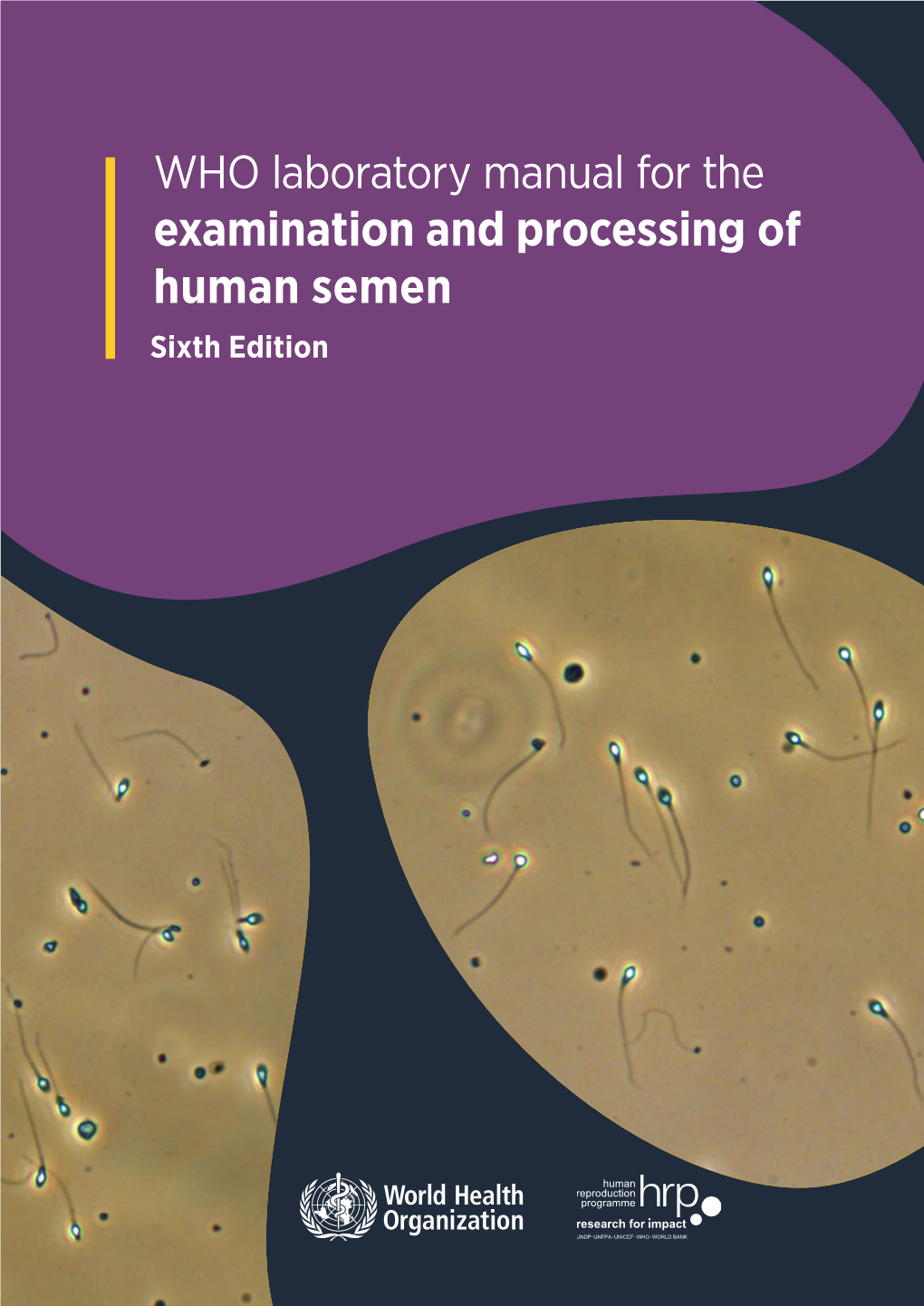
Examination and Processing of Human Semen Sixth Edition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Reference Sheet 1
MALE SEXUAL SYSTEM 8 7 8 OJ 7 .£l"00\.....• ;:; ::>0\~ <Il '"~IQ)I"->. ~cru::>s ~ 6 5 bladder penis prostate gland 4 scrotum seminal vesicle testicle urethra vas deferens FEMALE SEXUAL SYSTEM 2 1 8 " \ 5 ... - ... j 4 labia \ ""\ bladderFallopian"k. "'"f"";".'''¥'&.tube\'WIT / I cervixt r r' \ \ clitorisurethrauterus 7 \ ~~ ;~f4f~ ~:iJ 3 ovaryvagina / ~ 2 / \ \\"- 9 6 adapted from F.L.A.S.H. Reproductive System Reference Sheet 3: GLOSSARY Anus – The opening in the buttocks from which bowel movements come when a person goes to the bathroom. It is part of the digestive system; it gets rid of body wastes. Buttocks – The medical word for a person’s “bottom” or “rear end.” Cervix – The opening of the uterus into the vagina. Circumcision – An operation to remove the foreskin from the penis. Cowper’s Glands – Glands on either side of the urethra that make a discharge which lines the urethra when a man gets an erection, making it less acid-like to protect the sperm. Clitoris – The part of the female genitals that’s full of nerves and becomes erect. It has a glans and a shaft like the penis, but only its glans is on the out side of the body, and it’s much smaller. Discharge – Liquid. Urine and semen are kinds of discharge, but the word is usually used to describe either the normal wetness of the vagina or the abnormal wetness that may come from an infection in the penis or vagina. Duct – Tube, the fallopian tubes may be called oviducts, because they are the path for an ovum. -

THE PHYSIOLOGY and ECOPHYSIOLOGY of EJACULATION Tropical and Subtropical Agroecosystems, Vol
Tropical and Subtropical Agroecosystems E-ISSN: 1870-0462 [email protected] Universidad Autónoma de Yucatán México Lucio, R. A.; Cruz, Y.; Pichardo, A. I.; Fuentes-Morales, M. R.; Fuentes-Farias, A.L.; Molina-Cerón, M. L.; Gutiérrez-Ospina, G. THE PHYSIOLOGY AND ECOPHYSIOLOGY OF EJACULATION Tropical and Subtropical Agroecosystems, vol. 15, núm. 1, 2012, pp. S113-S127 Universidad Autónoma de Yucatán Mérida, Yucatán, México Available in: http://www.redalyc.org/articulo.oa?id=93924484010 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Tropical and Subtropical Agroecosystems, 15 (2012) SUP 1: S113 – S127 REVIEW [REVISIÓN] THE PHYSIOLOGY AND ECOPHYSIOLOGY OF EJACULATION [FISIOLOGÍA Y ECOFISIOLOGÍA DE LA EYACULACIÓN] R. A. Lucio1*, Y. Cruz1, A. I. Pichardo2, M. R. Fuentes-Morales1, A.L. Fuentes-Farias3, M. L. Molina-Cerón2 and G. Gutiérrez-Ospina2 1Centro Tlaxcala de Biología de la Conducta, Universidad Autónoma de Tlaxcala, Tlaxcala-Puebla km 1.5 s/n, Loma Xicotencatl, 90062, Tlaxcala, Tlax., México. 2Depto. Biología Celular y Fisiología, Instituto de Investigaciones Biomédicas, Universidad Nacional Autónoma de México, Ciudad Universitaria, 04510, México, D.F., México. 3Laboratorio de Ecofisiologia Animal, Departamento de Fisiologia, Instituto de Investigaciones sobre los Recursos Naturales, Universidad Michoacana de San Nicolás de Hidalgo, Av. San Juanito Itzicuaro s/n, Colonia Nueva Esperanza 58337, Morelia, Mich., México * Corresponding author ABSTRACT RESUMEN Different studies dealing with ejaculation view this Diferentes estudios enfocados en la eyaculación, process as a part of the male copulatory behavior. -
Andrology User Handbook
