Appendix G Patient Safety Indicators Appendices
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medical Policy Ultrasound Accelerated Fracture Healing Device
Medical Policy Ultrasound Accelerated Fracture Healing Device Table of Contents Policy: Commercial Coding Information Information Pertaining to All Policies Policy: Medicare Description References Authorization Information Policy History Policy Number: 497 BCBSA Reference Number: 1.01.05 Related Policies Electrical Stimulation of the Spine as an Adjunct to Spinal Fusion Procedures, #498 Electrical Bone Growth Stimulation of the Appendicular Skeleton, #499 Bone Morphogenetic Protein, #097 Policy Commercial Members: Managed Care (HMO and POS), PPO, and Indemnity Members Low-intensity ultrasound treatment may be MEDICALLY NECESSARY when used as an adjunct to conventional management (i.e., closed reduction and cast immobilization) for the treatment of fresh, closed fractures in skeletally mature individuals. Candidates for ultrasound treatment are those at high risk for delayed fracture healing or nonunion. These risk factors may include either locations of fractures or patient comorbidities and include the following: Patient comorbidities: Diabetes, Steroid therapy, Osteoporosis, History of alcoholism, History of smoking. Fracture locations: Jones fracture, Fracture of navicular bone in the wrist (also called the scaphoid), Fracture of metatarsal, Fractures associated with extensive soft tissue or vascular damage. Low-intensity ultrasound treatment may be MEDICALLY NECESSARY as a treatment of delayed union of bones, including delayed union** of previously surgically-treated fractures, and excluding the skull and vertebra. 1 Low-intensity ultrasound treatment may be MEDICALLY NECESSARY as a treatment of fracture nonunions of bones, including nonunion*** of previously surgically-treated fractures, and excluding the skull and vertebra. Other applications of low-intensity ultrasound treatment are INVESTIGATIONAL, including, but not limited to, treatment of congenital pseudarthroses, open fractures, fresh* surgically-treated closed fractures, stress fractures, arthrodesis or failed arthrodesis. -

Temporomandibular Joint Dysfunction Corporate Medical Policy Policy
Temporomandibular Joint Dysfunction Corporate Medical Policy File Name: Temporomandibular Joint Dysfunction File Code: UM.SURG.07 Origination: 06/2011 Last Review: 07/2019 Next Review: 07/2020 Effective Date: 10/01/2019 Description/Summary Temporomandibular joint (TMJ) dysfunction refers to a group of disorders characterized by pain in the TMJ and surrounding tissues. Initial conservative therapy is generally recommended; there are also a variety of nonsurgical and surgical treatment possibilities for patients whose symptoms persist. Policy Coding Information Click the links below for attachments, coding tables & instructions. Attachment I - CPT® Code Table & Instructions Attachment II - ICD-10-CM Diagnosis of TMJ When a service may be considered medically necessary • The following diagnostic procedures may be considered medically necessary in the diagnosis of temporomandibular joint (TMJ) dysfunction: - Diagnostic x-ray, tomograms, and arthrograms; - Computed tomography (CT) scan or magnetic resonance imaging (MRI) (in general, CT scans and MRIs are reserved for presurgical evaluations); - Cephalograms (x-rays of jaws and skull); - Pantograms (x-rays of maxilla and mandible). When a service is considered investigational • The following diagnostic procedures are considered investigational in the diagnosis of TMJ dysfunction: - Electromyography (EMG), including surface EMG; Page 1 of 17 Medical Policy Number: UM.SURG.07 - Kinesiography; - Thermography; - Neuromuscular junction testing; - Somatosensory testing; - Transcranial or lateral -

CASE REPORT Injuries Following Segway Personal
UC Irvine Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health Title Injuries Following Segway Personal Transporter Accidents: Case Report and Review of the Literature Permalink https://escholarship.org/uc/item/37r4387d Journal Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 16(5) ISSN 1936-900X Authors Ashurst, John Wagner, Benjamin Publication Date 2015 DOI 10.5811/westjem.2015.7.26549 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California CASE REPORT Injuries Following Segway Personal Transporter Accidents: Case Report and Review of the Literature John Ashurst DO, MSc Conemaugh Memorial Medical Center, Department of Emergency Medicine, Benjamin Wagner, DO Johnstown, Pennsylvania Section Editor: Rick A. McPheeters, DO Submission history: Submitted April 20, 2015; Accepted July 9, 2015 Electronically published October 20, 2015 Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.2015.7.26549 The Segway® self-balancing personal transporter has been used as a means of transport for sightseeing tourists, military, police and emergency medical personnel. Only recently have reports been published about serious injuries that have been sustained while operating this device. This case describes a 67-year-old male who sustained an oblique fracture of the shaft of the femur while using the Segway® for transportation around his community. We also present a review of the literature. [West J Emerg Med. 2015;16(5):693-695.] INTRODUCTION no parasthesia was noted. In 2001, Dean Kamen developed a self-balancing, zero Radiograph of the right femur demonstrated an oblique emissions personal transportation vehicle, known as the fracture of the proximal shaft of the femur with severe Segway® Personal Transporter (PT).1 The Segway’s® top displacement and angulation (Figure). -

