Computational Pharmacogenomics Screen Identifies Synergistic Statin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Illuminating Dna Packaging in Sperm Chromatin: How Polycation Lengths, Underprotamination and Disulfide Linkages Alters Dna Condensation and Stability
University of Kentucky UKnowledge Theses and Dissertations--Chemistry Chemistry 2019 ILLUMINATING DNA PACKAGING IN SPERM CHROMATIN: HOW POLYCATION LENGTHS, UNDERPROTAMINATION AND DISULFIDE LINKAGES ALTERS DNA CONDENSATION AND STABILITY Daniel Kirchhoff University of Kentucky, [email protected] Digital Object Identifier: https://doi.org/10.13023/etd.2019.233 Right click to open a feedback form in a new tab to let us know how this document benefits ou.y Recommended Citation Kirchhoff, Daniel, "ILLUMINATING DNA PACKAGING IN SPERM CHROMATIN: HOW POLYCATION LENGTHS, UNDERPROTAMINATION AND DISULFIDE LINKAGES ALTERS DNA CONDENSATION AND STABILITY" (2019). Theses and Dissertations--Chemistry. 112. https://uknowledge.uky.edu/chemistry_etds/112 This Doctoral Dissertation is brought to you for free and open access by the Chemistry at UKnowledge. It has been accepted for inclusion in Theses and Dissertations--Chemistry by an authorized administrator of UKnowledge. For more information, please contact [email protected]. STUDENT AGREEMENT: I represent that my thesis or dissertation and abstract are my original work. Proper attribution has been given to all outside sources. I understand that I am solely responsible for obtaining any needed copyright permissions. I have obtained needed written permission statement(s) from the owner(s) of each third-party copyrighted matter to be included in my work, allowing electronic distribution (if such use is not permitted by the fair use doctrine) which will be submitted to UKnowledge as Additional File. I hereby grant to The University of Kentucky and its agents the irrevocable, non-exclusive, and royalty-free license to archive and make accessible my work in whole or in part in all forms of media, now or hereafter known. -

Aloe Ferox 117 Table 9: Phytochemical Constituents of Different Extracts of Aloe CIM- Sheetal Leaves 119
International Journal of Scientific & Engineering Research ISSN 2229-5518 1 Morphological, in vitro, Biochemical and Genetic Diversity Studies in Aloe species THESIS SUBMITTED TO OSMANIA UNIVERSITY FOR THE AWARD OF DOCTOR OF PHILOSOPHY IN GENETICS IJSER By B. CHANDRA SEKHAR SINGH DEPARTMENT OF GENETICS OSMANIA UNIVERSITY HYDERABAD - 500007, INDIA JULY, 2015 IJSER © 2018 http://www.ijser.org International Journal of Scientific & Engineering Research ISSN 2229-5518 2 DECLARATION The investigation incorporated in the thesis entitled “Morphological, in vitro, Biochemical and Genetic Diversity Studies in Aloe species’’ was carried out by me at the Department of Genetics, Osmania University, Hyderabad, India under the supervision of Prof. Anupalli Roja Rani, Osmania University, Hyderabad, India. I hereby declare that the work is original and no part of the thesis has been submitted for the award of any other degree or diploma prior to this date. IJSER Date: (Bhaludra Chandra Sekhar Singh) IJSER © 2018 http://www.ijser.org International Journal of Scientific & Engineering Research ISSN 2229-5518 3 DEDICATION I dedicateIJSER this work to my beloved and beautiful wife B. Ananda Sekhar IJSER © 2018 http://www.ijser.org International Journal of Scientific & Engineering Research ISSN 2229-5518 4 Acknowledgements This dissertation is an outcome of direct and indirect contribution of many people, which supplemented my own humble efforts. I like this opportunity to mention specifically some of them and extend my gratefulness to other well wisher, known and unknown. I feel extremely privileged to express my veneration for my superviosor Dr. Anupalli Roja Rani, Professor and Head, Department of Genetics, Osmania University, Hyderabad. Her whole- hearted co-operation, inspiration and encouragement rendered throughout made this in carrying out the research and writing of this thesis possible. -

