Emergency Behavioral Health Services
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Annual Report of the Massachusetts Commission on Mental Diseases Of
TH** •O0«-»iA Public Document No. 117 SECOND ANNUAL EEPOET Massachusetts Commission on Mental Diseases THE COMMONWEALTH OF MASSACHUSETTS Year ending November 30, 1917. BOSTON: WRIGHT & POTTER PRINTING CO., STATE PRINTERS, 32 DERNE street. 1918. Publication of this Document approved by the Supervisor of Administration. TABLE OF CONTENTS. * PAGE Members of the Commission and List of Officers, 5 Letter of Transmission to Governor and Council, 7 Duties of the Commission, ..... 9,10 Activities of the Commission, ..... 10-15 Review of the Year: — All Classes under Care, ..... 16,17 The Insane, ....... 17-23 The Feeble-minded, . 23,24 The Epileptic, ....... 24,25 Report of the Pathologist, ..... 25-54 Reports of Committees on Nursing Service, . 54-61 Out-patient Departments, ..... 61-71 Commitments for Observation and Temporary Care, 71-73 Stability of Service, ...... 74,75 Capacity for Patients, ..... 76-78 Institutions : — Public 79-127 Private, . 127-130 Unlicensed Homes, . 131 Family Care of the Insane, .... 131-134 The Commission: — Proceedings of, . 135 Plans and Specifications, ..... 135 Estimates of State Expenses for 1918: — The Commission, 135, 136 Maintenance Appropriations, 136-138 Special Appropriations, .... 139-142 Financial Statement of Commission, 143, 144 Support Department, ..... 145-148 Deportations, ....... 148, 149 Transfers, ....... 150 Financial Department, . 150 General Matters : — New Legislation, ...... 151-160 Nineteen-year Statement as to Special Appropriations, 160-162 Financial Statistics, ....... 163-201 General Statistics, ....... 203-265 Directors^ of Institutions, ...... 266-278 Index, ......... 279-286 Digitized by the Internet Archive in 2010 with funding from Boston Library Consortium IVIember Libraries http://www.archive.org/details/annualreportofma1917mass2 Members of the Massachusetts Commission on Mental Diseases. -

Community Choice Acute Care Hospital Listing Effective July 1, 2017 When You Use a Community Choice Hospital, You Pay a $275 Inpatient Copay Per Calendar Quarter
UNICARE STATE INDEMNITY PLAN Community Choice Acute Care Hospital Listing Effective July 1, 2017 When you use a Community Choice hospital, you pay a $275 inpatient copay per calendar quarter. Community Choice members can also use additional hospitals for the same $275 copay for certain complex procedures and neonatal ICUs. To look for hospitals, go to unicarestateplan.com and, under the Quick Links tab on the Members page, select Look for health care providers. When you use non-Community Choice hospitals, your out-of-pocket costs are higher. Addison Gilbert Hospital Lawrence Memorial Hospital Anna Jaques Hospital Leominster Hospital (UMass Memorial) Athol Memorial Hospital Leonard Morse Hospital Baystate Franklin Medical Center Lowell General Hospital Baystate Medical Center Mary Lane Hospital (Baystate) Berkshire Medical Center Massachusetts Eye and Ear Beth Israel Deaconess Medical Center – Boston Melrose-Wakefield Hospital Beverly Hospital Mercy Medical Center Brockton Hospital Merrimack Valley Hospital Burbank Hospital (UMass Memorial) Milford Regional Medical Center Cambridge Hospital Milton Hospital (Beth Israel Deaconess) Cape Cod Hospital Morton Hospital Carney Hospital Mount Auburn Hospital Charlton Memorial Hospital Nashoba Valley Medical Center Children’s Hospital Boston Needham Hospital (Beth Israel Deaconess) Cooley Dickinson Hospital New England Baptist Hospital *Dana-Farber Cancer Institute (Boston location only) Noble Hospital (Baystate) Emerson Hospital Norwood Hospital Everett Hospital (formerly Whidden Hospital) Plymouth -
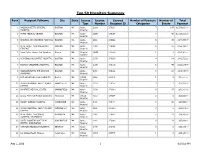
Top 50 Hospitals Summary
