Lieshout Van Lieshout, M.J.S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Turnedhead Adductedhip Truncal Curvature Syndrome
Archives ofDisease in Childhood 1994; 70: 515-519 515 Turned head adducted hip truncal curvature syndrome Arch Dis Child: first published as 10.1136/adc.70.6.515 on 1 June 1994. Downloaded from Chiaki Hamanishi, Seisuke Tanaka Abstract curvature. An epidemiological analysis was One hundred and eight neonates and carried out to determine whether the intra- infants who showed the clinical triad of a uterine environment of these asymmetrically head turned to one side, adduction con- deformed babies had been restricted. The tracture of the hip joint on the occipital clinical course of each feature of the clinical side of the turned head, and truncal cur- triad was also analysed to determine whether vature, which we named TAC syndrome, TAC syndrome is aetiologically related to any were studied. These cases included seven subsequent paediatric disorders. with congenital and five with late infantile dislocations of the hip joint and 14 who developed muscular torticollis. Forty one Patients and methods were among 7103 neonates examined by We studied a total of 108 cases with TAC one of the authors. An epidemiological syndrome. Of them, 41 were among a total analysis confirmed the aetiology of the number of 7103 neonates personally examined syndrome to be environmental. The side by one of the authors (CH) at newborn exami- to which the head was turned and that of nations conducted at hospitals in four cities the adducted hip contracture showed a since 1981. Thirteen were referred neonates. high correlation with the side of the The remaining 54 were among infants aged maternal spine on which the fetus had from 10 days to 3 months who were referred to been lying. -

The Primary Care Pediatrician and the Care of Children with Cleft Lip And/Or Cleft Palate Charlotte W
CLINICAL REPORT Guidance for the Clinician in Rendering Pediatric Care The Primary Care Pediatrician Charlotte W. Lewis, MD, MPH, FAAP, a Lisa S. Jacob, DDS, MS, b Christoph U. andLehmann, MD, the FAAP, FACMI, Care c SECTION ON ORALof HEALTH Children With Cleft Lip and/or Cleft Palate Orofacial clefts, specifically cleft lip and/or cleft palate (CL/P), are among the abstract most common congenital anomalies. CL/P vary in their location and severity and comprise 3 overarching groups: cleft lip (CL), cleft lip with cleft palate (CLP), and cleft palate alone (CP). CL/P may be associated with one of many syndromes that could further complicate a child’s needs. Care of patients aDivision of General Pediatrics and Hospital Medicine, Department of with CL/P spans prenatal diagnosis into adulthood. The appropriate timing Pediatrics, University of Washington School of Medicine and Seattle Children’s Hospital, Seattle, Washington; bGeorgetown Pediatric and order of specific cleft-related care are important factors for optimizing Dentistry and Orthodontics, Georgetown, Texas; and Departments of cBiomedical Informatics and Pediatrics, Vanderbilt University Medical outcomes; however, care should be individualized to meet the specific needs Center, Nashville, Tennessee of each patient and family. Children with CL/P should receive their specialty All three authors participated extensively in developing, researching, cleft-related care from a multidisciplinary cleft or craniofacial team with and writing the manuscript and revising it based on reviewers’ comments; Dr Lehmann made additional revisions after review by the sufficient patient and surgical volume to promote successful outcomes. board of directors. The primary care pediatrician at the child’s medical home has an essential This document is copyrighted and is property of the American role in making a timely diagnosis and referral; providing ongoing health Academy of Pediatrics and its Board of Directors. -

