conference at the International Agency for Research on Cancer (IARC), Lyon, October 25 - 27, 2007]. 4. ed. -

Atypical Fibroxanthoma - Histological Diagnosis, Immunohistochemical Markers and Concepts of Therapy
ANTICANCER RESEARCH 35: 5717-5736 (2015) Review Atypical Fibroxanthoma - Histological Diagnosis, Immunohistochemical Markers and Concepts of Therapy MICHAEL KOCH1, ANNE J. FREUNDL2, ABBAS AGAIMY3, FRANKLIN KIESEWETTER2, JULIAN KÜNZEL4, IWONA CICHA1* and CHRISTOPH ALEXIOU1* 1Department of Otorhinolaryngology, Head and Neck Surgery, University Hospital Erlangen, Erlangen, Germany; 2Dermatology Clinic, 3Institute of Pathology, and 4ENT Department, University Hospital Mainz, Mainz, Germany Abstract. Background: Atypical fibroxanthoma (AFX) is an in 1962 (2). The name 'atypical fibroxanthoma' reflects the uncommon, rapidly growing cutaneous neoplasm of uncertain tumor composition, containing mainly xanthomatous-looking histogenesis. Thus far, there are no guidelines for diagnosis and cells and a varying proportion of fibrocytoid cells with therapy of this tumor. Patients and Methods: We included 18 variable, but usually marked cellular atypia (3). patients with 21 AFX, and 2,912 patients with a total of 2,939 According to previous reports, AFX chiefly occurs in the AFX cited in the literature between 1962 and 2014. Results: In sun-exposed head-and-neck area, especially in elderly males our cohort, excision with safety margin was performed in 100% (3). There are two disease peaks described: one within the 5th of primary tumors. Local recurrences were observed in 25% of to 7th decade of life and another one between the 7th and 8th primary tumors and parotid metastases in 5%. Ten-year disease- decade. The former disease peak is associated with lower specific survival was 100%. The literature research yielded 280 tumor frequency (21.8%) and tumors that do not necessarily relevant publications. Over 90% of the reported cases were manifest on skin areas exposed to sunlight (4). -

Atypical Fibroxanthoma and Pleomorphic Dermal Sarcoma - Two Stages of the Same Disease?
Case Report World Journal of Oral and Maxillofacial Surgery Published: 12 Jul, 2018 Atypical Fibroxanthoma and Pleomorphic Dermal Sarcoma - Two Stages of the Same Disease? Farhana Kapasi1*, Marta Cabral2, Phillip Ameerally1 and Antonia Barbieri1 1Department of Oral and Maxillofacial Surgery, Northampton General Hospital, UK 2Marta Cabral, The Royal Devon and Exeter NHS Foundation Trust, UK Abstract Atypical Fibroxanthoma and Pleomorphic Dermal Sarcoma are rare cutaneous neoplasm's which share clinical and Histopathological features which can pose a diagnostic challenge. Atypical Fibroxanthoma has been considered a low-grade malignancy whereas Pleomorphic Dermal Sarcoma has been considered high grade and aggressive. We report a case of an 83-year-old male with a history of Actinic Keratosis who presented with an erythematous papule on the right parietal scalp. Histopathological diagnosis was Atypical Fibroxanthoma. Seven months postoperatively, the patient developed a rapidly growing purple nodule at the operative site which was adherent to the skull. Histopathological diagnosis was Pleomorphic Dermal Sarcoma with bone involvement. We suggest that the recurrence rate and low aggressive potential of Atypical Fibroxanthoma may have been underestimated, as these tumours are rare and have not been widely reported in the literature. In this case, the tumour recurred following complete excision. The recurrence was the more infiltrative Pleomorphic Dermal Sarcoma, which reinforces the hypotheses that Atypical Fibroxanthoma may be the precursor lesion of Pleomorphic Dermal Sarcoma and that these are indeed two stages of the same disease rather than separate entities. Keywords: General dermatology; Medical dermatology; Head and neck oncology Introduction OPEN ACCESS Atypical Fibroxanthoma is a rare cutaneous tumour first described in 1963 by Elson Helwig [1]. -

Pleural Mesothelioma Dilated and the Pulmonary Trunk Was Occluded by a Large Embolus
Thorax 1993;48:409-410 409 lungs showed fibrosis, subpleural honeycomb Liposarcomatous changes, chronic bronchitis, and foci of bron- chopneumonia. The heart was slightly differentiation in diffuse enlarged (weight 430 g, right ventricle 120 g, left ventricle 230 g). The right side was Thorax: first published as 10.1136/thx.48.4.409 on 1 April 1993. Downloaded from pleural mesothelioma dilated and the pulmonary trunk was occluded by a large embolus. The left atrium J Krishna, M T Haqqani was occupied by a large myxoid tumour mass measuring 15 x 6 cm attached to a blood clot which extended into the pulmonary veins. The rest of the organs showed no abnor- Abstract malities. A case history is presented of a woman who died eight hours after hospital MICROSCOPICAL APPEARANCES admission with severe breathlessness. At The right pleura was diffusely infiltrated by necropsy the right lung was encased in a the tumour, which showed a sarcomatous thickened pleura with a large tumour. pattern with myxoid change and abundant Histological examination of the tumour typical lipoblasts containing sharply defined showed pleural mesothelioma with cytoplasmic vacuoles indenting hyperchro- liposarcomatous differentiation. The matic nuclei in the right upper lobe. This was lungs showed changes of asbestosis and confirmed on the electron microscope after the asbestos fibre count was significandy the tissue was post fixed in osmium tetraoxide raised. Liposarcomatous differentiation (fig 1). The right upper lobe also showed an in pleural mesothelioma has not been adjacent mesothelioma with an epithelial reported previously. glandular component (fig 2), uniformly nega- tive for carcinoembryonic antigen but (Thorax 1993;48:409-410) strongly positive for epithelial membrane antigen and cytokeratin. -