Top 50 Hospitals Summary Rank Recipient Fullname City State License License Covered Number of Payment Number of Total Type Number Recipient ID Categories Events Payment 1 MASSACHUSETTS GENERAL BOSTON MA Acute 2168 276130 7 147 $1,271,666.00 HOSPITAL Hospital 2 TUFTS MEDICAL CENTER BOSTON MA Acute 2299 276184 7 42 $1,028,318.00 Hospital 3 BRIGHAM AND WOMEN'S HOSPITAL BOSTON MA Acute 2341 276342 6 36 $170,355.00 Hospital 4 BETH ISRAEL DEACONESS MED BOSTON MA Acute 2069 276068 6 25 $155,269.00 CTR/EAST Hospital 5 Dana Farber Cancer Inst Inpatient Boston MA Hospital 2PW6 243229 1 3 $135,360.00 Satellite 6 NEW ENGLAND BAPTIST HOSPITAL BOSTON MA Acute 2059 276066 4 14 $112,722.00 Hospital 7 BOSTON CHILDREN'S HOSPITAL BOSTON MA Acute 2139 276116 6 49 $111,214.00 Hospital 8 MASSACHUSETTS EYE AND EAR BOSTON MA Acute 2167 276128 5 12 $106,067.00 INFIRMARY Hospital 9 Beth Israel Deaconess Medical Ctr Boston MA Virtual VL42 287371 1 1 $90,000.00 Hospital 10 UMASS MEMORIAL MED CTR/MEM WORCESTER MA Acute 2124 276107 3 4 $43,197.00 CAMPUS Hospital 11 BAYSTATE MEDICAL CENTER SPRINGFIELD MA Acute 2339 276340 6 67 $30,262.00 Hospital 12 Umass Memorial Medical Center Inc Worcester MA Virtual V111 287364 2 5 $25,638.00 Hospital 13 MOUNT AUBURN HOSPITAL CAMBRIDGE MA Acute 2071 276070 2 42 $24,536.00 Hospital 14 UMASS MEMORIAL MED CTR/UNIV WORCESTER MA Acute 2841 277550 3 5 $21,276.00 CAMPUS Hospital 15 BETH ISRAEL DEACONESS PLYMOUTH MA Acute 2082 276074 5 23 $18,763.00 HOSPITAL - PLYMOUTH Hospital 16 LAHEY HOSPITAL & MEDICAL BURLINGTON MA Acute 2342 276343 -
Community Hospitals at a Crossroads: Findings from an Examination of the Massachusetts Health Care System
COMMONWEALTH OF MASSACHUSETTS HEALTH POLICY COMMISSION Community Hospitals at a Crossroads: Findings from an Examination of the Massachusetts Health Care System March 2016 About the Health Policy Commission The Health Policy Commission (HPC) is an independent state agency established through Chapter 224 of the Acts of 2012, the Commonwealth’s landmark cost-containment law. The HPC, led by an 11-member board with diverse experience in health care, is charged with developing health policy to reduce overall cost growth while improving the quality of care, and monitoring the health care delivery and payment systems in Massachusetts. The HPC's mission is to advance a more transparent, accountable, and innovative health care system through independent policy leadership and investment programs. The HPC’s goal is better health and better care at a lower cost across the Commonwealth. II | HEALTH POLICY COMMISSION Community Hospitals at a Crossroads: Findings from an Examination of the Massachusetts Health Care System Introduction 2 Executive Summary 5 Section I. Definitions, Data Sources, and Methods 11 Section II. Background: Community Hospitals in Massachusetts 14 Section III. The Value of Community Hospitals to the Massachusetts Health Care System 22 Section IV. Challenges Facing Community Hospitals 35 Section V. From Community Hospitals to Community Health: Building a Path to a Thriving Community-Based Care System 68 COMMUNITY HOSPITALS AT A CROSSROADS | 1 Introduction Massachusetts has been a national leader in ensuring access to high quality health care for its residents and, with the passage of the Commonwealth’s landmark 2012 health care cost containment law, Massachusetts took significant steps to again lead the nation in efforts to slow the growth of health care costs. -

Wayfair Preferred (Narrow) Network Plan Hospitals
Wayfair Preferred (Narrow) Network Hospitals Hospital Name City State Addison Gilbert Hospital Gloucester MA Anna Jaques Hospital Newburyport MA BayRidge Hospital (acute psychiatric hospital) Lynn MA Beth Israel Deaconess Medical Center—Boston Boston MA Beth Israel Deaconess Hospital—Milton Milton MA Beth Israel Deaconess Hospital—Needham Campus Needham MA Beth Israel Deaconess Hospital—Plymouth Plymouth MA Beverly Hospital Beverly MA Boston Children’s Hospital Boston MA Boston Medical Center Boston MA Brigham and Women’s/Mass General Health Care Center at Patriot Place Foxborough MA Cambridge Health Alliance—Cambridge Campus Cambridge MA Cambridge Health Alliance—Somerville Campus Somerville MA Cambridge Health Alliance—Whidden Campus Everett MA Carney Hospital Dorchester MA Clinton Hospital Clinton MA Cooley Dickinson Hospital Northampton MA Emerson Hospital Concord