Clinical Efficacy of Extended Modified Posteromedial Approach Versus
Clinical ecacy of extended modied posteromedial approach versus posterolateral approach for surgical treatment of posterior pilon fracture: a retrospective analysis Qin-Ming Zhang Aliated Hospital of Jining Medical University Hai-Bin Wang Aliated Hospital of Jining Medical University Xiao-Yan Li Aliated Hospital of Jining Medical University Feng-Long Chu Aliated Hospital of Jining Medical University Liang Han Aliated Hospital of Jining Medical University Dong-Mei Li Aliated Hospital of Jining Medical University Bin Wu ( [email protected] ) Alited Hospital of Jining Medical University https://orcid.org/0000-0003-3707-0056 Research article Keywords: posterior pilon fracture, approach, fracture xation, buttress plate Posted Date: March 30th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-19392/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/12 Abstract Background: Posterior pilon fracture is a type of ankle fracture associated with poorer treatment results compared to the conventional ankle fracture. This is partly related to the lack of consensus on the classication, approach selection, and internal xation method for this type of fracture. This study aimed to investigate the clinical ecacy of posterolateral approach versus extended modied posteromedial approach for surgical treatment of posterior pilon fracture. Methods: Data of 67 patients with posterior pilon fracture who received xation with a buttress plate between January 2015 and December 2018 were retrospectively reviewed. Patients received steel plate xation through either the posterolateral approach (n = 35, group A) or the extended modied posteromedial approach (n = 32, group B). Operation time, intraoperative blood loss, excellent and good rate of reduction, fracture healing time, American Orthopaedic Foot & Ankle Society (AOFAS) Ankle- Hindfoot Scale score, and Visual Analogue Scale score were compared between groups A and B. -