Document code: AY.P001 Version number: 7 Date of issue: 29/06/2020 USER HANDBOOK FOR ANDROLOGY SERVICES Diagnostic Semen Analysis Post Vasectomy Semen Analysis Retrograde Ejaculation Analysis Page 1 of 24 Document code: AY.P001 Version number: 7 Date of issue: 29/06/2020 Contents: 1. Introduction .................................................................................................................... 3 2. Location and Opening Times .......................................................................................... 4 3. Useful contacts ............................................................................................................... 4 4. Services provided by the laboratory ............................................................................... 5 5. Requesting semen analysis ............................................................................................ 5 6. Analysis test types .......................................................................................................... 8 6.1 Diagnostic semen analysis (DSA) test for fertility ......................................................... 8 6.1a Instructions for collection of a semen sample for DSA (fertility)............................... 9 6.1b How Diagnostic Semen Analysis assessments are reported .................................10 6.2 Retrograde Analysis ....................................................................................................11 6.2a Instructions for collection of urine for retrograde ejaculation -

Semen Arousal: Its Prevalence, Relationship to HIV Risk Practices
C S & lini ID ca A l f R o e l s Klein, J AIDS Clin Res 2016, 7:2 a e Journal of n a r r DOI: 10.4172/2155-6113.1000546 c u h o J ISSN: 2155-6113 AIDS & Clinical Research Research Article Open Access Semen Arousal: Its Prevalence, Relationship to HIV Risk Practices, and Predictors among Men Using the Internet to Find Male Partners for Unprotected Sex Hugh Klein* Kensington Research Institute, USA Abstract Purpose: This paper examines the extent to which men who use the Internet to find other men for unprotected sex are aroused by semen. It also looks at the relationship between semen arousal and involvement in HIV risk practices, and the factors associated with higher levels of semen arousal. Methods: 332 men who used any of 16 websites targeting unprotected sex completed 90-minute telephone interviews. Both quantitative and qualitative data were collected. A random sampling strategy was used. Semen arousal was assessed by four questions asking men how much they were turned on by the way that semen smelled, tasted, looked, and felt. Results: 65.1% of the men found at least one sensory aspect of semen to be “fairly” or “very” arousing, compared to 10.2% being “not very” or “not at all” aroused by all four sensory aspects of semen. Multivariate analysis revealed that semen arousal was related to greater involvement in HIV risk practices, even when the impact of other salient factors such as demographic characteristics, HIV serostatus, and psychological functioning was taken into account. Five factors were found to underlie greater levels of semen arousal: not being African American, self-identification as a sexual “bottom,” being better educated, being HIV-positive, and being more depressed. -

INTRAUTERINE INSEMINATION of HUSBAND's SEMEN Departments
