Reduction of Delirium Risk and Postoperative Cognitive Dysfunction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Who's Afraid of the Brothers Grimm?: Socialization and Politization Through Fairy Tales
Who's Afraid of the Brothers Grimm?: Socialization and Politization through Fairy Tales Jack Zipes The Lion and the Unicorn, Volume 3, Number 2, Winter 1979-80, pp. 4-41 (Article) Published by Johns Hopkins University Press DOI: https://doi.org/10.1353/uni.0.0373 For additional information about this article https://muse.jhu.edu/article/247386 Access provided by University of Mary Washington & (Viva) (19 Sep 2017 17:43 GMT) Who's Afraid of the Brothers Grimm? Socialization and Politization through Fairy Tales Jack Zipes Over 170 years ago the Brothers Grimm began collecting original folk tales in Germany and stylized them into potent literary fairy tales. Since then these tales have exercised a pro- found influence on children and adults alike throughout the western world. Indeed, whatever form fairy tales in general have taken since the original publication of the Grimms' nar- ratives in 1812, the Brothers Grimm have been continually looking over our shoulders and making their presence felt. For most people this has not been so disturbing. However, during the last 15 years there has been a growing radical trend to over- throw the Grimms' benevolent rule in fairy-tale land by writers who believe that the Grimms' stories contribute to the creation of a false consciousness and reinforce an authoritarian sociali- zation process. This trend has appropriately been set by writers in the very homeland of the Grimms where literary revolutions have always been more common than real political ones.1 West German writers2 and critics have come to -

769531709.Pdf
A Service of Leibniz-Informationszentrum econstor Wirtschaft Leibniz Information Centre Make Your Publications Visible. zbw for Economics Piaszeck, Simon; Wenzel, Lars; Wolf, André Working Paper Regional diversity in the costs of electricity outages: Results for German counties HWWI Research Paper, No. 142 Provided in Cooperation with: Hamburg Institute of International Economics (HWWI) Suggested Citation: Piaszeck, Simon; Wenzel, Lars; Wolf, André (2013) : Regional diversity in the costs of electricity outages: Results for German counties, HWWI Research Paper, No. 142, Hamburgisches WeltWirtschaftsInstitut (HWWI), Hamburg This Version is available at: http://hdl.handle.net/10419/83646 Standard-Nutzungsbedingungen: Terms of use: Die Dokumente auf EconStor dürfen zu eigenen wissenschaftlichen Documents in EconStor may be saved and copied for your Zwecken und zum Privatgebrauch gespeichert und kopiert werden. personal and scholarly purposes. Sie dürfen die Dokumente nicht für öffentliche oder kommerzielle You are not to copy documents for public or commercial Zwecke vervielfältigen, öffentlich ausstellen, öffentlich zugänglich purposes, to exhibit the documents publicly, to make them machen, vertreiben oder anderweitig nutzen. publicly available on the internet, or to distribute or otherwise use the documents in public. Sofern die Verfasser die Dokumente unter Open-Content-Lizenzen (insbesondere CC-Lizenzen) zur Verfügung gestellt haben sollten, If the documents have been made available under an Open gelten abweichend von diesen Nutzungsbedingungen die in der dort Content Licence (especially Creative Commons Licences), you genannten Lizenz gewährten Nutzungsrechte. may exercise further usage rights as specified in the indicated licence. www.econstor.eu Regional Diversity in the Costs of Electricity Outages: Results for German Counties Simon Piaszeck, Lars Wenzel, André Wolf HWWI Research Paper 142 Hamburg Institute of International Economics (HWWI) | 2013 ISSN 1861-504X Lars Wenzel Hamburg Institute of International Economics (HWWI) Heimhuder Str. -