6.3.3 Distal Radius and Wrist
6 Specific fractures 6.3 Forearm and hand 6.3.3 Distal radius and wrist 1 Assessment 657 1.1 Biomechanics 657 1.2 Pathomechanics and classification 657 1.3 Imaging 658 1.4 Associated lesions 659 1.5 Decision making 659 2 Surgical anatomy 660 2.1 Anatomy 660 2.2 Radiographic anatomy 660 2.3 Preoperative planning 661 2.4 Surgical approaches 662 2.4.1 Dorsal approach 2.4.2 Palmar approach 3 Management and surgical treatment 665 3.1 Type A—extraarticular fractures 665 3.2 Type B—partial articular fractures 667 3.3 Type C—complete articular fractures 668 3.4 Ulnar column lesions 672 3.4.1 Ulnar styloid fractures 3.4.2 Ulnar head, neck, and distal shaft fractures 3.5 Postoperative care 674 3.6 Complications 676 3.7 Results 676 4 Bibliography 677 5 Acknowledgment 677 656 PFxM2_Section_6_I.indb 656 9/19/11 2:45:49 PM Authors Daniel A Rikli, Doug A Campbell 6.3.3 Distal radius and wrist of this stable pivot. The TFCC allows independent flexion/ 1 Assessment extension, radial/ulnar deviation, and pronation/supination of the wrist. It therefore plays a crucial role in the stability of 1.1 Biomechanics the carpus and forearm. Significant forces are transmitted across the ulnar column, especially while making a tight fist. The three-column concept (Fig 6.3.3-1) [1] is a helpful bio- mechanical model for understanding the pathomechanics of 1.2 Pathomechanics and classification wrist fractures. The radial column includes the radial styloid and scaphoid fossa, the intermediate column consists of the Virtually all types of distal radial fractures, with the exception lunate fossa and sigmoid notch (distal radioulnar joint, DRUJ), of dorsal rim avulsion fractures, can be produced by hyper- and the ulnar column comprises the distal ulna (DRUJ) with extension forces [2]. -
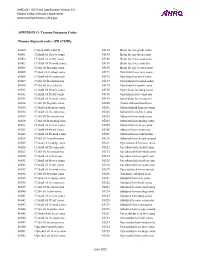
PSI Appendix G Version 6.0 Patient Safety Indicators Appendices
AHRQ QI™ ICD-9-CM Specification Version 6.0 Patient Safety Indicators Appendices www.qualityindicators.ahrq.gov APPENDIX G: Trauma Diagnosis Codes Trauma diagnosis codes: (TRAUMID) 80000 Closed skull vault fx 85184 Brain lac nec-proln coma 80001 Cl skull vlt fx w/o coma 85185 Brain lac nec-deep coma 80002 Cl skull vlt fx-brf coma 85186 Brain lacer nec-coma nos 80003 Cl skull vlt fx-mod coma 85189 Brain lacer nec-concuss 80004 Cl skl vlt fx-proln coma 85190 Brain lac nec w open wnd 80005 Cl skul vlt fx-deep coma 85191 Opn brain lacer w/o coma 80006 Cl skull vlt fx-coma nos 85192 Opn brain lac-brief coma 80009 Cl skl vlt fx-concus nos 85193 Opn brain lacer-mod coma 80010 Cl skl vlt fx/cerebr lac 85194 Opn brain lac-proln coma 80011 Cl skull vlt fx w/o coma 85195 Open brain lac-deep coma 80012 Cl skull vlt fx-brf coma 85196 Opn brain lacer-coma nos 80013 Cl skull vlt fx-mod coma 85199 Open brain lacer-concuss 80014 Cl skl vlt fx-proln coma 85200 Traum subarachnoid hem 80015 Cl skul vlt fx-deep coma 85201 Subarachnoid hem-no coma 80016 Cl skull vlt fx-coma nos 85202 Subarach hem-brief coma 80019 Cl skl vlt fx-concus nos 85203 Subarach hem-mod coma 80020 Cl skl vlt fx/mening hem 85204 Subarach hem-prolng coma 80021 Cl skull vlt fx w/o coma 85205 Subarach hem-deep coma 80022 Cl skull vlt fx-brf coma 85206 Subarach hem-coma nos 80023 Cl skull vlt fx-mod coma 85209 Subarach hem-concussion 80024 Cl skl vlt fx-proln coma 85210 Subarach hem w opn wound 80025 Cl skul vlt fx-deep coma 85211 Opn subarach hem-no coma 80026 Cl skull vlt fx-coma nos 85212 -

Management of Pediatric Forearm Torus Fractures: a Systematic
ORIGINAL ARTICLE Management of Pediatric Forearm Torus Fractures A Systematic Review and Meta-Analysis Nan Jiang, MD,*† Zhen-hua Cao, MD,*‡ Yun-fei Ma, MD,*† Zhen Lin, MD,§ and Bin Yu, MD*† many disadvantages, such as heavy, bulky, and requires a second Objectives: Pediatric forearm torus fracture, a frequent reason for emer- visit to the hospital for removal. These flaws of cast may bring gency department visits, can be immobilized by both rigid cast and non- inconvenience to children as well as their families. In recent years, rigid methods. However, controversy still exists regarding the optimal many pediatric clinicians reported other methods to instead tradi- treatment of the disease. The aim of this study was to compare, in a system- tionally used cast, including soft cast,9,10 Futuro wrist splint,8,11 atic review, clinical efficacy of rigid cast with nonrigid methods for immo- and double Tubigrip.11 Although patients that suffered from fore- bilization of the pediatric forearm torus fractures. arm torus fractures can be immobilized by both rigid cast and non- Methods: Literature search was performed of PubMed and Cochrane Li- rigid materials, controversy still exists in the optimal treatment of brary by 2 independent reviewers to identify randomized controlled trials this fracture. comparing rigid cast with nonrigid methods for pediatric forearm torus The aim of this study was to, in a systematic review and fractures from inception to December 31, 2013, without limitation of publi- meta-analysis, compare clinical efficacy of recently used nonrigid cation language. Trial quality was assessed using the modified Jadad scale. immobilization methods with rigid cast. -