INTRAUTERINE INSEMINATION OF HUSBAND'S SEMEN B. N. BARWIN Departments of Physiology and Midwifery & Gynaecology, The Queen's University of Belfast, Northern Ireland (Received 11 th January 1973) Summary. Fifty patients with primary infertility were treated by intra- uterine insemination of the husband's semen which had been stored. Thirty patients had sperm counts of greater than 20 \m=x\106/ml with 50% motility and twenty patients had oligospermia (<20 \m=x\106/ml). The technique of storage of semen is reported and the intrauterine method described. The r\l=o^\leof the buffer solution is discussed in over- coming the complications of intrauterine insemination. A success rate of 70% is reported in the normospermic group and 55% in the oligo- spermic group over nine cycles of intrauterine insemination of husband's semen. INTRODUCTION One of the main problems confronting the gynaecologist in the investigation of infertility is the consistent finding of immotile spermatozoa, spermatozoa of low motility and low sperm count in the cervical mucus or semen (Scott, 1968). There was considerable controversy among earlier workers in the field that the sperm count was substandard if it fell below 60 106/ml but MacLeod (1962) has carried out considerable research in this field and it is now generally accepted that true oligospermia is represented by counts of less than 20 IO6/ ml provided the motility is good. SUBJECTS AND METHODS Selection of cases Fifty couples with primary infertility of between 3 and 14 years' duration were selected. The age distribution was between 24 and 41 years. In all cases, the wives had been subjected to a full clinical investigation. -

Prevention of Infections in an Artificial Insemination Program
SPERM ONLY PLEASE: Prevention of infections in an artificial insemination program Carin Huyser Reproductive and Endocrine Unit Department Ob/Gyn University of Pretoria Steve Biko Academic Hospital South Africa [email protected] ESHRE Campus workshop Genk Belgium, 15 December 2009 1 CONTENT I. Introduction Infection and contamination control Environment Staff Supplies Patients & specimens II. Aim Origin & prevention III. Prevalence (origin) of pathogens in ART Bacteria and STIs Viruses Interaction STI & HIV IV. Risk reduction (prevention) Screening & counselling Semen washing Validation of specimens ART procedure: IUI versus IVF/ICSI V. Discussion & Conclusion VI. Acknowledgements 2 I. INTRODUCTION ‘Semen contains vitality & heredity, not germs ’: seminal discourse in the AIDS era 1. Infection and contamination control in ART laboratory 2-4: Environment (inside & outside of lab e.g. Pseudomona spp. in water, fungal spores in air) Staff (individuals & techniques) Facilities & supplies (equipment, eg. cryostorage tanks; media) PatientsPatients & & specimens specimens 1. Khan et al . J Health Popul Nutr 2006; 24 :195-200; 2. Englert et al . Hum Reprod Update 2004; 10 :149-162; 3. Elder, Baker & Ribes. Infections, 3 Infertility and Assisted Reproduction 2005; 4. Magli et al . Hum Reprod 2008; 23 :1253-1262 I. INTRODUCTION Infection and contamination control in ART laboratory 1: Patients & specimens (semen ) Prevalence of pathogens (origin) Risk reduction (prevent) BBV+ BBV+ Fig 1: Prediction of reproductive potential 1. Elder, Baker & Ribes. Infections, Infertility and Assisted Reproduction. 2005 4 I. INTRODUCTION Infection and contamination control in ART laboratory 2: Patients & specimens (semen ) Prevalence of pathogens (origin) Risk reduction (prevent) BBV+/- BBV+/- Fig 1: Prediction of reproductive potential 1. -

Commentary Unprotected: Condoms, Bareback Porn, and the First Amendment