The Future of the German-Jewish Past: Memory and the Question of Antisemitism
Purdue University Purdue e-Pubs Purdue University Press Books Purdue University Press Fall 12-15-2020 The Future of the German-Jewish Past: Memory and the Question of Antisemitism Gideon Reuveni University of Sussex Diana University Franklin University of Sussex Follow this and additional works at: https://docs.lib.purdue.edu/purduepress_ebooks Part of the Jewish Studies Commons Recommended Citation Reuveni, Gideon, and Diana Franklin, The Future of the German-Jewish Past: Memory and the Question of Antisemitism. (2021). Purdue University Press. (Knowledge Unlatched Open Access Edition.) This document has been made available through Purdue e-Pubs, a service of the Purdue University Libraries. Please contact [email protected] for additional information. THE FUTURE OF THE GERMAN-JEWISH PAST THE FUTURE OF THE GERMAN-JEWISH PAST Memory and the Question of Antisemitism Edited by IDEON EUVENI AND G R DIANA FRANKLIN PURDUE UNIVERSITY PRESS | WEST LAFAYETTE, INDIANA Copyright 2021 by Purdue University. Printed in the United States of America. Cataloging-in-Publication data is on file at the Library of Congress. Paperback ISBN: 978-1-55753-711-9 An electronic version of this book is freely available, thanks to the support of librar- ies working with Knowledge Unlatched. KU is a collaborative initiative designed to make high-quality books Open Access for the public good. The Open Access ISBN for this book is 978-1-61249-703-7. Cover artwork: Painting by Arnold Daghani from What a Nice World, vol. 1, 185. The work is held in the University of Sussex Special Collections at The Keep, Arnold Daghani Collection, SxMs113/2/90. -

Historia Kosmopolity Z Zabrza
Angela Bajorek, Dariusz Walerjański Od Eckerta do Janoscha : historia kosmopolity z Zabrza Wieki Stare i Nowe 6(11), 140-150 2014 Angela Bajorek Uniwersytet Pedagogiczny im. KEN w Krakowie Dariusz Walerjański Towarzystwo Opieki nad Zabytkami Zabrza Od Eckerta do Janoscha Historia kosmopolity z Zabrza Gdyby nie zagmatwana historia jego i jego rodziny, wszyscy czytelnicy znaliby go dziś zapewne jako Horsta Eckerta alias Janosch. Ojciec pisarza — Johann Valen- tin Eckert (1903—1983), drobny handlarz, przemytnik, zwolennik bimbru i prze- mocy domowej, nazywa tak swego pierworodnego na cześć niemieckiego działacza nazistowskiego Horsta Wessela, zastrzelonego w 1930 roku przez członka komu- nistycznej partii i uznanego w III Rzeszy za męczennika za narodowy socjalizm. Johann Eckert jest tak bardzo zafascynowany postacią młodego Wessela, studenta prawa w Berlinie oraz autora tekstu hymnu partyjnego NSDAP, że w sierpniu 1933 roku w Zabrzu bierze czynny udział w postawieniu ogromnego 30tonowego głazu narzutowego z tablicą pamiątkową na cześć Horsta Wessela — sutenera, miłośnika prostytutek, jak mówili o nim jego przeciwnicy. Plac, na którym stał pomnik, został nazwany w 1939 roku również jego imieniem, dopiero po wojnie przemianowano go na plac Słowiański. Imię, które Janosch uważa za „niezniszczalną obrazę”1, pozostało na zawsze, a po obelisku nie ma już śladu, według lokalnej legendy nie został on bowiem w 1945 roku ani wywieziony, ani zniszczony, lecz z uwagi na swe gabaryty prawdopodobnie strącono go w głęboki dół wykopany pod nim2. Janosch urodził się 11 marca 1931 roku w zaborskiej robotniczej Porembie, w familoku przy ulicy Ciupkaweg 6 (Philipp Ciupka to znany zabrzański piekarz), późniejszej Piekarskiej3, który w 2005 roku wyburzono z uwagi na budowę Dro- 1 Email Janoscha do A. -

The German Netzdg As Role Model Or Cautionary Tale? Implications for the Debate on Social Media Liability
Fordham Intellectual Property, Media and Entertainment Law Journal Volume 31 XXXI Number 4 Article 4 2021 The German NetzDG as Role Model or Cautionary Tale? Implications for the Debate on Social Media Liability Patrick Zurth Ludwig Maximilian University of Munich (LMU), [email protected] Follow this and additional works at: https://ir.lawnet.fordham.edu/iplj Part of the International Law Commons, and the Internet Law Commons Recommended Citation Patrick Zurth, The German NetzDG as Role Model or Cautionary Tale? Implications for the Debate on Social Media Liability, 31 Fordham Intell. Prop. Media & Ent. L.J. 1084 (2021). Available at: https://ir.lawnet.fordham.edu/iplj/vol31/iss4/4 This Article is brought to you for free and open access by FLASH: The Fordham Law Archive of Scholarship and History. It has been accepted for inclusion in Fordham Intellectual Property, Media and Entertainment Law Journal by an authorized editor of FLASH: The Fordham Law Archive of Scholarship and History. For more information, please contact [email protected]. The German NetzDG as Role Model or Cautionary Tale? Implications for the Debate on Social Media Liability Cover Page Footnote Dr. iur., LL.M. (Stanford). Postdoctoral Fellow at the Chair for Private Law and Intellectual Property Law with Information- and IT-Law (GRUR-chair) (Prof. Dr. Matthias Leistner, LL.M. (Cambridge)) at Ludwig Maximilian University of Munich, Germany. Thanks to Professor David Freeman Engstrom, Abhilasha Vij, Jasmin Hohmann, Shazana Rohr, and the editorial board of the Fordham Intellectual Property, Media and Entertainment Law Journal for helpful comments and assistance. -

