Strongly Heterogeneous Transmission of COVID–19 in Mainland China: Local and Regional Variation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Greater Bay Area Logistics Markets and Opportunities Colliers Radar Logistics | Industrial Services | South China | 29 May 2020
COLLIERS RADAR LOGISTICS | INDUSTRIAL SERVICES | SOUTH CHINA | 29 MAY 2020 Rosanna Tang Head of Research | Hong Kong SAR and Southern China +852 2822 0514 [email protected] Jay Zhong Senior Analyst | Research | Guangzhou +86 20 3819 3851 [email protected] Yifan Yu Assistant Manager | Research | Shenzhen +86 755 8825 8668 [email protected] Justin Yi Senior Analyst | Research | Shenzhen +86 755 8825 8600 [email protected] GREATER BAY AREA LOGISTICS MARKETS AND OPPORTUNITIES COLLIERS RADAR LOGISTICS | INDUSTRIAL SERVICES | SOUTH CHINA | 29 MAY 2020 TABLE OF CONTENTS Page INSIGHTS AND RECOMMENDATIONS 3 MAP OF GBA LOGISTICS MARKETS AND RECOMMENDED CITIES 4 MAP OF GBA TRANSPORTATION SYSTEM 5 LOGISTICS INDUSTRY SUPPLY AND DEMAND 6 NEW GROWTH POTENTIAL AREA IN GBA LOGISTICS 7 GBA LOGISTICS CLUSTER – ZHUHAI-ZHONGSHAN-JIANGMEN 8 GBA LOGISTICS CLUSTER – SHENZHEN-DONGGUAN-HUIZHOU 10 GBA LOGISTICS CLUSTER – GUANGZHOU-FOSHAN-ZHAOQING 12 2 COLLIERS RADAR LOGISTICS | INDUSTRIAL SERVICES | SOUTH CHINA | 29 MAY 2020 Insights & Recommendations RECOMMENDED CITIES This report identifies three logistics Zhuhai Zhongshan Jiangmen clusters from the mainland Greater Bay The Hong Kong-Zhuhai-Macau We expect Zhongshan will be The manufacturing sector is Area (GBA)* cities and among these Bridge Zhuhai strengthens the a logistics hub with the now the largest contributor clusters highlights five recommended marine and logistics completion of the Shenzhen- to Jiangmen’s overall GDP. logistics cities for occupiers and investors. integration with Hong Kong Zhongshan Bridge, planned The government aims to build the city into a coastal logistics Zhuhai-Zhongshan-Jiangmen: and Macau. for 2024, connecting the east and west banks of the Peral center and West Guangdong’s > Zhuhai-Zhongshan-Jiangmen’s existing River. -

Appendix 1: Rank of China's 338 Prefecture-Level Cities
Appendix 1: Rank of China’s 338 Prefecture-Level Cities © The Author(s) 2018 149 Y. Zheng, K. Deng, State Failure and Distorted Urbanisation in Post-Mao’s China, 1993–2012, Palgrave Studies in Economic History, https://doi.org/10.1007/978-3-319-92168-6 150 First-tier cities (4) Beijing Shanghai Guangzhou Shenzhen First-tier cities-to-be (15) Chengdu Hangzhou Wuhan Nanjing Chongqing Tianjin Suzhou苏州 Appendix Rank 1: of China’s 338 Prefecture-Level Cities Xi’an Changsha Shenyang Qingdao Zhengzhou Dalian Dongguan Ningbo Second-tier cities (30) Xiamen Fuzhou福州 Wuxi Hefei Kunming Harbin Jinan Foshan Changchun Wenzhou Shijiazhuang Nanning Changzhou Quanzhou Nanchang Guiyang Taiyuan Jinhua Zhuhai Huizhou Xuzhou Yantai Jiaxing Nantong Urumqi Shaoxing Zhongshan Taizhou Lanzhou Haikou Third-tier cities (70) Weifang Baoding Zhenjiang Yangzhou Guilin Tangshan Sanya Huhehot Langfang Luoyang Weihai Yangcheng Linyi Jiangmen Taizhou Zhangzhou Handan Jining Wuhu Zibo Yinchuan Liuzhou Mianyang Zhanjiang Anshan Huzhou Shantou Nanping Ganzhou Daqing Yichang Baotou Xianyang Qinhuangdao Lianyungang Zhuzhou Putian Jilin Huai’an Zhaoqing Ningde Hengyang Dandong Lijiang Jieyang Sanming Zhoushan Xiaogan Qiqihar Jiujiang Longyan Cangzhou Fushun Xiangyang Shangrao Yingkou Bengbu Lishui Yueyang Qingyuan Jingzhou Taian Quzhou Panjin Dongying Nanyang Ma’anshan Nanchong Xining Yanbian prefecture Fourth-tier cities (90) Leshan Xiangtan Zunyi Suqian Xinxiang Xinyang Chuzhou Jinzhou Chaozhou Huanggang Kaifeng Deyang Dezhou Meizhou Ordos Xingtai Maoming Jingdezhen Shaoguan -