Commentary Unprotected: Condoms, Bareback Porn, and the First Amendment Bailey J. Langnert ABSTRACT In November 2012, Los Angeles County voters passed Measure B, or the Safer Sex in the Adult Film Industry Act. Measure B mandated condom use by all porn performers in adult films produced within county borders and created a complex regulatory process for adult film producers that included permitting, mandatory public health trainings, and warrantless administrative searches. Shortly after its passage, Vivid Entertainment filed a lawsuit to enjoin the enforcement of Measure B, arguing that the Measure violated their First Amendment right to portray condomless sex in porn. In December 2014, the Ninth Circuit upheld the district court's decision upholding the constitutionality of Measure B. Notably, the mainstream discourse surrounding the Measure B campaign, as well as the legal arguments put forth in the lawsuit, focused exclusively on straight pornography while purporting to represent all porn. As a result, an entire genre of condomless pornography went unrepresented in the discussion: bareback porn, which portrays intentional unprotected anal sex between men. Excluding bareback porn from the lawsuit represented a missed opportunityfor Vivid in its challenge of Measure B. There are several political messages underlying bareback porn unique to that genre that might have resulted in the t The author received a law degree from the University of California, Berkeley, School of Law (Boalt Hall) in 2015. As a law student, the author worked as a Teaching Assistant in the First Year Legal Writing Program and served as a Senior Board Member of the Boalt Hall Women's Association. -

Illuminating Dna Packaging in Sperm Chromatin: How Polycation Lengths, Underprotamination and Disulfide Linkages Alters Dna Condensation and Stability
University of Kentucky UKnowledge Theses and Dissertations--Chemistry Chemistry 2019 ILLUMINATING DNA PACKAGING IN SPERM CHROMATIN: HOW POLYCATION LENGTHS, UNDERPROTAMINATION AND DISULFIDE LINKAGES ALTERS DNA CONDENSATION AND STABILITY Daniel Kirchhoff University of Kentucky, [email protected] Digital Object Identifier: https://doi.org/10.13023/etd.2019.233 Right click to open a feedback form in a new tab to let us know how this document benefits ou.y Recommended Citation Kirchhoff, Daniel, "ILLUMINATING DNA PACKAGING IN SPERM CHROMATIN: HOW POLYCATION LENGTHS, UNDERPROTAMINATION AND DISULFIDE LINKAGES ALTERS DNA CONDENSATION AND STABILITY" (2019). Theses and Dissertations--Chemistry. 112. https://uknowledge.uky.edu/chemistry_etds/112 This Doctoral Dissertation is brought to you for free and open access by the Chemistry at UKnowledge. It has been accepted for inclusion in Theses and Dissertations--Chemistry by an authorized administrator of UKnowledge. For more information, please contact [email protected]. STUDENT AGREEMENT: I represent that my thesis or dissertation and abstract are my original work. Proper attribution has been given to all outside sources. I understand that I am solely responsible for obtaining any needed copyright permissions. I have obtained needed written permission statement(s) from the owner(s) of each third-party copyrighted matter to be included in my work, allowing electronic distribution (if such use is not permitted by the fair use doctrine) which will be submitted to UKnowledge as Additional File. I hereby grant to The University of Kentucky and its agents the irrevocable, non-exclusive, and royalty-free license to archive and make accessible my work in whole or in part in all forms of media, now or hereafter known. -

Aloe Ferox 117 Table 9: Phytochemical Constituents of Different Extracts of Aloe CIM- Sheetal Leaves 119