CIHI - Canadian Institute for Health Information CEDIS - the Canadian Emergency Department Information System Committee
CIHI - Canadian Institute for Health Information CEDIS - The Canadian Emergency Department Information System Committee ICIS - Institut canadien d'information sur la santé SIGDUC - le comité des systèmes d'informations de gestion des départements d'urgence canadiens Bernard Unger1, Marc Afilalo1, Jean François Boivin2, Michael Bullard3, Eric Grafstein4, Michael Schull5, Eddy Lang1, Antoinette Colacone1, Nathalie Soucy1, Xiaoqing Xue1, Eli Segal3 1 Emergency Multidisciplinary Research Unit, SMBD-Jewish General Hospital, McGill University, Montreal 2 Centre for Clinical Epidemiology and Community Studies, SMBD-Jewish General Hospital, McGill University, Montreal 3 University of Alberta Hospital, University of Alberta, Edmonton, Alberta 4 St. Paul's Hospital, Vancouver, University of British Columbia, Vancouver, British Columbia 5 Sunnybrook Health Sciences Centre and Institute for Clinical Evaluative Sciences, University of Toronto, Toronto, Ontario with/avec Canadian Institute for Health Information - Classifications & Terminologies and Clinical Administrative Databases (CAD) teams Institut canadien d'information sur la santé - les équipes de classifications & terminologies & des bases de données clinico-administratives (BDCA) Alberta Children's Hospital: Belanger F, Millar K BC Children's Hospital: Clarke M, Colbourne M, Haughton D, Hung G, Whitehouse S Canadian Pediatric Society Cape Breton Regional Hospital: Currie T Children's Hospital of Eastern Ontario: Farion K CH de l'Université de Montréal: Desaulniers P, Boulet M, Charbonneau L, Laurens JP, Jourdenais E CH de l'Université de Québec-Pavillon CHUL: Bernier D, Germain V, Guimont C, Nazair P, Turgeon R Colchester Regional Hospital: Howlett M Credit Valley Hospital, Mississauga: Humniski AM, Letovsky E, Scampoli N CSSS Gatineau: Folot MH, Forest G, Michaud MN, Pham Dinh M, Sibille P Foothills Medical Centre, Calgary: Wertzler B Greater Niagara General Hospital: Turineck D Grey Nuns Comm. -

Treatment of Distal Radius Fractures – Clinical Outcome, Regional Variation and Health Economics
From THE DEPARTMENT OF CLINICAL SCIENCE AND EDUCATION, SÖDERSJUKHUSET Karolinska Institutet, Stockholm, Sweden TREATMENT OF DISTAL RADIUS FRACTURES – CLINICAL OUTCOME, REGIONAL VARIATION AND HEALTH ECONOMICS Jenny Saving Stockholm 2019 All previously published papers were reproduced with permission from the publisher. Published by Karolinska Institutet. Printed by Eprint AB 2019 © Jenny Saving, 2019 ISBN 978-91-7831-339-6 Treatment of distal radius fractures – clinical outcome, regional variation and health economics THESIS FOR DOCTORAL DEGREE (Ph.D.) By Jenny Saving, MD Principal Supervisor: Opponent: MD, Associate Professor Anders Enocson MD, Professor Lars Adolfsson Karolinska Institutet University of Linköping Department of Clinical Science and Education Department of Clinical and Experimental Division of Orthopaedics Medicine Södersjukhuset Examination Board: Co-supervisor(s): MD, Professor Hans Mallmin MD, PhD, Cecilia Mellstrand Navarro Uppsala University Karolinska Institutet Department of Surgical Sciences Department of Clinical Science and Education Section of Orthopaedics Division of Hand Surgery Södersjukhuset MD, Associate Professor Rüdiger Weiss Karolinska Institutet MD, Professor Sari Ponzer Department of Molecular Medicine and Surgery Karolinska Instiutet Karolinska University Hospital Department of Clinical Science and Education Division of Orthopaedics MD, Professor Olof Nilsson Södersjukhuset Uppsala University Department of Surgical Sciences Section of Orthopaedics To my family 3 4 ABSTRACT A distal radius fracture (DRF) remains the most common fracture encountered in health care. DRFs have traditionally been treated with a plaster or surgically with percutaneous methods. Since the end of the 20th century, when internal fixation with a volar locking plate (VLP) was introduced, the incidence of DRF surgery in general and of plating in particular have increased markedly. -