MA Faulkner Hospital Jamaica Plain MA Good Samaritan Medical Center Brockton MA HealthAlliance Hospitals—Burbank Campus Fitchburg MA HealthAlliance Hospitals—Leominster Campus Leominster MA Heywood Hospital Gardner MA Holyoke Medical Center Holyoke MA Lahey Hospital and Medical Center Burlington MA Hospital Name City State Lahey Medical Center Peabody MA Lawrence General Hospital Lawrence MA Lawrence Memorial Hospital Medford MA Lowell General Hospital (includes the campus Lowell MA formerly known as Saints Medical Center) Massachusetts Eye and Ear®´ Infirmary Boston MA Mass General/North Shore Center for Outpatient Care Danvers MA Melrose-Wakefield Hospital Melrose MA Mercy -

EMERGENCY CARE HOSPITALS by City
EMERGENCY CARE HOSPITALS By City You can go to any hospital listed below for emergency care. You do not need a referral. Your provider will make plans for you to go to one of our participating hospitals when you need to for all other care. Emergency care hospitals are open 24 hours a day, seven days a week. ATHOL Massachusetts General CONCORD Athol Memorial Hospital Hospital Emerson Hospital 2033 Main St. 55 Fruit St. 133 Old Road to Nine Acre Athol, MA 01331 Boston, MA 02114 Corner (978) 249-3511 (617) 726-2000 Concord, MA 01742 ATTLEBOROUGH New England Medical Center (978) 369-1400 Sturdy Memorial Hospital 750 Washington St. EVERETT 211 Park St. Boston, MA 02111 Whidden Memorial Hospital Attleboro, MA 02703 (617) 636-5000 103 Garland St. (508) 236-8111 St. Elizabeth’s Medical Center Everett, MA 02149 AYER 736 Cambridge St. (617) 389-6270 Deaconess-Nashoba Hospital Boston, MA 02135 FALL RIVER 200 Groton Ave. (617) 789-3000 Charlton Memorial Hospital Ayer, MA 01432 BROCKTON 363 Highland Ave. (978) 772-0200 Brockton Hospital Fall River, MA 02720 BEVERLY 680 Centre St. (508) 679-3131 Beverly Hospital Brockton, MA 02302 St. Anne’s Hospital 85 Herrick St. (508) 941-7000 795 Middle St. Beverly, MA 01915 Caritas Good Samaritan Fall River, MA 02721 (978) 922-3000 Hospital (508) 674-5741 BOSTON 235 North Pearl St. FALMOUTH Beth Israel-Deaconess Brockton, MA 02301 Falmouth Hospital Medical Center (508) 427-3000 100 Ter Heun Dr. 330 Brookline Ave. BURLINGTON Falmouth, MA 02540 Boston, MA 02215 Lahey Clinic (508) 548-5300 (617) 667-7000 41 Mall Rd. -

Curtis Penney, DO
Curtis W. Penney, D.O. Diplomate, American Board of Psychiatry and Neurology (Neurology) 4285 Coventry Drive South Fargo, North Dakota 58104 Telephone: 701-205-0390 Cell: 701-446-7691 Curriculum Vitae Education Academic Preparation: Doctor of Osteopathy (D.O.) University of New England College of Osteopathic Medicine Hills Beach Road Biddeford, Maine 04005 (Programme: 1989-1993) Doctor of Ministry (D.Min.) Department of Psychology Andover Newton Theological School 210 Herrick Road Newton Centre, Massachusetts 02159 (Programme: 1980-1982) Doctoral Degree awarded in Psychology and Clinical Studies Doctoral Dissertation entitled: “The Role of Language from a Psychological and Theological Perspective: Understanding the Pastoral Counselor as Psychologist and Theologian” Master of Divinity (M.Div.) Andover Newton Theological School 210 Herrick Road Newton Centre, Massachusetts 02159 (Programme: 1974-1978; concentration in Psychology Bachelor of Arts (B.A.) Eastern Nazarene College 21 E. Elm Avenue Wollaston, Massachusetts 02170 (Programme: 1969-1973; major in Psychology) Post-graduate Medical Training: Internship: Internal Medicine (Preliminary Year) Department of Medicine Carney Hospital 2100 Dorchester Avenue Boston, Massachusetts 02124 (PGY I: 1993-1994) Dr. Curtis W. Penney Page 2 Residency in Neurology: Neurological Unit Boston City Hospital 818 Harrison Avenue 02118 (PGY II, III and IV; Chief Resident in Neurology: 1996-1997) Residency completed in Association with: Department of Neurology St. Elizabeth’s Medical Center Boston, Massachusetts -
Manager and Executive Compensation in Hospitals and Health Systems Survey Report