Investigation and Engineering of Polyketide Biosynthetic Pathways
Utah State University DigitalCommons@USU All Graduate Theses and Dissertations Graduate Studies 12-2017 Investigation and Engineering of Polyketide Biosynthetic Pathways Lei Sun Utah State University Follow this and additional works at: https://digitalcommons.usu.edu/etd Part of the Biological Engineering Commons Recommended Citation Sun, Lei, "Investigation and Engineering of Polyketide Biosynthetic Pathways" (2017). All Graduate Theses and Dissertations. 6903. https://digitalcommons.usu.edu/etd/6903 This Dissertation is brought to you for free and open access by the Graduate Studies at DigitalCommons@USU. It has been accepted for inclusion in All Graduate Theses and Dissertations by an authorized administrator of DigitalCommons@USU. For more information, please contact [email protected]. INVESTIGATION AND ENGINEERING OF POLYKETIDE BIOSYNTHETIC PATHWAYS by Lei Sun A dissertation submitted in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSPHY in Biological Engineering Approved: ______________________ ____________________ Jixun Zhan, Ph.D. David W. Britt, Ph.D. Major Professor Committee Member ______________________ ____________________ Dong Chen, Ph.D. Jon Takemoto, Ph.D. Committee Member Committee Member ______________________ ____________________ Elizabeth Vargis, Ph.D. Mark R. McLellan, Ph.D. Committee Member Vice President for Research and Dean of the School of Graduate Studies UTAH STATE UNIVERSITY Logan, Utah 2017 ii Copyright© Lei Sun 2017 All Rights Reserved iii ABSTRACT Investigation and engineering of polyketide biosynthetic pathways by Lei Sun, Doctor of Philosophy Utah State University, 2017 Major Professor: Jixun Zhan Department: Biological Engineering Polyketides are a large family of natural products widely found in bacteria, fungi and plants, which include many clinically important drugs such as tetracycline, chromomycin, spirolaxine, endocrocin and emodin. -

WO 2016/123419 Al 4 August 2016 (04.08.2016) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization I International Bureau (10) International Publication Number (43) International Publication Date WO 2016/123419 Al 4 August 2016 (04.08.2016) P O P C T (51) International Patent Classification: AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, C12Q 1/68 (2006.01) C07H 21/02 (2006.01) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (21) International Application Number: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, PCT/US2016/015503 KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, (22) International Filing Date: MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, 29 January 2016 (29.01 .2016) PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, (25) Filing Language: English TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (26) Publication Language: English (84) Designated States (unless otherwise indicated, for every (30) Priority Data: kind of regional protection available): ARIPO (BW, GH, 62/1 10,050 30 January 2015 (30.01.2015) US GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, (71) Applicant: PRESIDENT AND FELLOWS OF HAR¬ TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, VARD COLLEGE [US/US]; 17 Quincy Street, Cam DK, EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, bridge, MA 02138 (US). -

A Review of the Different Staining Techniques for Human Metaphase Chromosomes
Department of Chemistry University College London University of London A Review of the Different Staining Techniques for Human Metaphase Chromosomes Ana Katrina C. Estandarte Submitted in partial fulfillment of the requirements for the degree of Masters in Research !at the University of London February 24, 2012 Abstract This review investigates the different staining techniques for human metaphase chromosomes. The higher order organization of chromosomes still remains unclear today. There are various imaging techniques that can be used to study chromosomes. Staining increases the contrast of chromosomes under these different imaging techniques while banding allows the identification of chromosomes and the abnormalities present in it, and provides information about the chromosomal substructures. The different stains that can be used for studying human metaphase chromosomes with light, fluorescence and electron microscopy, and coherent x-ray diffraction imaging are discussed. By understanding the underlying mechanism of staining and banding, an insight on the relation of the chromosomal bands with the chromosomal substructures is provided. Moreover, through this review, an understanding of how the structure of the stain affects its mode of binding to the chromosomes and how this mode of binding, in turn, affects the mechanism of band formation are achieved. The information obtained from this review can then be used to develop a suitable stain for studying the structure of human metaphase chromosomes with different imaging techniques. Copyright -