Workcover NSW 2012 Claims Estimation
Minimum Weekly Compensation Estimate for Certain Injuries Extract from Workcover NSW Claims Estimation Manual - Dec 2012 Minimum Bodily Location And Injury Type Estimate GROUP 1: HEAD (includes cranium, eye, ear, mouth, nose and face) Fracture of skull (without brain injury) 6 weeks Fracture of jaw (without dislocation) 6 weeks Fracture-dislocation of jaw 12 weeks Concussion 1 week Serious head injuries (including closed/open head and brain injuries, severe facial Refer to Chapter J injuries involving face, nose and/or ear) Eye Major burn/thermal injury 26 weeks Moderate thermal or chemical burn 6 weeks Foreign body (corneal) and abrasions 2 weeks Foreign body (intraocular) 6 weeks Conjunctivitis/chemical irritation 1 week Contusions/bruising 1 week Retinal detachment 6 weeks Ear Perforated ear drum 2 weeks GROUP 2: NECK Whiplash associated disorder (WAD) without radicular pain 4 weeks Whiplash associated disorder (WAD) with radicular pain 12 weeks Contusion/bruising/sprains 4 weeks Fracture: to vertebral body 12 weeks to spinous or transverse process 6 weeks Fracture – dislocation 26 weeks Fracture with spinal cord injury Refer to Chapter J/Q GROUP 3: TRUNK (includes upper/lower back, chest, abdomen and pelvic region) Acute or recurrent back pain (non-radicular) 4 weeks Radicular back pain 12 weeks Fracture: of vertebral body 12 weeks of transverse or spinous process 6 weeks of sacrum 4 weeks of coccyx 4 weeks Contusion/bruising (upper/lower back) 4 weeks Chest/thorax: Closed rib fracture 4 weeks Fracture with complications (eg: pneumothorax) -

Orthopaedics Instructions: to Best Navigate the List, First Download This PDF File to Your Computer
Orthopaedics Instructions: To best navigate the list, first download this PDF file to your computer. Then navigate the document using the bookmarks feature in the left column. The bookmarks expand and collapse. Finally, ensure that you look at the top of each category and work down to review notes or specific instructions. Bookmarks: Bookmarks: notes or specific with expandable instructions and collapsible topics As you start using the codes, it is recommended that you also check in Index and Tabular lists to ensure there is not a code with more specificity or a different code that may be more appropriate for your patient. Copyright APTA 2016, ALL RIGHTS RESERVED. Last Updated: 09/14/16 Contact: [email protected] Orthopaedics Disorder by site: Ankle Achilles tendinopathy ** Achilles tendinopathy is not listed in ICD10 M76.6 Achilles tendinitis Achilles bursitis M76.61 Achilles tendinitis, right leg M76.62 Achilles tendinitis, left leg ** Tendinosis is not listed in ICD10 M76.89 Other specified enthesopathies of lower limb, excluding foot M76.891 Other specified enthesopathies of right lower limb, excluding foot M76.892 Other specified enthesopathies of left lower limb, excluding foot Posterior tibialis dysfunction **Posterior Tibial Tendon Dysfunction (PTTD) is not listed in ICD10 M76.82 Posterior tibial tendinitis M76.821 Posterior tibial tendinitis, right leg M76.822 Posterior tibial tendinitis, left leg M76.89 Other specified enthesopathies of lower limb, excluding foot M76.891 Other specified enthesopathies of right lower limb, -

Vanderbilt Sports Medicine
Alabama AAP Fall Meeting Sept.19-20, 2009 Pediatric Fracture Care for the Pediatrician Andrew Gregory, MD, FAAP, FACSM Assistant Professor Orthopedics & Pediatrics Program Director, Sports Medicine Fellowship Vanderbilt University Vanderbilt Sports Medicine Disclosure No conflict of interest - unfortunately for me, I have no financial relationships with companies making products regarding this topic to disclose Objectives Review briefly the differences of pediatric bone Review Pediatric Fracture Classification Discuss subtle fractures in kids Discuss a few other pediatric only conditions 1 Pediatric Skeleton Bone is relatively elastic and rubbery Periosteum is quite thick & active Ligaments are strong relative to the bone Presence of the physis - “weak link” Ligament injuries & dislocations are rare – “kids don’t sprain stuff” Fractures heal quickly and have the capacity to remodel Anatomy of Pediatric Bone Epiphysis Physis Metaphysis Diaphysis Apophysis Pediatric Fracture Classification Plastic Deformation – Bowing usually of fibula or ulna Buckle/ Torus – compression, stable Greenstick – unicortical tension Complete – Spiral, Oblique, Transverse Physeal – Salter-Harris Apophyseal avulsion 2 Plastic deformation Bowing without fracture Often deformed requiring reduction Buckle (Torus) Fracture Buckled Periosteum – Metaphyseal/ diaphyseal junction Greenstick Fracture Cortex Broken on Only One Side – Incomplete 3 Complete Fractures Transverse – Perpendicular to the bone Oblique – Across the bone at 45-60 o – Unstable Spiral – Rotational