Soonerstart Automatic Qualifying Syndromes and Conditions 001
SoonerStart Automatic Qualifying Syndromes and Conditions 001 Abetalipoproteinemia 272.5 002 Acanthocytosis (see Abetalipoproteinemia) 272.5 003 Accutane, Fetal Effects of (see Fetal Retinoid Syndrome) 760.79 004 Acidemia, 2-Oxoglutaric 276.2 005 Acidemia, Glutaric I 277.8 006 Acidemia, Isovaleric 277.8 007 Acidemia, Methylmalonic 277.8 008 Acidemia, Propionic 277.8 009 Aciduria, 3-Methylglutaconic Type II 277.8 010 Aciduria, Argininosuccinic 270.6 011 Acoustic-Cervico-Oculo Syndrome (see Cervico-Oculo-Acoustic Syndrome) 759.89 012 Acrocephalopolysyndactyly Type II 759.89 013 Acrocephalosyndactyly Type I 755.55 014 Acrodysostosis 759.89 015 Acrofacial Dysostosis, Nager Type 756.0 016 Adams-Oliver Syndrome (see Limb and Scalp Defects, Adams-Oliver Type) 759.89 017 Adrenoleukodystrophy, Neonatal (see Cerebro-Hepato-Renal Syndrome) 759.89 018 Aglossia Congenita (see Hypoglossia-Hypodactylia) 759.89 019 Albinism, Ocular (includes Autosomal Recessive Type) 759.89 020 Albinism, Oculocutaneous, Brown Type (Type IV) 759.89 021 Albinism, Oculocutaneous, Tyrosinase Negative (Type IA) 759.89 022 Albinism, Oculocutaneous, Tyrosinase Positive (Type II) 759.89 023 Albinism, Oculocutaneous, Yellow Mutant (Type IB) 759.89 024 Albinism-Black Locks-Deafness 759.89 025 Albright Hereditary Osteodystrophy (see Parathyroid Hormone Resistance) 759.89 026 Alexander Disease 759.89 027 Alopecia - Mental Retardation 759.89 028 Alpers Disease 759.89 029 Alpha 1,4 - Glucosidase Deficiency (see Glycogenosis, Type IIA) 271.0 030 Alpha-L-Fucosidase Deficiency (see Fucosidosis) -

Research Article
z Available online at http://www.journalcra.com INTERNATIONAL JOURNAL OF CURRENT RESEARCH International Journal of Current Research Vol. 10, Issue, 07, pp.71222-71228, July, 2018 ISSN: 0975-833X RESEARCH ARTICLE THE TONGUE SPEAKS A LOT OF HEALTH. 1,*Dr. Firdous Shaikh, 2Dr. Sonia Sodhi, 3Dr Zeenat Fatema Farooqui and 4Dr. Lata Kale 1PG Student, Department of Oral Medicine and Radiology, CSMSS Dental College and Hospital, Aurangabad 2Professor, Department of Oral Medicine and Radiology, CSMSS Dental College and Hospital, Aurangabad 3Fatema Farooqui, Chief Medical Officer, Sri Ram Homeopathic Clinic and Research Center, Solapur 4Professor and Head, Department of Oral Medicine and Radiology, CSMSS Dental College and Hospital, Aurangabad ARTICLE INFO ABSTRACT Article History: Multifunctional organ of the human body without a bone yet strong is the tongue. It mainly consists Received 26th April, 2018 of the functional portion of muscle mass, mucosa, fat and the specialized tissue of taste i.e. the Received in revised form papillae. Diseases may either result from internal/ systemic causes of extrinsic causes like trauma, 14th May, 2018 infection, etc. A new method for classification has been proposed in this review for diseases of Accepted 09th June, 2018 tongue. This review mainly focuses on encompassing almost each aspect that the body reflects via its th Published online 30 July, 2018 mirror in mouth, the tongue. Key Words: Tongue, Diseases of Tongue, Discoloration of Tongue, Oral health, Hairy Tongue. Copyright © 2018, Firdous Shaikh et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. -

Orthopedic-Conditions-Treated.Pdf
Orthopedic and Orthopedic Surgery Conditions Treated Accessory navicular bone Achondroplasia ACL injury Acromioclavicular (AC) joint Acromioclavicular (AC) joint Adamantinoma arthritis sprain Aneurysmal bone cyst Angiosarcoma Ankle arthritis Apophysitis Arthrogryposis Aseptic necrosis Askin tumor Avascular necrosis Benign bone tumor Biceps tear Biceps tendinitis Blount’s disease Bone cancer Bone metastasis Bowlegged deformity Brachial plexus injury Brittle bone disease Broken ankle/broken foot Broken arm Broken collarbone Broken leg Broken wrist/broken hand Bunions Carpal tunnel syndrome Cavovarus foot deformity Cavus foot Cerebral palsy Cervical myelopathy Cervical radiculopathy Charcot-Marie-Tooth disease Chondrosarcoma Chordoma Chronic regional multifocal osteomyelitis Clubfoot Congenital hand deformities Congenital myasthenic syndromes Congenital pseudoarthrosis Contractures Desmoid tumors Discoid meniscus Dislocated elbow Dislocated shoulder Dislocation Dislocation – hip Dislocation – knee Dupuytren's contracture Early-onset scoliosis Ehlers-Danlos syndrome Elbow fracture Elbow impingement Elbow instability Elbow loose body Eosinophilic granuloma Epiphyseal dysplasia Ewing sarcoma Extra finger/toes Failed total hip replacement Failed total knee replacement Femoral nonunion Fibrosarcoma Fibrous dysplasia Fibular hemimelia Flatfeet Foot deformities Foot injuries Ganglion cyst Genu valgum Genu varum Giant cell tumor Golfer's elbow Gorham’s disease Growth plate arrest Growth plate fractures Hammertoe and mallet toe Heel cord contracture -