2019 Manager and Executive Compensation in Hospitals and Health Systems Survey Report Survey data effective January 1, 2019 © 2019 SullivanCotter, Inc. All rights reserved. 200 W. Madison Street, Suite 2450 Chicago, IL 60606-3416 2019 MANAGER AND EXECUTIVE COMPENSATION IN HOSPITALS AND HEALTH SYSTEMS SURVEY REPORT Survey data effective January 1, 2019 LICENSE AGREEMENT LICENSE AGREEMENT By accessing or downloading the Survey Report files online or by opening the packaging for this Survey Report, you agree to the terms of this License Agreement (this “Agreement”). If you do not agree to these terms and have not yet accessed or downloaded the Survey Report files or opened the packaging for this Survey Report, you may cancel your online purchase or download at this time or you may return this Survey Report to SullivanCotter, Inc. for a full refund within thirty (30) days of receipt, but you may not access or download the Survey Report files or open the packaging for, or otherwise use, this Survey Report. Accessing or downloading the Survey Report files or opening the packaging, or otherwise using, this Survey Report binds you to this Agreement. This Agreement is entered into by and between SullivanCotter, Inc. ("SullivanCotter") and the purchaser or participant of this Survey Report (the “Licensee”). In consideration of the mutual covenants in this Agreement, SullivanCotter and the Licensee agree as follows: Grant of License. This Survey Report contains the aggregation of compensation data and other data provided to SullivanCotter by its survey participants, statistics, tables, reports, research, aggregations, calculations, data analysis, formulas, summaries, content, text and other information and materials provided to the Licensee by SullivanCotter through any other means, whether digital or hard copy, related thereto (the “Aggregated Data”). -
Fy 2018 Massachusetts Hospital Profiles Technical Appendix January 2020
CENTER FOR HEALTH INFORMATION AND ANALYSIS FY 2018 MASSACHUSETTS HOSPITAL PROFILES TECHNICAL APPENDIX JANUARY 2020 Publication Number 20-30-CHIA-02 CHIA FY18 Massachusetts Acute Care Hospitals (January 2020) TECHNICAL APPENDIX Table of Contents Introduction ....................................................................................................................................................................................... 2 Multi-Acute Hospital System Affiliation and Location ................................................................................................................... 3 Regional Definitions ..................................................................................................................................................................... 4 Special Designations.................................................................................................................................................................... 6 Hospital Types ............................................................................................................................................................................. 7 At a Glance ....................................................................................................................................................................................... 9 Acute Hospital Profiles: Services ................................................................................................................................................... -

758 Hospitals Penalized for Patient Safety in 2016
758 Hospitals Penalized For Patient Safety In 2016 Medicare is lowering its 2016 payments by 1 percent for 758 hospitals with high rates of potentially avoidable infections and complications such as blood clots, bed sores and falls. This is the second year of the Hospital-Acquired Conditions Reduction Program, which was mandated by the federal health law to reduce patient injuries. Below are the hospitals being penalized. Source: Kaiser Health News analysis of data from the U.S. Centers for Medicare & Medicaid Services Also Penalized in Hospital City State 2015 ALASKA REGIONAL HOSPITAL ANCHORAGE AK Y MT EDGECUMBE HOSPITAL SITKA AK CENTRAL PENINSULA GENERAL HOSPITAL SOLDOTNA AK BROOKWOOD MEDICAL CENTER