Hong Kong SAR
China Data Supplement November 2006 J People’s Republic of China J Hong Kong SAR J Macau SAR J Taiwan ISSN 0943-7533 China aktuell Data Supplement – PRC, Hong Kong SAR, Macau SAR, Taiwan 1 Contents The Main National Leadership of the PRC 2 LIU Jen-Kai The Main Provincial Leadership of the PRC 30 LIU Jen-Kai Data on Changes in PRC Main Leadership 37 LIU Jen-Kai PRC Agreements with Foreign Countries 47 LIU Jen-Kai PRC Laws and Regulations 50 LIU Jen-Kai Hong Kong SAR 54 Political, Social and Economic Data LIU Jen-Kai Macau SAR 61 Political, Social and Economic Data LIU Jen-Kai Taiwan 65 Political, Social and Economic Data LIU Jen-Kai ISSN 0943-7533 All information given here is derived from generally accessible sources. Publisher/Distributor: GIGA Institute of Asian Affairs Rothenbaumchaussee 32 20148 Hamburg Germany Phone: +49 (0 40) 42 88 74-0 Fax: +49 (040) 4107945 2 November 2006 The Main National Leadership of the PRC LIU Jen-Kai Abbreviations and Explanatory Notes CCP CC Chinese Communist Party Central Committee CCa Central Committee, alternate member CCm Central Committee, member CCSm Central Committee Secretariat, member PBa Politburo, alternate member PBm Politburo, member Cdr. Commander Chp. Chairperson CPPCC Chinese People’s Political Consultative Conference CYL Communist Youth League Dep. P.C. Deputy Political Commissar Dir. Director exec. executive f female Gen.Man. General Manager Gen.Sec. General Secretary Hon.Chp. Honorary Chairperson H.V.-Chp. Honorary Vice-Chairperson MPC Municipal People’s Congress NPC National People’s Congress PCC Political Consultative Conference PLA People’s Liberation Army Pol.Com. -
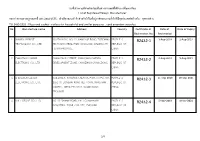
No. Manufacture Name Address Country Certificate of Registration
รายชื่อโรงงานทที่ าผลิตภัณฑ์ในตา่ งประเทศทไี่ ดร้ ับการขึ้นทะเบียน List of Registered Foreign Manufacturer ขอบขา่ ยตามมาตรฐานเลขท ี่ มอก.2432-2555 : เตา้ เสียบและเตา้ รับส าหรับใชใ้ นทอี่ ยู่อาศัยและงานทวั่ ไปทมี่ จี ุดประสงค์คล้ายกัน : ชดุ สายพ่วง TIS 2432-2555 : Plugs and socket - outlets for household and similar purposes : cord extention setsrules No. Manufacture name Address Country Certificate of Date of Date of Expiry Registration No. Registration 1 XIAMEN SEEBEST SOUTH BLDG, NO. 31 XIANGYUE ROAD, TORCH HI- PEOPLE' S R2432-1 3-Aug-2018 2-Aug-2021 TECHNOLOGY CO., LTD. TECH INDUSTRIAL PARK (XIANG'AN), XIAMEN CITY, REPUBLIC OF FUJIAN PROVINCE CHINA 2 CHAOZHOU NANKE CHANGCHUN STREET, XIANGQIAO GARDEN PEOPLE' S R2432-2 6-Aug-2018 5-Aug-2021 ELECTRONIC CO., LTD. DEVELOPMENT ZONE, CHAOZHOU GUANGDONG REPUBLIC OF CHINA 3 SHENZHEN CLEVER BUILDING 8, BAIWANG CREATIVE PARK (UTPC), NO. PEOPLE' S R2432-3 11-Sep-2018 10-Sep-2021 ELECTRONIC CO., LTD. 1051 OF SONGBAI ROAD XILI TOWN, NANSHAN REPUBLIC OF DISTRICT, SHENZHEN CITY, GUANGDONG CHINA PROVINCE 4 BULL GROUP CO., LTD. NO. 32 SHAHAI ROAD, EAST GUANHAIWEI PEOPLE' S R2432-4 5-Nov-2018 4-Nov-2021 INDUSTRIAL ZONE, CIXI CITY, ZHEJIANG REPUBLIC OF CHINA 1/4 รายชื่อโรงงานทที่ าผลิตภัณฑ์ในตา่ งประเทศทไี่ ดร้ ับการขึ้นทะเบียน List of Registered Foreign Manufacturer ขอบขา่ ยตามมาตรฐานเลขท ี่ มอก.2432-2555 : เตา้ เสียบและเตา้ รับส าหรับใชใ้ นทอี่ ยู่อาศัยและงานทวั่ ไปทมี่ จี ุดประสงค์คล้ายกัน : ชดุ สายพ่วง TIS 2432-2555 : Plugs and socket - outlets for household and similar purposes : cord extention setsrules No. Manufacture name Address Country Certificate of Date of Date of Expiry Registration No. Registration 5 DONGGUAN GWTEE ELECTRIC GETIAN INDUSTRIAL ZONE, CHAOLANG VILLAGE, PEOPLE' S R2432-5 16-Nov-2018 15-Nov-2021 MANUFACTURE CO., LTD. -