Application of Fluorescent Staining of Chromosomes to Genetic Studies in Citrus
Japanese Journal of Plant Science ©2007 Global Science Books Application of Fluorescent Staining of Chromosomes to Genetic Studies in Citrus Masashi Yamamoto Faculty of Agriculture, Kagoshima University, Korimoto, Kagoshima 890-0065, Japan Correspondence : [email protected] ABSTRACT The application of staining with the guanine-cytosine specific fluorochrome chromomycin A3 (CMA) of citrus chromosomes to genetic studies is reviewed. When CMA staining is performed, the existence of characteristic CMA banding patterns with high levels of diversity and heterozygosity in citrus chromosomes is demonstrated. Similar CMA banding patterns have been observed in related species. Thus, CMA banding patterns of chromosomes have been considered to provide very important information for phylogenic studies in citrus. Chromosomal identification of citrus has also progressed rapidly by means of the CMA banding method. Chromosomes exhibiting the same CMA banding pattern were separated and classified using the relative sizes of fluorescent bands as indices. All nine chromosomes of haploid citrus were identified by this method. Analysis of the chromosomal configuration of parental materials and their progeny was efficient for genetic improvement in citrus. Characteristic chromosomes could be used as a marker for the parent-progeny relationship since these chromosomes are transmitted from the parents. In particular, CMA chromosome staining is a very powerful tool for ploidy manipulation. The advantage of using CMA staining is that the entire chromosomal -

Downloaded and Curated
bioRxiv preprint doi: https://doi.org/10.1101/2021.02.25.432909; this version posted February 26, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Description and analysis of glycosidic residues in the largest open natural products database Authors: Jonas Schaub; Institute for Inorganic and Analytical Chemistry; Friedrich-Schiller University, Lessing Strasse 8, 07743, Jena, Germany; [email protected]; ORCID: 0000-0003-1554-6666 Achim Zielesny; Institute for Bioinformatics and Chemoinformatics, Westphalian University of Applied Sciences, August-Schmidt-Ring 10, 45665, Recklinghausen, Germany; [email protected]; ORCID: 0000-0003-0722-4229 Christoph Steinbeck*; Institute for Inorganic and Analytical Chemistry; Friedrich-Schiller University, Lessing Strasse 8, 07743, Jena, Germany; [email protected]; ORCID: 0000-0001-6966-0814 Maria Sorokina*; Institute for Inorganic and Analytical Chemistry; Friedrich-Schiller University, Lessing Strasse 8, 07743, Jena, Germany; [email protected]; ORCID: 0000-0001-9359-7149 Corresponding author emails: [email protected], [email protected] Abstract: Natural products (NP), biomolecules produced by living organisms, inspire the pharmaceutical industry and research due to their structural characteristics and the substituents from which they derive their activities. Glycosidic residues are frequently present in NP structures and have particular pharmacokinetic and pharmacodynamic importance as they improve their solubility and are often involved in molecular transport, target specificity, ligand-target interactions and receptor binding. The COlleCtion of Open Natural prodUcTs (COCONUT) is currently the largest open database of NP and therefore a suitable starting point for the detection and analysis of the diversity of glycosidic residues in NP. -

WO 2016/138496 Al 1 September 2016 (01.09.2016) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/138496 Al 1 September 2016 (01.09.2016) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C12Q 1/68 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/US20 16/0 19962 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 26 February 2016 (26.02.2016) KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, (25) Filing Language: English PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, (26) Publication Language: English SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 62/126,230 27 February 2015 (27.02.2015) US (84) Designated States (unless otherwise indicated, for every 62/162,471 15 May 2015 (15.05.2015) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, (71) Applicant: CELLULAR RESEARCH, INC. -