Crouzon Syndrome with Ophthalmological Complications
Journal of Rawalpindi Medical College (JRMC); 2012;16(1):80-81 Case Report Crouzon Syndrome With Ophthalmological Complications Rahela Nasir Paediatric Department, Capital Hospital, CDA Islamabad. Crouzon Syndrome is characterized by premature bilateral optic atrophy. Other facial features included a craniosynostosis. It has an autosomal dominant inheritance prominent nose and deep and narrow palate. No but represents fresh mutation also. Other craniofacial digital abnormalities were seen. No dental aplasia was abnormalities include ocular proptosis caused by shallow present. Systemic examination revealed no orbits with or without divergent strabismus. There may be abnormality. increased intracranial pressure for which surgical morcellation procedures are indicated. A case of He was diagnosed as a case of Crouzon syndrome craniosynostosis is reported which is diagnosed as Crouzon with ocular complications on clinical basis. He was Syndrome with ocular complications on clinical grounds. investigated for microcephaly and suspected Split craniotomy was performed by a neurosurgeon to craniosynostosis. Radiographs of skull showed small relieve raised intracranial pressure and to enhance brain sized skull with early closure of sutures and fontanelle growth. Crouzon Syndrome was originally described in 1912 suggestive of craniosynstosis(Fig 2). A hammered- by Crouzon in a mother and her daughter. It is an autosomal silver (beaten metal/ copper beaten) appearance was dominant inherited disorder but represents fresh mutation also seen due to raised intracranial pressure and also. Crouzon syndrome is characterized by premature compression of the developing brain on the fused craniosynostosis which is quite variable but the coronal suture is nearly always bilaterally involved. Craniofacial bone. CT scan brain with contrast was done which abnormalities include brachycephaly, shallow orbits and confirmed the features suggestive of craniosynostosis maxillary hypoplasia. -
Macrocephaly Information Sheet 6-13-19
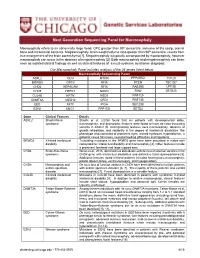
Next Generation Sequencing Panel for Macrocephaly Clinical Features: Macrocephaly refers to an abnormally large head, OFC greater than 98th percentile, inclusive of the scalp, cranial bone and intracranial contents. Megalencephaly, brain weight/volume ratio greater than 98th percentile, results from true enlargement of the brain parenchyma [1]. Megalencephaly is typically accompanied by macrocephaly, however macrocephaly can occur in the absence of megalencephaly [2]. Both macrocephaly and megalencephaly can been seen as isolated clinical findings as well as clinical features of a mutli-systemic syndromic diagnosis. Our Macrocephaly Panel includes analysis of the 36 genes listed below. Macrocephaly Sequencing Panel ASXL2 GLI3 MTOR PPP2R5D TCF20 BRWD3 GPC3 NFIA PTEN TBC1D7 CHD4 HEPACAM NFIX RAB39B UPF3B CHD8 HERC1 NONO RIN2 ZBTB20 CUL4B KPTN NSD1 RNF125 DNMT3A MED12 OFD1 RNF135 EED MITF PIGA SEC23B EZH2 MLC1 PPP1CB SETD2 Gene Clinical Features Details ASXL2 Shashi-Pena Shashi et al. (2016) found that six patients with developmental delay, syndrome macrocephaly, and dysmorphic features were found to have de novo truncating variants in ASXL2 [3]. Distinguishing features were macrocephaly, absence of growth retardation, and variability in the degree of intellectual disabilities The phenotype also consisted of prominent eyes, arched eyebrows, hypertelorism, a glabellar nevus flammeus, neonatal feeding difficulties and hypotonia. BRWD3 X-linked intellectual Truncating mutations in the BRWD3 gene have been described in males with disability nonsyndromic intellectual disability and macrocephaly [4]. Other features include a prominent forehead and large cupped ears. CHD4 Sifrim-Hitz-Weiss Weiss et al., 2016, identified five individuals with de novo missense variants in the syndrome CHD4 gene with intellectual disabilities and distinctive facial dysmorphisms [5]. -
Craniosynostosis and Related Disorders Mark S
CLINICAL REPORT Guidance for the Clinician in Rendering Pediatric Care Identifying the Misshapen Head: Craniosynostosis and Related Disorders Mark S. Dias, MD, FAAP, FAANS,a Thomas Samson, MD, FAAP,b Elias B. Rizk, MD, FAAP, FAANS,a Lance S. Governale, MD, FAAP, FAANS,c Joan T. Richtsmeier, PhD,d SECTION ON NEUROLOGIC SURGERY, SECTION ON PLASTIC AND RECONSTRUCTIVE SURGERY Pediatric care providers, pediatricians, pediatric subspecialty physicians, and abstract other health care providers should be able to recognize children with abnormal head shapes that occur as a result of both synostotic and aSection of Pediatric Neurosurgery, Department of Neurosurgery and deformational processes. The purpose of this clinical report is to review the bDivision of Plastic Surgery, Department of Surgery, College of characteristic head shape changes, as well as secondary craniofacial Medicine and dDepartment of Anthropology, College of the Liberal Arts characteristics, that occur in the setting of the various primary and Huck Institutes of the Life Sciences, Pennsylvania State University, State College, Pennsylvania; and cLillian S. Wells Department of craniosynostoses and deformations. As an introduction, the physiology and Neurosurgery, College of Medicine, University of Florida, Gainesville, genetics of skull growth as well as the pathophysiology underlying Florida craniosynostosis are reviewed. This is followed by a description of each type of Clinical reports from the American Academy of Pediatrics benefit from primary craniosynostosis (metopic, unicoronal, bicoronal, sagittal, lambdoid, expertise and resources of liaisons and internal (AAP) and external reviewers. However, clinical reports from the American Academy of and frontosphenoidal) and their resultant head shape changes, with an Pediatrics may not reflect the views of the liaisons or the emphasis on differentiating conditions that require surgical correction from organizations or government agencies that they represent. -

