WPV Outbreak Response Somalia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
SOMALIA, YEAR 2019: Update on Incidents According to the Armed Conflict Location & Event Data Project (ACLED) Compiled by ACCORD, 22 June 2020
SOMALIA, YEAR 2019: Update on incidents according to the Armed Conflict Location & Event Data Project (ACLED) compiled by ACCORD, 22 June 2020 Number of reported incidents with at least one fatality Number of reported fatalities National borders: GADM, November 2015a; administrative divisions: GADM, November 2015b; Ethiopia/Somalia bor- der status: CIA, 2014; incident data: ACLED, 13 June 2020; coastlines and inland waters: Smith and Wessel, 1 May 2015 SOMALIA, YEAR 2019: UPDATE ON INCIDENTS ACCORDING TO THE ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) COMPILED BY ACCORD, 22 JUNE 2020 Contents Conflict incidents by category Number of Number of reported fatalities 1 Number of Number of Category incidents with at incidents fatalities Number of reported incidents with at least one fatality 1 least one fatality Battles 1131 458 2154 Conflict incidents by category 2 Explosions / Remote 621 228 1221 Development of conflict incidents from 2010 to 2019 2 violence Violence against civilians 530 358 640 Methodology 3 Strategic developments 140 6 16 Conflict incidents per province 4 Protests 78 2 2 Riots 19 3 5 Localization of conflict incidents 4 Total 2519 1055 4038 Disclaimer 6 This table is based on data from ACLED (datasets used: ACLED, 13 June 2020). Development of conflict incidents from 2010 to 2019 This graph is based on data from ACLED (datasets used: ACLED, 13 June 2020). 2 SOMALIA, YEAR 2019: UPDATE ON INCIDENTS ACCORDING TO THE ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) COMPILED BY ACCORD, 22 JUNE 2020 Methodology on what level of detail is reported. Thus, towns may represent the wider region in which an incident occured, or the provincial capital may be used if only the province The data used in this report was collected by the Armed Conflict Location & Event is known. -

South and Central Somalia Security Situation, Al-Shabaab Presence, and Target Groups
1/2017 South and Central Somalia Security Situation, al-Shabaab Presence, and Target Groups Report based on interviews in Nairobi, Kenya, 3 to 10 December 2016 Copenhagen, March 2017 Danish Immigration Service Ryesgade 53 2100 Copenhagen Ø Phone: 00 45 35 36 66 00 Web: www.newtodenmark.dk E-mail: [email protected] South and Central Somalia: Security Situation, al-Shabaab Presence, and Target Groups Table of Contents Disclaimer .......................................................................................................................................................... 3 Introduction and methodology ......................................................................................................................... 4 Abbreviations..................................................................................................................................................... 6 1. Security situation ....................................................................................................................................... 7 1.1. The overall security situation ........................................................................................................ 7 1.2. The extent of al-Shabaab control and presence.......................................................................... 10 1.3. Information on the security situation in selected cities/regions ................................................ 11 2. Possible al-Shabaab targets in areas with AMISOM/SNA presence ....................................................... -

Somalia Energy Sector Needs Assessment and Investment Programme November 2015 Somalia - Energy Sector Needs Assessment and Investment Programme
Somalia Energy Sector Needs Assessment and Investment Programme November 2015 Somalia - Energy Sector Needs Assessment and Investment Programme Copyright © 2015 African Development Bank Group Immeuble du Centre de commerce International d’Abidjan CCIA Avenue Jean-Paul II 01 BP 1387 Abidjan 01, Côte d'Ivoire Phone (Standard): +225 20 26 10 20 Internet: www.afdb.org Rights and Permissions All rights reserved. The text and data in this publication may be reproduced as long as the source is cited. Reproduction for commercial purposes is forbidden. Legal Disclaimer The findings, interpretations and conclusions expressed in this report are those of the author/s and are not necessarily those of the African Development Bank. In the preparation of this document, every effort has been made to offer the most current, correct and clearly expressed information possible. Nonetheless, inadvertent errors can occur, and appli - cable laws, rules and regulations may change. The African Development Bank makes its documentation available wi - thout warranty of any kind and accepts no responsibility for its accuracy or for any consequences of its use. Cover design: AfDB Cover photos: Image © AU-UN IST PHOTO/Ilyas A. Abukar; Image © NIGEL CARR ii Somalia - Energy Sector Needs Assessment and Investment Programme Table of contents Foreword v Ackonwledgements vii Abbreviations and acronyms ix Executive summary xi 1. Introduction and background 1 1.1. Introduction 1 1.2. Objectives/scope 3 1.3. Brief description of the current energy sector 3 1.4. Sector organisation and policies 4 1.5. Reliance on the private sector 5 1.6. Four main issues facing Somalia’s energy sector 6 2. -