Spatiotemporal Patterns of Population Mobility and Its Determinants in Chinese Cities Based on Travel Big Data
sustainability Article Spatiotemporal Patterns of Population Mobility and Its Determinants in Chinese Cities Based on Travel Big Data Zhen Yang 1,2 , Weijun Gao 1,2,* , Xueyuan Zhao 1,2, Chibiao Hao 3 and Xudong Xie 3 1 Innovation Institute for Sustainable Maritime Architecture Research and Technology, Qingdao University of Technology, Qingdao 266033, China; [email protected] (Z.Y.); [email protected] (X.Z.) 2 Faculty of Environmental Engineering, The University of Kitakyushu, Kitakyushu 808-0135, Japan 3 College of Architecture and Urban Planning, Qingdao University of Technology, Qingdao 266033, China; [email protected] (C.H.); [email protected] (X.X.) * Correspondence: [email protected]; Tel.: +81-93-695-3234 Received: 16 April 2020; Accepted: 13 May 2020; Published: 14 May 2020 Abstract: Large-scale population mobility has an important impact on the spatial layout of China’s urban systems. Compared with traditional census data, mobile-phone-based travel big data can describe the mobility patterns of a population in a timely, dynamic, complete, and accurate manner. With the travel big dataset supported by Tencent’s location big data, combined with social network analysis (SNA) and a semiparametric geographically weighted regression (SGWR) model, this paper first analyzed the spatiotemporal patterns and characteristics of mobile-data-based population mobility (MBPM), and then revealed the socioeconomic factors related to population mobility during the Spring Festival of 2019, which is the most important festival in China, equivalent to Thanksgiving Day in United States. During this period, the volume of population mobility exceeded 200 million, which became the largest time node of short-term population mobility in the world. -

Epidemiologic Clues to SARS Origin in China Rui-Heng Xu,* Jian-Feng He,* Meirion R
RESEARCH Epidemiologic Clues to SARS Origin in China Rui-Heng Xu,* Jian-Feng He,* Meirion R. Evans,†‡ Guo-Wen Peng,* Hume E Field,§ De-Wen Yu,* Chin-Kei Lee,¶ Hui-Min Luo,* Wei-Sheng Lin,* Peng Lin,* Ling-Hui Li,* Wen-Jia Liang,* Jin-Yan Lin,* and Alan Schnur#1 An epidemic of severe acute respiratory syndrome ipalities (Foshan, Jiangmen, Zhongshan, Guangzhou, (SARS) began in Foshan municipality, Guangdong Shenzhen, Zhaoqing) from November 2002 to mid- Province, China, in November 2002. We studied SARS January 2003. On February 3, 2003, province-wide case reports through April 30, 2003, including data from mandatory case reporting of atypical pneumonia that used case investigations and a case series analysis of index a standard case definition and reporting form was institut- cases. A total of 1,454 clinically confirmed cases (and 55 deaths) occurred; the epidemic peak was in the first week ed. The provincial health department also introduced a of February 2003. Healthcare workers accounted for 24% range of public health control measures, including guide- of cases. Clinical signs and symptoms differed between lines on epidemiologic investigation of cases and contacts children (<18 years) and older persons (>65 years). (February 3) and on hospital admission, clinical manage- Several observations support the hypothesis of a wild ani- ment, and infection control arrangements for patients mal origin for SARS. Cases apparently occurred independ- (February 9). Subsequently, the department issued guide- ently in at least five different municipalities; -

Analysis of CO2 Emission in Guangdong Province, China