Craniofacial Development After Three Different Palatoplasties in Children Born with Isolated Cleft Palate
From the DEPARTMENT OF DENTAL MEDICINE Karolinska Institutet, Stockholm, Sweden CRANIOFACIAL DEVELOPMENT AFTER THREE DIFFERENT PALATOPLASTIES IN CHILDREN BORN WITH ISOLATED CLEFT PALATE Konstantinos A. Parikakis Stockholm 2018 All previously published papers were reproduced with permission from the publisher Published by Karolinska Institutet Printed by Eprint AB 2018 © Konstantinos A. Parikakis, 2018 ISBN 978-91-7831-277-1 Craniofacial development after three different palatoplasties in children born with isolated cleft palate THESIS FOR DOCTORAL DEGREE (Ph.D.) By Konstantinos A. Parikakis Principal Supervisor: Opponent: Associate Professor Agneta Karsten Professor David Rice Karolinska Institutet University of Helsinki Department of Dental Medicine Department of Orthodontics Division of Orthodontics and Pedodontics Examination Board: Co-supervisor(s): Associate Professor Magnus Becker Associate Professor Ola Larson University of Lund Karolinska University Hospital Department of Plastic and Reconstructive Surgery Department of Reconstructive Plastic Surgery Professor Britt Gustafsson Karolinska Institutet Department of Clinical Science, Intervention and Technology (CLINTEC) Division of Pediatrics Associate Professor Farhan Bazargani University of Örebro Centrum för Specialisttandvard Department of Orthodontics To Christina, little Anastasios and…forthcoming Vassilios “Wherever the art of Medicine is loved, there is also a love of Humanity” Hippocrates of Kos, c.460-370 B.C. ABSTRACT Introduction: Different palatoplasties are applied for -