German Historical Institute London Bulletin Vol 34 (2012), No. 2
German Historical Institute London Bulletin Volume XXXIV, No. 2 November 2012 CONTENTS Articles Artistic Encounters: British Perspectives on Bavaria and Saxony in the Vormärz (Hannelore Putz) 3 ‘De-Industrialization’: A Research Project on the Societal History of Economic Change in Britain (1970–90) (Jörg Arnold) 34 Review Article The Hidden Transcript: The Deformation of the Self in Germany’s Dictatorial Regimes (Bernd Weisbrod) 61 Book Reviews David Rollason, Conrad Leyser, and Hannah Williams (eds.), England and the Continent in the Tenth Century: Studies in Honour of Wilhelm Levison (1876–1947) (Benjamin Pohl) 73 Craig Koslofsky, Evening’s Empire: A History of the Night in Early Modern Europe (Andreas Bähr) 78 Jerrold Seigel, Modernity and Bourgeois Life: Society, Politics, and Culture in England, France and Germany since 1750 (Andreas Fahrmeir) 84 Frank Lorenz Müller, Our Fritz: Emperor Frederick III and the Pol itical Culture of Imperial Germany (Martin Kohlrausch) 89 (cont.) Contents Anne Friedrichs, Das Empire als Aufgabe des Historikers. Historio graphie in imperialen Nationalstaaten: Großbritannien und Frankreich 1919–1968 (Roger Chickering) 94 J. A. S. Grenville, The Jews and Germans of Hamburg: The De - struc tion of a Civilization 1790–1945 (Moshe Zimmermann) 97 Ian Kershaw, The End: Hitler’s Germany, 1944–45 (Lothar Kettenacker) 103 Antje Robrecht, ‘Diplomaten in Hemdsärmeln?’ Auslands korre - s pon denten als Akteure in den deutsch-britischen Beziehungen 1945–1962 (Christian Haase) 107 Conference Reports Diverging Paths? -

World Scientists' Warning of a Climate Emergency
Supplemental File S1 for the article “World Scientists’ Warning of a Climate Emergency” published in BioScience by William J. Ripple, Christopher Wolf, Thomas M. Newsome, Phoebe Barnard, and William R. Moomaw. Contents: List of countries with scientist signatories (page 1); List of scientist signatories (pages 1-319). List of 153 countries with scientist signatories: Albania; Algeria; American Samoa; Andorra; Argentina; Australia; Austria; Bahamas (the); Bangladesh; Barbados; Belarus; Belgium; Belize; Benin; Bolivia (Plurinational State of); Botswana; Brazil; Brunei Darussalam; Bulgaria; Burkina Faso; Cambodia; Cameroon; Canada; Cayman Islands (the); Chad; Chile; China; Colombia; Congo (the Democratic Republic of the); Congo (the); Costa Rica; Côte d’Ivoire; Croatia; Cuba; Curaçao; Cyprus; Czech Republic (the); Denmark; Dominican Republic (the); Ecuador; Egypt; El Salvador; Estonia; Ethiopia; Faroe Islands (the); Fiji; Finland; France; French Guiana; French Polynesia; Georgia; Germany; Ghana; Greece; Guam; Guatemala; Guyana; Honduras; Hong Kong; Hungary; Iceland; India; Indonesia; Iran (Islamic Republic of); Iraq; Ireland; Israel; Italy; Jamaica; Japan; Jersey; Kazakhstan; Kenya; Kiribati; Korea (the Republic of); Lao People’s Democratic Republic (the); Latvia; Lebanon; Lesotho; Liberia; Liechtenstein; Lithuania; Luxembourg; Macedonia, Republic of (the former Yugoslavia); Madagascar; Malawi; Malaysia; Mali; Malta; Martinique; Mauritius; Mexico; Micronesia (Federated States of); Moldova (the Republic of); Morocco; Mozambique; Namibia; Nepal; -