BIRMINGHAM AL Y L V STABLER MEMORIAL HOSPITAL GREENVILLE AL SPRINGHILL MEMORIAL HOSPITAL MOBILE AL Y SHOALS HOSPITAL MUSCLE SHOALS AL RUSSELLVILLE HOSPITAL RUSSELLVILLE AL Y D C H REGIONAL MEDICAL CENTER TUSCALOOSA AL Y NORTHWEST MEDICAL CENTER WINFIELD AL WHITE RIVER MEDICAL CENTER BATESVILLE AR Y CHAMBERS MEMORIAL HOSPITAL DANVILLE AR Y PHYSICIANS' SPECIALTY HOSPITAL FAYETTEVILLE AR Y WASHINGTON REGIONAL MEDICAL CENTER FAYETTEVILLE AR WADLEY REGIONAL MEDICAL CENTER AT HOPE HOPE AR NATIONAL PARK MEDICAL CENTER HOT SPRINGS AR NORTH METRO MEDICAL CENTER JACKSONVILLE AR ST BERNARDS MEDICAL CENTER JONESBORO AR Y BAPTIST HEALTH MEDICAL CENTER-HOT SPRINGS COUNTY MALVERN AR ARIZONA ORTHOPEDIC AND SURGICAL SPECIALITY HOSP CHANDLER AZ Y FLAGSTAFF MEDICAL CENTER FLAGSTAFF AZ FLORENCE HOSPITAL AT ANTHEM, LLC FLORENCE AZ Y BANNER THUNDERBIRD MEDICAL -

114.1 CMR 41.00: Rates of Payment for Services Provided to Industrial Accident Patients by Hospitals
The Commonwealth of Massachusetts Executive Office of Health and Human Services One Ashburton Place, Room 1109 Boston, MA 02108 CHARLES D. BAKER Tel: (617) 573-1600 Governor Fax: (627) 573-1891 www.mass.gov/eohhs KARYN E. POLITO Lieutenant Governor MARYLOU SUDDERS Secretary Administrative Bulletin 17-01 114.1 CMR 41.00: Rates of Payment for Services Provided to Industrial Accident Patients by Hospitals Effective January 1, 2017 Publication of Payment on Account Factors (PAFs) for Hospital Services The Executive Office of Health and Human Services (EOHHS), pursuant to 114.1 CMR 41.05(1) and (3), is publishing the Payment on Account Factors (PAF) for acute and non-acute hospital services rendered to industrial accident patients. The application of the PAF to all billed charges payable pursuant to 114.1 CMR 41.00 results in the payment of the average percentage of charges paid by the private sector to each hospital for its services and shall be deemed to meet the test of reasonable cost of medical services prescribed by M.G.L. c. 152, the Workers’ Compensation Act. No lesser amount shall be paid unless agreed to by the provider, insurer, and employer. Provided below are the PAFs for acute and non-acute hospital services rendered on or after January 1, 2017. Acute Hospitals PAF % Anna Jaques Hospital 55.42% Athol Memorial Hospital 35.62% Baystate Franklin Medical Center 51.90% Baystate Mary Lane Hospital 50.36% Baystate Medical Center 57.98% Baystate Wing Hospital 43.07% Berkshire Medical Center 66.85% Beth Israel Deaconess Hospital - Milton -

BCRP Brochure 2021 Class
Boston Combined Residency Program This brochure describes the residency program as we assume it will -19 exist will in be JulyThe 2021, Pediatric by which time Residency authorities Training Program predict a vaccine to COVID of available. If thatBoston is not the Children’s case and the Hospital pandemic is still active, the program Harvard Medical School will be very similar but many of the and educational conferences and other group activities Bostonwill be virtual Medical instead Center Boston University School of Medicine of in-person, as they are today. August 2020 edi,on CLASS OF 2021.. BOSTON COMBINED RESIDENCY PROGRAM Boston Medical Center Boston Children’s Hospital CONTENTS History…………........................... 3 Rotation # descriptions.................. 47# Global health fellowships............ 84# BCRP…........................................ 3# Night call................................... 53# Global health grants………….… 84 # Boston Children’s Hospital........... 3# Longitudinal ambulatory.............. 54# Diversity and Inclusion................. 84# Boston Medical Center................. 8# Electives………………………….. 55# Salaries and benefits.................... 87# People……................................... 11 Individualized curriculum............ 56# Child care................................... 88# Program director biosketches...... 11# Academic development block.. 56# O$ce of fellowship training....... 88# Residency program leadership..... 12# Education.................................... 57# Cost of living..............................