Feasibility Study of CCUS-Readiness in Guangdong Province, China (GDCCSR) Final Report: Part 1 Analysis of CO2 Emission in Guangdong Province, China GDCCSR-GIEC Team March 2013 Authors (GDCCSR-GIEC Team) Daiqing Zhao Cuiping Liao Ying Huang, Hongxu Guo Li Li, Weigang Liu (Guangzhou Institute of Energy Conversion, Chinese Academy of Sciences, Guangzhou, China) For comments or queries please contact: Prof. Cuiping Liao [email protected] Announcement This is the first part of the final report of the project “Feasibility Study of CCS-Readiness in Guangdong (GDCCSR)”, which is funded by the Strategic Programme Fund of the UK Foreign & Commonwealth Office joint with the Global CCS Institute. The report is written based on published data mainly. The views in this report are the opinions of the authors and do not necessarily reflect those of the Guangzhou Institute of Energy Conversion, nor of the funding organizations. The complete list of the project reports are as follows: Part 1 Analysis of CO2 emission in Guangdong Province, China. Part 2 Assessment of CO2 Storage Potential for Guangdong Province, China. Part 3 CO2 Mitigation Potential and Cost Analysis of CCS in Power Sector in Guangdong Province, China. Part 4 Techno-economic and Commercial Opportunities for CCS-Ready Plants in Guangdong Province, China. Part 5 CCUS Capacity Building and Public Awareness in Guangdong Province, China Part 6 CCUS Development Roadmap Study for Guangdong Province, China Analysis of CO2 Emission in Guangdong Province Contents Background for the Report .........................................................................................2 -

Exploring Coordinative Mechanisms for Environmental Governance in Guangdong-Hong Kong-Macao Greater Bay Area: an Ecology of Games Framework
sustainability Article Exploring Coordinative Mechanisms for Environmental Governance in Guangdong-Hong Kong-Macao Greater Bay Area: An Ecology of Games Framework Wenjie Zhou and Rui Mu * Faculty of Humanities and Social Sciences, Dalian University of Technology, Dalian 116024, China; [email protected] * Correspondence: [email protected]; Tel.: +86-0411-8470-7479 Received: 15 May 2019; Accepted: 30 May 2019; Published: 3 June 2019 Abstract: To solve regional environmental problems, there is a trend of establishing urban agglomerations and formulating cooperative policy institutions in China. The extant studies on policy institutions largely focus on the coordinative mechanisms of multiple actors within one single institution. Only a few studies have tried to understand how different policy institutions are interlinked and mutually affected to influence actors’ decisions and problem resolutions. This article applies a network-based analytical approach and adopts the Ecology of Games Framework to explore how regional environmental governance is coordinated in the Guangdong-Hong Kong-Macao Greater Bay Area. It was found that coordinative mechanisms in regional environmental governance can happen around three elements: policy institutions, policy actors, and policy issues. Policy institutions tend to serve as an umbrella for many diverse and interdependent activities and actors within individual institutions. Additionally, positive externalities emerging between different policy institutions perform as coordinators across institutions. For actors, state-level actors usually play as facilitators of policy institutions while they are not active in participating in policy games in later phases; it is regional actors, particularly from Guangdong, that are active in the operation of policy institutions. For policy issues, they emerge because they are often tied with each other, and some of them play as the common ground for seemly separating policy institutions. -