Honour List 2018 © International Board on Books for Young People (IBBY), 2018
HONOUR LIST 2018 © International Board on Books for Young People (IBBY), 2018 IBBY Secretariat Nonnenweg 12, Postfach CH-4009 Basel, Switzerland Tel. [int. +4161] 272 29 17 Fax [int. +4161] 272 27 57 E-mail: [email protected] http://www.ibby.org Book selection and documentation: IBBY National Sections Editors: Susan Dewhirst, Liz Page and Luzmaria Stauffenegger Design and Cover: Vischer Vettiger Hartmann, Basel Lithography: VVH, Basel Printing: China Children’s Press and Publication Group (CCPPG) Cover illustration: Motifs from nominated books (Nos. 16, 36, 54, 57, 73, 77, 81, 86, 102, www.ijb.de 104, 108, 109, 125 ) We wish to kindly thank the International Youth Library, Munich for their help with the Bibliographic data and subject headings, and the China Children’s Press and Publication Group for their generous sponsoring of the printing of this catalogue. IBBY Honour List 2018 IBBY Honour List 2018 The IBBY Honour List is a biennial selection of This activity is one of the most effective ways of We use standard British English for the spelling outstanding, recently published children’s books, furthering IBBY’s objective of encouraging inter- foreign names of people and places. Furthermore, honouring writers, illustrators and translators national understanding and cooperation through we have respected the way in which the nomi- from IBBY member countries. children’s literature. nees themselves spell their names in Latin letters. As a general rule, we have written published The 2018 Honour List comprises 191 nomina- An IBBY Honour List has been published every book titles in italics and, whenever possible, tions in 50 different languages from 61 countries. -

Beltz & Gelberg
Beltz & Gelberg Foreign Rights Catalogue Spring 2011 Our agents: Greece: Literary Agency Iris Catherine Fragou Tel: 0030 210 24 32 473 Fax: 0030 210 24 35 042 [email protected] Israel: I. Pikarski Literary Agency Gabrielle Hertzmann Tel: ++972-3-527 01 59 Fax: ++972-3-527 01 60 [email protected] Italy: Agenzia Letteraria Internazionale Sibylle Kirchbach Tel.: ++39-02-865 445 Fax: ++0039-02-876 222 [email protected] Japan: Meike Marx Tel: ++81-45-226-9912 [email protected] Fax: ++81-45-22 69 923 Korea: Agency Chang Hea-Za Yu Tel: ++82-42-477 8816 Fax: ++82-42-477 6858 [email protected] MOMO Agency Geenie Han Tel: ++82-2-337 8606 Fax: ++82-2-337 8702 [email protected] Taiwan Bardon Chinese Media Agency & VR China: Jian-Mei Wang (China) [email protected] Mingju Hong (Taiwan) [email protected] Cynthia Chang (Taiwan) [email protected] Tel: ++886-2-3393 2585 Fax: ++886-2-2392 9577 VR China: Beijing Star Media Co, Ltd. Wang Xing [email protected] www.beltz.de Editorial Beltz & Gelberg 1 Dear Colleagues, again a new catalogue which we happily present to you! There are lots of outstanding titles, for example: Toto the Treasure Seeker: finally a new children’s book by Helme Heine about the greatest treasure in the world – love! A Book for Hanna: In her new novel Mirjam Pressler tells the moving story of 14-year-old Hanna who was deported to the concentration camp Theresienstadt during World War II. A novel based on a real-life story. -
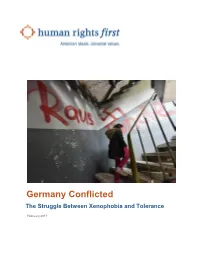
Germany Conflicted the Struggle Between Xenophobia and Tolerance
Germany Conflicted The Struggle Between Xenophobia and Tolerance February 2017 ON HUMAN RIGHTS, the United States must be a beacon. ACKNOWLEDGEMENTS Activists fighting for freedom around the globe continue to Research for this report was conducted by Susan Corke look to us for inspiration and count on us for support. and Erika Asgeirsson at Human Rights First and a team from Upholding human rights is not only a moral obligation; it’s a the University of Munich: Heather Painter, Britta vital national interest. America is strongest when our policies Schellenberg, and Klaus Wahl. Much of the research and actions match our values. consisted of interviews and consultations with human rights Human Rights First is an independent advocacy and action activists, government officials, national and international organization that challenges America to live up to its ideals. NGOs, multinational bodies, faith and interfaith groups, We believe American leadership is essential in the struggle scholars, and attorneys. We greatly appreciate their for human rights so we press the U.S. government and assistance and expertise. Rebecca Sheff, the former legal private companies to respect human rights and the rule of fellow with the antisemitism and extremism team, also law. When they don’t, we step in to demand reform, contributed to the research for this report during her time at accountability, and justice. Around the world, we work where Human Rights First. We are grateful for the team at Dechert we can best harness American influence to secure core LLP for their pro bono research on German law. At Human freedoms. Rights First, thanks to Sarah Graham for graphics and design; Meredith Kucherov and David Mizner for editorial We know that it is not enough to expose and protest injustice, assistance; Dora Illei for her research assistance; and so we create the political environment and policy solutions the communications team for their work on this report. -