International Journal of Scientific & Engineering Research ISSN 2229-5518 1 Morphological, in vitro, Biochemical and Genetic Diversity Studies in Aloe species THESIS SUBMITTED TO OSMANIA UNIVERSITY FOR THE AWARD OF DOCTOR OF PHILOSOPHY IN GENETICS IJSER By B. CHANDRA SEKHAR SINGH DEPARTMENT OF GENETICS OSMANIA UNIVERSITY HYDERABAD - 500007, INDIA JULY, 2015 IJSER © 2018 http://www.ijser.org International Journal of Scientific & Engineering Research ISSN 2229-5518 2 DECLARATION The investigation incorporated in the thesis entitled “Morphological, in vitro, Biochemical and Genetic Diversity Studies in Aloe species’’ was carried out by me at the Department of Genetics, Osmania University, Hyderabad, India under the supervision of Prof. Anupalli Roja Rani, Osmania University, Hyderabad, India. I hereby declare that the work is original and no part of the thesis has been submitted for the award of any other degree or diploma prior to this date. IJSER Date: (Bhaludra Chandra Sekhar Singh) IJSER © 2018 http://www.ijser.org International Journal of Scientific & Engineering Research ISSN 2229-5518 3 DEDICATION I dedicateIJSER this work to my beloved and beautiful wife B. Ananda Sekhar IJSER © 2018 http://www.ijser.org International Journal of Scientific & Engineering Research ISSN 2229-5518 4 Acknowledgements This dissertation is an outcome of direct and indirect contribution of many people, which supplemented my own humble efforts. I like this opportunity to mention specifically some of them and extend my gratefulness to other well wisher, known and unknown. I feel extremely privileged to express my veneration for my superviosor Dr. Anupalli Roja Rani, Professor and Head, Department of Genetics, Osmania University, Hyderabad. Her whole- hearted co-operation, inspiration and encouragement rendered throughout made this in carrying out the research and writing of this thesis possible. -
The Impact of Testicular Torsion on Testicular Function
Review Article pISSN: 2287-4208 / eISSN: 2287-4690 World J Mens Health Published online Apr 10, 2019 https://doi.org/10.5534/wjmh.190037 The Impact of Testicular Torsion on Testicular Function Frederik M. Jacobsen1 , Trine M. Rudlang1 , Mikkel Fode1 , Peter B. Østergren1 , Jens Sønksen1 , Dana A. Ohl2 , Christian Fuglesang S. Jensen1 ; On behalf of the CopMich Collaborative 1Department of Urology, Herlev and Gentofte Hospital, University of Copenhagen, Herlev, Denmark, 2Department of Urology, University of Michigan, Ann Arbor, MI, USA Torsion of the spermatic cord is a urological emergency that must be treated with acute surgery. Possible long-term effects of torsion on testicular function are controversial. This review aims to address the impact of testicular torsion (TT) on the endo- crine- and exocrine-function of the testis, including possible negative effects of torsion on the function of the contralateral testis. Testis tissue survival after TT is dependent on the degree and duration of TT. TT has been demonstrated to cause long- term decrease in sperm motility and reduce overall sperm counts. Reduced semen quality might be caused by ischemic dam- age and reperfusion injury. In contrast, most studies find endocrine parameters to be unaffected after torsion, although few report minor alterations in levels of gonadotropins and testosterone. Contralateral damage after unilateral TT has been sug- gested by histological abnormalities in the contralateral testis after orchiectomy of the torsed testis. The evidence is, however, limited as most human studies are small case-series. Theories as to what causes contralateral damage mainly derive from animal studies making it difficult to interpret the results in a human context. -

Gay Men and Barebacking: Radical Or Realistic?