Complicated HCV Subtype Expansion Among Drug Users in Guangdong
Infection, Genetics and Evolution 73 (2019) 139–145 Contents lists available at ScienceDirect Infection, Genetics and Evolution journal homepage: www.elsevier.com/locate/meegid Research paper Complicated HCV subtype expansion among drug users in Guangdong province, China T ⁎ Jin Yana, , Xiao-Bing Fua, Ping-Ping Zhoub, Xiang Heb, Jun Liua, Xu-He Huangb, Guo-Long Yua, Xin-Ge Yana, Jian-Rong Lia, Yan Lia, Peng Lina a Guangdong Provincial Center for Disease Control and Prevention, 160 Qunxian Road, Panyu District, Guangzhou 511430, Guangdong, China b Guangdong Provincial Institute of Public Health, Guangdong Provincial Center for Disease Control and Prevention, 160 Qunxian Road, Panyu District, Guangzhou 511430, Guangdong, China ARTICLE INFO ABSTRACT Keywords: Guangdong Province is one of the most developed and populous provinces in southern China. The subtype HCV situation of hepatitis C virus (HCV) in Guangdong remains unknown. The aim of this study was to investigate Subtype and estimate the HCV subtypes in drug users (DU) using a city-based sampling strategy to better understand the Drug users characteristics of HCV transmission in Guangdong. Archived plasma samples (n = 1074) from DU who were Molecular epidemiology anti-HCV positive in 2014 were selected randomly from 20 cities in Guangdong Province. Subtypes were de- Guangdong termined based on core and/or E1 sequences using phylogenetic analysis. The distributions of HCV subtypes in DU and different regions were analyzed. A total of 8 genotypes were identified. The three main HCV subtypes in DU in Guangdong were 6a (63.0%), 3a (15.2%), and 3b (11.8%). Significant differences were discovered among different registered residency and regions but not among genders, marital status, education level, or drug use patterns. -

Women's Development in Guangdong; Unequal Opportunities and Limited Development in a Market Economy
City University of New York (CUNY) CUNY Academic Works Dissertations and Theses City College of New York 2012 Women's Development in Guangdong; Unequal Opportunities and Limited Development in a Market Economy Ying Hua Yue CUNY City College How does access to this work benefit ou?y Let us know! More information about this work at: https://academicworks.cuny.edu/cc_etds_theses/169 Discover additional works at: https://academicworks.cuny.edu This work is made publicly available by the City University of New York (CUNY). Contact: [email protected] Running head: WOMEN’S DEVELOPMENT IN GUANGDONG 1 Women’s Development in Guangdong: Unequal Opportunities and Limited Development in a Market Economy Yinghua Yue The City College of New York In Partial Fulfillment of the Requirements for the Degree of Master of Arts in Sociology Fall 2012 WOMEN’ S DEVELOPMENT IN GUANGDONG 2 ABSTRACT In the context of China’s three-decade market-oriented economic reform, in which economic development has long been prioritized, women’s development, as one of the social undertakings peripheral to economic development, has relatively lagged behind. This research is an attempt to unfold the current situation of women’s development within such context by studying the case of Guangdong -- the province as forerunner of China’s economic reform and opening-up -- drawing on current primary resources. First, this study reveals mixed results for women’s development in Guangdong: achievements have been made in education, employment and political participation in terms of “rates” and “numbers,” and small “breakthroughs” have taken place in legislation and women’s awareness of their equal rights and interests; however, limitations and challenges, like disparities between different women groups in addition to gender disparity, continue to exist. -