Biosynthesis of Polyketides in Streptomyces
Review Biosynthesis of Polyketides in Streptomyces Chandra Risdian 1,2,*, Tjandrawati Mozef 3 and Joachim Wink 1,* 1 Microbial Strain Collection (MISG), Helmholtz Centre for Infection Research (HZI), 38124 Braunschweig, Germany 2 Research Unit for Clean Technology, Indonesian Institute of Sciences (LIPI), Bandung 40135, Indonesia 3 Research Center for Chemistry, Indonesian Institute of Sciences (LIPI), Serpong 15314, Indonesia; [email protected] * Correspondence: [email protected] or [email protected] (C.R.); [email protected] (J.W.); Tel.: +49-531-6181-4222 (C.R.); +49-531-6181-4223 (J.W.) Received: 18 March 2019; Accepted: 27 April 2019; Published: 6 May 2019 Abstract: Polyketides are a large group of secondary metabolites that have notable variety in their structure and function. Polyketides exhibit a wide range of bioactivities such as antibacterial, antifungal, anticancer, antiviral, immune-suppressing, anti-cholesterol, and anti-inflammatory activity. Naturally, they are found in bacteria, fungi, plants, protists, insects, mollusks, and sponges. Streptomyces is a genus of Gram-positive bacteria that has a filamentous form like fungi. This genus is best known as one of the polyketides producers. Some examples of polyketides produced by Streptomyces are rapamycin, oleandomycin, actinorhodin, daunorubicin, and caprazamycin. Biosynthesis of polyketides involves a group of enzyme activities called polyketide synthases (PKSs). There are three types of PKSs (type I, type II, and type III) in Streptomyces responsible for producing polyketides. This paper focuses on the biosynthesis of polyketides in Streptomyces with three structurally-different types of PKSs. Keywords: Streptomyces; polyketides; secondary metabolite; polyketide synthases (PKSs) 1. Introduction Polyketides, a large group of secondary metabolites, are known to possess remarkable variety, not only in their structure, and but also in their function [1,2]. -

Description and Analysis of Glycosidic Residues in the Largest Open Natural Products Database
biomolecules Article Description and Analysis of Glycosidic Residues in the Largest Open Natural Products Database Jonas Schaub 1 , Achim Zielesny 2, Christoph Steinbeck 1,* and Maria Sorokina 1,* 1 Institute for Inorganic and Analytical Chemistry, Friedrich-Schiller University, Lessing Strasse 8, 07743 Jena, Germany; [email protected] 2 Institute for Bioinformatics and Chemoinformatics, Westphalian University of Applied Sciences, August-Schmidt-Ring 10, 45665 Recklinghausen, Germany; [email protected] * Correspondence: [email protected] (C.S.); [email protected] (M.S.) Abstract: Natural products (NPs), biomolecules produced by living organisms, inspire the pharma- ceutical industry and research due to their structural characteristics and the substituents from which they derive their activities. Glycosidic residues are frequently present in NP structures and have particular pharmacokinetic and pharmacodynamic importance as they improve their solubility and are often involved in molecular transport, target specificity, ligand–target interactions, and receptor binding. The COlleCtion of Open Natural prodUcTs (COCONUT) is currently the largest open database of NPs, and therefore a suitable starting point for the detection and analysis of the diversity of glycosidic residues in NPs. In this work, we report and describe the presence of circular, linear, terminal, and non-terminal glycosidic units in NPs, together with their importance in drug discovery. Keywords: natural products; glycosides; bioactivity; glycosidic residues; sugars; carbohydrates; Citation: Schaub, J.; Zielesny, A.; deglycosylation; cheminformatics; Chemistry Development Kit; CDK Steinbeck, C.; Sorokina, M. Description and Analysis of Glycosidic Residues in the Largest Open Natural Products Database. 1. Introduction Biomolecules 2021, 11, 486. https:// Natural products (NPs) are biologically active molecules produced by living organ- doi.org/10.3390/biom11040486 isms. -