Eric J. Roberson ENG 3305 – Essay Writing Dr. JoAnn Pavletich – UHD Fall 2009 Semester 2 Dec. 2009 Gay Men and Barebacking: Radical or Realistic? By Eric J. Roberson Prepared for Dr. JoAnn Pavletich ENG 3305 Advanced Essay Writing Fall 2009 Semester Gay Men and Barebacking: Radical or Realistic? Page 1 of 17 By Eric J. Roberson Gay Men and “Barebacking”: Radical or Realistic? By Eric J. Roberson Sex is not a competitive sport, and if you are gay and think it is then you should listen up! “HIV is a serious long-term condition, and young gay men remain the group of young people most at risk” (“UK Same-Sex Relationships 1). Some gay men willfully and deliberately discard condoms in preference for unprotected sex. Regardless of your age, this essay will not convince you on what to do with your “hard on,” but it may help you decide to get tested and to put on a condom before your next casual sexual encounter. Consider these three simple solutions: communication before sex, compassion for others, and condoms for casual encounters. If you happen to be straight and are reading this essay, do not put it down. Straight people who have gay friends may learn about some of the challenges gay men face in leading fulfilling relationships. You may also gain ideas on how to be more supportive. Regardless of your sexual orientation, the goal is to expose how the internet has shaped the practice of barebacking and other mitigating factors that compel gay men to consciously and explicitly eschew condoms during anal intercourse – colloquially known as “barebacking” (Gastaldo, et. -

Artificial Insemination
Ch36-A03309.qxd 1/23/07 5:16 PM Page 539 Section 6 Infertility and Recurrent Pregnancy Loss Chapter Artificial Insemination 36 Ashok Agarwal and Shyam S. R. Allamaneni INTRODUCTION widely available, the terms homologous artificial insemination and heterologous artificial insemination were used to differentiate Artificial insemination is an assisted conception method that can these two alternative sources. However, the use of these bio- be used to alleviate infertility in selected couples. The rationale medical terms in this manner is at variance with their scientific behind the use of artificial insemination is to increase the gamete meaning, where they denote different species or organisms (as in, density near the site of fertilization.1 The effectiveness of artificial e.g., homologous and heterologous tissue grafts). insemination has been clearly established in specific subsets of In the latter half of the 20th century, the terms artificial infertile patients such as those with idiopathic infertility, infertility insemination, donor (AID) and artificial insemination, husband related to a cervical factor, or a mild male factor infertility (AIH) found common use. However, the widespread use of the (Table 36-1).2,3 An accepted advantage of artificial insemination acronym AIDS for acquired immunodeficiency syndrome resulted is that it is generally less expensive and invasive than other in the replacement of AID with therapeutic donor insemination assisted reproductive technology (ART) procedures.4 (TDI). An analogous alternative term for AIH has not evolved, This chapter provides a comprehensive description of probably in part because of the increasingly common situation indications for artificial insemination, issues to consider before where the woman’s partner is not her legal husband.