ENLIGHTENMENT in the 21St Century
ENLIGHTENMENT in the 21st century WIR FORDERN: DIE KAMPAGNE n Die religiöse Diskriminierung in der Arbeitswelt muss „Gegen religiöse Diskriminierung ein Ende haben! In allen Sozialeinrichtungen, die aus am Arbeits platz“ (GerDiA) öffentlichen Mitteln finanziert werden, müssen die Grund rechte, insbesondere Religions- und Welt an- n Die Kampagne „Gegen religiöse Diskriminierung am schauungsfreiheit, gewährleistet sein. Arbeits platz“ (GerDiA) setzt sich für Weltanschauungs frei heit in der Arbeitswelt ein. Sie fordert, die Gültigkeit des Betriebs- n Das Betriebsverfassungsgesetz muss auch für kirchliche verfassungsgesetzes auf kirchliche Sozialeinrichtungen aus- Sozialeinrichtungen gelten. Es ist nicht einzusehen, zuweiten, damit die dort Beschäftigten zukünftig ihre private weshalb für kirchliche Einrichtungen andere Bestim- Lebensführung nicht mehr an kirchlichen Vorgaben ausrichten mungen gelten sollten als für die AWO. Der „besondere müssen und die üblichen Mitbestimmungsrechte erhalten. Tendenzschutz“ für Religionsgemeinschaften (BetrVG Informationen im Internet unter: § 118, Abs. 2) muss aufgehoben werden. www.religioese-diskriminierung.de bzw. www.gerdia.de n Angestellte kirchlicher Insti tutionen sollen die gleichen GerDiA-Koordinierungsstelle: Vera Muth, Tel.: 0174-97 88 66 4 Rechte wie andere Arbeitnehmer haben, also einen Mail: [email protected] Betriebsrat bilden und streiken dürfen. n Religionsgesellschaften als Arbeitgeber im sozialen Die Initiatoren der Kampagne: oder medizinischen Bereich dürfen nicht in die private -

THE FUTURE of the GERMAN-JEWISH PAST
THE FUTURE OF THE GERMAN-JEWISH PAST THE FUTURE OF THE GERMAN-JEWISH PAST Memory and the Question of Antisemitism Edited by IDEON EUVENI AND G R DIANA FRANKLIN PURDUE UNIVERSITY PRESS | WEST LAFAYETTE, INDIANA Copyright 2021 by Purdue University. All rights reserved. Printed in the United States of America. Cataloging-in-Publication data is on file at the Library of Congress. Paperback ISBN: 978-1-55753-711-9 ePub ISBN: 978-1-55753-729-4 ePDF ISBN: 978-1-55753-796-6 Cover artwork: Painting by Arnold Daghani from What a Nice World, vol. 1, 185. The work is held in the University of Sussex Special Collections at The Keep, Arnold Daghani Collection, SxMs113/2/90. The authors are grateful to the Centre for German-Jewish Studies at the University of Sussex for granting us permission to use the image for the cover. This book is dedicated to the memory of Professor Edward Timms OBE— scholar, mentor, friend, and founder of the Centre for German-Jewish Studies at the University of Sussex. CONTENTS Acknowledgments xi The Future of the German-Jewish Past Starts Here xiii Gideon Reuveni THE PERSONAL, THE HISTORICAL, AND THE MAKING OF GERMAN-JEWISH MEMORY “No More Mr. Nice Guy”: Questioning the Ideal of Assimilation 3 Alan Posener Generation in Flux: Diasporic Reflections on the Future of German-Jewishness 13 Sheer Ganor Home on the Balcony: New Initiatives for the Preservation of Documents and Material Objects Relating to German-Jewish History 25 Joachim Schlör From Object to Subject: Representing Jews and Jewishness at the Jewish Museum Berlin 37