11Th International Conference on Chaozhou Studies
11TH INTERNATIONAL CONFERENCE ON CHAOZHOU STUDIES AUGUST 17 – 19, 2015 UNIVERSITY OF VICTORIA VICTORIA, BRITISH COLUMBIA, CANADA PHOTO BY UVIC PHOTO SERVICES UVIC PHOTO BY PHOTO 八 潮 第十 N IO T 年 N E V T H N E O 1 C 8 L t h A T N E O I O T C A H N E R W E T N I 11TH INTERNATIONAL CONFERENCE ON CHAOZHOU STUDIES A 痦⼧♧㾉惐㷖㕂꣢灇雭⠔11TH INTERNATIONAL CONFERENCE ON CHAOZHOU STUDIES Revised Program & Itinerary Revised Program & Itinerary Due to the absence of a number of scheduled present- Due to the absence of a number of scheduled present- ers, we have had to make changes to the conference ers, we have had to make changes to the conference program. Please see the revised schedule & itinerary for program. Please see the revised schedule & itinerary for updated times and locations. updated times and locations. HUANG Ting will not be able to present the keynote HUANG Ting will not be able to present the keynote speech during the Opening Plenary. Instead, we will speech during the Opening Plenary. Instead, we will hear from ZHOU Shaochan. A short biography is hear from ZHOU Shaochan. A short biography is included below. included below. The following sessions have been combined and will be The following sessions have been combined and will be at 11:30 am on Tuesday: at 11:30 am on Tuesday: • Religion and Characters will be in Fraser 157 • Religion and Characters will be in Fraser 157 • Dialect #1 and Dialect #2 will be in Fraser 158 • Dialect #1 and Dialect #2 will be in Fraser 158 Professor ZHOU Shaochuan, PhD in History ワ㼱䊛侅䱇⾎〷㷖⽇㡦 Professor ZHOU Shaochuan is from Shantou, Guangdong Province in China, ワ㼱䊛⽇㡦勻荈䎛⚎寀㣢梡⟣ currently a professor and doctoral tutor at School of Chinese Ancient Books ⻌❩䋗薴㣐㷖〢硂♸⠛絡俒⻊灇 and Traditional Culture, Beijing Normal University. -

Guangdong Province, 2019
China CDC Weekly Preplanned Studies Co-Administration of Multiple Childhood Vaccines — Guangdong Province, 2019 Hai Li1,2; Yanqiu Tan1,3; Haiying Zeng1,3; Fengmei Zeng1,4; Xing Xu1,5; Yu Liao1,6; Qi Zhu6; Meng Zhang1,6; Xuguang Chen1,6; Min Kang1,6; Fujie Xu7; Huizhen Zheng1,6,# This policy could save about 1137.62 RMB for each Summary child during their first 2 years of life. To provide scope, What is already known about this topic? 1.8 million infants in Guangdong received the first The Co-Administration of Multiple Vaccines were dose of Hepatitis B vaccine in 2018; based on the implemented in many countries and have been shown number of children, this policy could therefore save up to significantly reduce many times of visiting the to 2.0 billion RMB for families in Guangdong vaccination clinic. Province for this single vaccination event. The Co- What is added by this report? Administration of Multiple Vaccines Policy can It is the first time to calculate the cost of visiting significantly reduce vaccination costs for children’s vaccination clinic from transportation and work- families and can greatly improve the social cost- effectiveness of childhood vaccinations. Our findings absence for children’s families in Guangdong. suggest that Co-Administration of Multiple Vaccines What are the implications for public health should be implemented as soon as possible. practice? This study estimated the cost incurred by the We demonstrated the importance of Co- families with children under 2 years old in Guangdong Administration of Multiple Vaccines that reduce the Province during the process of inoculation.