About Soft Tissue Sarcoma Overview and Types
cancer.org | 1.800.227.2345 About Soft Tissue Sarcoma Overview and Types If you've been diagnosed with soft tissue sarcoma or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is a Soft Tissue Sarcoma? Research and Statistics See the latest estimates for new cases of soft tissue sarcoma and deaths in the US and what research is currently being done. ● Key Statistics for Soft Tissue Sarcomas ● What's New in Soft Tissue Sarcoma Research? What Is a Soft Tissue Sarcoma? Cancer starts when cells start to grow out of control. Cells in nearly any part of the body can become cancer and can spread to other areas. To learn more about how cancers start and spread, see What Is Cancer?1 There are many types of soft tissue tumors, and not all of them are cancerous. Many benign tumors are found in soft tissues. The word benign means they're not cancer. These tumors can't spread to other parts of the body. Some soft tissue tumors behave 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 in ways between a cancer and a non-cancer. These are called intermediate soft tissue tumors. When the word sarcoma is part of the name of a disease, it means the tumor is malignant (cancer).A sarcoma is a type of cancer that starts in tissues like bone or muscle. Bone and soft tissue sarcomas are the main types of sarcoma. Soft tissue sarcomas can develop in soft tissues like fat, muscle, nerves, fibrous tissues, blood vessels, or deep skin tissues. -

Cutaneous Neoplasms
torr CALIFORNIA TUMOR TISSUE REGISTRY 1 03RD SEMI-ANNUAL CANCER SEMINAR ON CUTANEOUS NEOPLASMS CASE HISTORIES 00•MODERAT.0RS: . PHILIP E. LE~0FJ', M.Q. Dir;ector O:f Oermatopafholo.gy ;Ser:Vice Associate Professor of Clinical Pathology U.C.S.F.- Elermatopa~hology San Francisco, ·californla and TIMGTH1f' H. MCG~WMON'f,, M ~D. Assistant Clinical Professor U.C~S.F. - Dermatopathology San Francisco, California December 7, 1997 Sheraton Palace Hotel San Francisco, California PLATFORM CHAIR: CLAUDE 0. BURDICK, M.D. Director of laboratory ValleyCare Health System Pleasanton, California CASE RISTORJES 10.3"" Semi-Annual Seminar (Due to in$uffient material, Case 115 is • compo~ite to two ca!ICll with an identical diagnosis, Ace. #15523 and Ace #12395.) Ca.c 1#1 - As:c 1#28070: The patient was a 12-ycaro{)ld male who had a fairly long history ofa very small bump in the scalp of the temporal area, which had recently become greally enlarged. The submitting denna!ologist mentioned that this was a soliwy lesion, with no other lesions apparent (Contributed by Prescott Rasmussen, MD.) c-111- As:c #11543: The patient was a 60-year-old Caucasian female wbo presented with a S.O em right suprapalellar subcutaneous mass which was reported to be present and gradually increasing in size for a period of approximately rn·o years. There was no history of prior trauma, and the remainder ofthe clinical history and physical findings wcze uoremarialble. An cxeisional biopsy was performed. The specimeD consisted ofa 4.S x 1.1 em elliptical segment ofeentnllly dimpled skin which surmowlted a S.3 x 4.4 x 3.6 em delicately encapsulated. -

Mesenchymal) Tissues E
Bull. Org. mond. San 11974,) 50, 101-110 Bull. Wid Hith Org.j VIII. Tumours of the soft (mesenchymal) tissues E. WEISS 1 This is a classification oftumours offibrous tissue, fat, muscle, blood and lymph vessels, and mast cells, irrespective of the region of the body in which they arise. Tumours offibrous tissue are divided into fibroma, fibrosarcoma (including " canine haemangiopericytoma "), other sarcomas, equine sarcoid, and various tumour-like lesions. The histological appearance of the tamours is described and illustrated with photographs. For the purpose of this classification " soft tis- autonomic nervous system, the paraganglionic struc- sues" are defined as including all nonepithelial tures, and the mesothelial and synovial tissues. extraskeletal tissues of the body with the exception of This classification was developed together with the haematopoietic and lymphoid tissues, the glia, that of the skin (Part VII, page 79), and in describing the neuroectodermal tissues of the peripheral and some of the tumours reference is made to the skin. HISTOLOGICAL CLASSIFICATION AND NOMENCLATURE OF TUMOURS OF THE SOFT (MESENCHYMAL) TISSUES I. TUMOURS OF FIBROUS TISSUE C. RHABDOMYOMA A. FIBROMA D. RHABDOMYOSARCOMA 1. Fibroma durum IV. TUMOURS OF BLOOD AND 2. Fibroma molle LYMPH VESSELS 3. Myxoma (myxofibroma) A. CAVERNOUS HAEMANGIOMA B. FIBROSARCOMA B. MALIGNANT HAEMANGIOENDOTHELIOMA (ANGIO- 1. Fibrosarcoma SARCOMA) 2. " Canine haemangiopericytoma" C. GLOMUS TUMOUR C. OTHER SARCOMAS D. LYMPHANGIOMA D. EQUINE SARCOID E. LYMPHANGIOSARCOMA (MALIGNANT LYMPH- E. TUMOUR-LIKE LESIONS ANGIOMA) 1. Cutaneous fibrous polyp F. TUMOUR-LIKE LESIONS 2. Keloid and hyperplastic scar V. MESENCHYMAL TUMOURS OF 3. Calcinosis circumscripta PERIPHERAL NERVES II. TUMOURS OF FAT TISSUE VI.