Guidelines for Conducting Birth Defects Surveillance
NATIONAL BIRTH DEFECTS PREVENTION NETWORK HTTP://WWW.NBDPN.ORG Guidelines for Conducting Birth Defects Surveillance Edited By Lowell E. Sever, Ph.D. June 2004 Support for development, production, and distribution of these guidelines was provided by the Birth Defects State Research Partnerships Team, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention Copies of Guidelines for Conducting Birth Defects Surveillance can be viewed or downloaded from the NBDPN website at http://www.nbdpn.org/bdsurveillance.html. Comments and suggestions on this document are welcome. Submit comments to the Surveillance Guidelines and Standards Committee via e-mail at [email protected]. You may also contact a member of the NBDPN Executive Committee by accessing http://www.nbdpn.org and then selecting Network Officers and Committees. Suggested citation according to format of Uniform Requirements for Manuscripts ∗ Submitted to Biomedical Journals:∗ National Birth Defects Prevention Network (NBDPN). Guidelines for Conducting Birth Defects Surveillance. Sever, LE, ed. Atlanta, GA: National Birth Defects Prevention Network, Inc., June 2004. National Birth Defects Prevention Network, Inc. Web site: http://www.nbdpn.org E-mail: [email protected] ∗International Committee of Medical Journal Editors. Uniform requirements for manuscripts submitted to biomedical journals. Ann Intern Med 1988;108:258-265. We gratefully acknowledge the following individuals and organizations who contributed to developing, writing, editing, and producing this document. NBDPN SURVEILLANCE GUIDELINES AND STANDARDS COMMITTEE STEERING GROUP Carol Stanton, Committee Chair (CO) Larry Edmonds (CDC) F. John Meaney (AZ) Glenn Copeland (MI) Lisa Miller-Schalick (MA) Peter Langlois (TX) Leslie O’Leary (CDC) Cara Mai (CDC) EDITOR Lowell E. -

Craniofacial Center
Craniofacial Center The team concept The Craniofacial Center at Children’s Hospital New Orleans is dedicated to providing holistic, coordinated, state-of-the-art care to children with craniofacial differences. All team members specialize in complexities of caring for children with clefts and other craniofacial conditions. Children with clefts and craniofacial differences thrive best when cared for by specialists from many different disciplines. The team approach ensures that healthcare providers work together to implement a single, coordinated, and patient-centered treatment plan unique to your child. Craniofacial Center Craniofacial Pediatrics Genetics Otolaryngology The craniofacial pediatrician will Many babies with craniofacial Our otolaryngologists are surgeons diagnose your child and manage conditions have “isolated” problems with expertise in treating disorders medical problems related to that do not affect their general of the head, neck, ears, nose and their craniofacial differences. The health. The geneticist identifies throat in children of all ages. They physician guides your child’s overall those few patients who may have a assess and monitor your child’s treatment and works with other more complicated genetic condition hearing, ears, feeding, breathing team members to coordinate associated with other medical and speech development. specialty care. Your craniofacial problems and/or family history. They pediatrician will be familiar with all can advise you about the pros and Neurosurgery aspects of your child’s condition and cons of genetic testing, counsel the Neurosurgeons specialize in treating with your family’s needs and desires. family, and give information about children with abnormalities of the The craniofacial pediatrician will the prognosis and recurrence risks. -

Blueprint Genetics Craniosynostosis Panel
Craniosynostosis Panel Test code: MA2901 Is a 38 gene panel that includes assessment of non-coding variants. Is ideal for patients with craniosynostosis. About Craniosynostosis Craniosynostosis is defined as the premature fusion of one or more cranial sutures leading to secondary distortion of skull shape. It may result from a primary defect of ossification (primary craniosynostosis) or, more commonly, from a failure of brain growth (secondary craniosynostosis). Premature closure of the sutures (fibrous joints) causes the pressure inside of the head to increase and the skull or facial bones to change from a normal, symmetrical appearance resulting in skull deformities with a variable presentation. Craniosynostosis may occur in an isolated setting or as part of a syndrome with a variety of inheritance patterns and reccurrence risks. Craniosynostosis occurs in 1/2,200 live births. Availability 4 weeks Gene Set Description Genes in the Craniosynostosis Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ALPL Odontohypophosphatasia, Hypophosphatasia perinatal lethal, AD/AR 78 291 infantile, juvenile and adult forms ALX3 Frontonasal dysplasia type 1 AR 8 8 ALX4 Frontonasal dysplasia type 2, Parietal foramina AD/AR 15 24 BMP4 Microphthalmia, syndromic, Orofacial cleft AD 8 39 CDC45 Meier-Gorlin syndrome 7 AR 10 19 EDNRB Hirschsprung disease, ABCD syndrome, Waardenburg syndrome AD/AR 12 66 EFNB1 Craniofrontonasal dysplasia XL 28 116 ERF Craniosynostosis 4 AD 17 16 ESCO2 SC phocomelia syndrome, Roberts syndrome