Subject Index
Subject Index A DNA binding 38-40 DNA strand breaks 37 Scatchard plot 36 ACIMBO 146 effects on nuclear nucleic acid 58 Aclacinomycin 59 and nuclear damage 36 Aclacinomycin A 60,63-5,67 Adriamycin macromolecule complexes and catalase 65,71 79 and DNA binding 64 Adriamycin-ara-C 106 and DNA strand breaks 64 Adriamycin-14-benzoate 94 and DNA synthesis 64 Adriamycin-14-(1-naphthalene acetate) and RNA synthesis 64 94 Acridine orange 2 Adriamycin-14-octanoate 94,120 Acridine yellow 3 Agglutination 25 Acridones 26-9 Aklavine 68 alkaloids 28 Aklavinone 59 nitroacridone 27 Albumin microspheres 79 thioacridone 27 Alcindromycin 66 Acriflavine 1, 2 Aldehyde reductase 109 Acrolein 11 0 Alkaline elution 37,206,316,318, Acronycine 28 335,336,344 and DNA synthesis 28 Alkaline sucrose sedimentation 206, detoxification 28 218,222,316,322 metabolism 28 Alkylated DNA 244 and RNA synthesis 28 Alkylated RNA 244 Actinomycins 24, 104, 148 Alkylating acridines 3, 4 inhibition of RNA synthesis 25 Alkylating agents 233ff, 284 Actinomycin D 37,104,129,150 local administration of 264 DNA damage 105 Alkylation of DNA bases 300 AD32 74,97,104 Alkylation products 300 cell cycle effects 74 7-a1kylguanines 300 AD41 97 Alkyltransferase 346,355 Adamanty1 substituents 385 Allopurinol 111 Adenocarcinoma 386 Ametantrone 82-5 Adriamycin 21,35-53,57-86,94, D-aminoacid oxidase 111 96, 104, 108 L-aminoacid oxidase 111 cardiotoxicity of 57 9-aminoacridine 1,18,22,23 chromatin binding 36-7 imino form 10 chromatin compaction 37 Aminopterin 368,380 395 396 Subject Index AML 121 Ataxia -
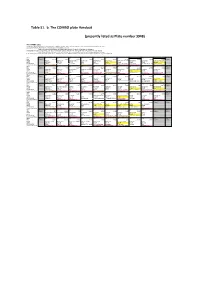
Table S1. B. the COMBO Plate Handout (Presently Listed As Plate
Table S1. b. The COMBO plate Handout (presently listed as Plate number 3948) NCI COMBO plate Compounds approved by FDA (for any indication) are highlighted in pink. Information from http://www.accessdata.fda.gov/scripts/cder/drugsatfda/ Compounds tested in clinical trials (for any indication) are highlighted in orange. Date is the most recent publication found searching pubmed or Google for clinical trials with this agent. Compounds are supplied as 20 microL at the given concentration (approx. 500x the conc. of the GI50 of the least sensitive line in the NCI60) Some compounds were not soluble at the desired conc., these are highlighted in yellow, with the actual conc. plated shown Mechanisms given are from published reports. Some compounds may have additional activities. NCI-DTP has not verified mechanism for any of the compounds. WELL A1 A2 A3 A4 A5 A6 A7 A8 A9 A10 A11 A12 NSC BLANK 332598 89671 681228 56410 289487 166454 312887 169091 65690 129943 BLANK NAME Rhizoxin Brefeldin A Velcade analog Porfiromycin Asterriquinone Dequalinium Fludarabine phosphateMethdilazine Agaric Acid ICRF 159 (Razoxane) milliM 0.005 mM 0.05 mM 0.5 mM 5mM 5mM 3 mM 50 mM 50 mM 50 mM 200 mM MECHANISM Tubulin Arf-GEF Proteasome Alkyl Intercalater Ion channel Nucleoside analog Antihistamine GAPDH; adenine nucleotideTopo II translocase catalytic CLINICAL STATUS Clinical trials (2000) analog of approved agentClinical trials (1997) Clinical trials (2002) FDA approved FDA approved Clinical trials (2000) WELL B1 B2 B3 B4 B5 B6 B7 B8 B9 B10 B11 B12 NSC BLANK 153858