Security Council Seventy-Sixth Year 8779Th Meeting
United Nations S/PV.8779 Security Council Provisional Seventy-sixth year 8779th meeting Tuesday, 25 May 2021, 10 a.m. New York President: Mr. Zhang Jun/Mr. Dai Bing ....................... (China) Members: Estonia ........................................ Mr. Jürgenson France ........................................ Mrs. Broadhurst Estival India ......................................... Mr. Raguttahalli Ireland ........................................ Ms. Byrne Nason Kenya. Mr. Kimani Mexico ........................................ Mr. De la Fuente Ramírez Niger ......................................... Mr. Abarry Norway ....................................... Ms. Juul Russian Federation ............................... Mr. Nebenzia Saint Vincent and the Grenadines ................... Ms. DeShong Tunisia ........................................ Mr. Ladeb United Kingdom of Great Britain and Northern Ireland .. Dame Barbara Woodward United States of America .......................... Mr. Mills Viet Nam ...................................... Mr. Dang Agenda The situation in Somalia Report of the Secretary-General on the situation in Somalia (S/2021/485) This record contains the text of speeches delivered in English and of the translation of speeches delivered in other languages. The final text will be printed in the Official Records of the Security Council. Corrections should be submitted to the original languages only. They should be incorporated in a copy of the record and sent under the signature of a member of the delegation concerned -
SOMALIA, SECOND QUARTER 2020: Update on Incidents According to the Armed Conflict Location & Event Data Project (ACLED) Compiled by ACCORD, 30 October 2020
SOMALIA, SECOND QUARTER 2020: Update on incidents according to the Armed Conflict Location & Event Data Project (ACLED) compiled by ACCORD, 30 October 2020 Number of reported incidents with at least one fatality Number of reported fatalities National borders: GADM, November 2015a; administrative divisions: GADM, November 2015b; Ethiopia/Somalia border status: CIA, 2014; incident data: ACLED, 3 October 2020; coastlines and inland waters: Smith and Wessel, 1 May 2015 SOMALIA, SECOND QUARTER 2020: UPDATE ON INCIDENTS ACCORDING TO THE ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) COMPILED BY ACCORD, 30 OCTOBER 2020 Contents Conflict incidents by category Number of Number of reported fatalities 1 Number of Number of Category incidents with at incidents fatalities Number of reported incidents with at least one fatality 1 least one fatality Battles 327 152 465 Conflict incidents by category 2 Violence against civilians 146 100 144 Development of conflict incidents from June 2018 to June 2020 2 Explosions / Remote 133 59 187 violence Methodology 3 Protests 28 1 1 Conflict incidents per province 4 Strategic developments 18 2 2 Riots 6 0 0 Localization of conflict incidents 4 Total 658 314 799 Disclaimer 6 This table is based on data from ACLED (datasets used: ACLED, 3 October 2020). Development of conflict incidents from June 2018 to June 2020 This graph is based on data from ACLED (datasets used: ACLED, 3 October 2020). 2 SOMALIA, SECOND QUARTER 2020: UPDATE ON INCIDENTS ACCORDING TO THE ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) COMPILED BY ACCORD, 30 OCTOBER 2020 Methodology on what level of detail is reported. Thus, towns may represent the wider region in which an incident occured, or the provincial capital may be used if only the province The data used in this report was collected by the Armed Conflict Location & Event is known. -

S/2021/723 Security Council
United Nations S/2021/723 Security Council Distr.: General 10 August 2021 Original: English Situation in Somalia Report of the Secretary-General I. Introduction 1. The present report, submitted pursuant to paragraph 16 of Security Council resolution 2540 (2020) and paragraph 41 of resolution 2568 (2021), provides updates on the implementation of those resolutions, including on the mandates of the United Nations Assistance Mission in Somalia (UNSOM) and the United Nations Support Office in Somalia (UNSOS). The report covers significant developments from 8 May to 31 July 2021. II. Political, security and economic overview A. Political developments 2. Progress was made towards holding the delayed elections. The National Consultative Council met between 22 and 27 May. It brought together Federal Government and federal member state leaders, the Governor of the Banaadir Regional Administration and the Mayor of Mogadishu. It reached an agreement to resolve the contentious issues in the implementation of the agreement of 17 September based on the recommendation made by the technical committee in Baidoa. Those issues included the composition of electoral management and dispute resolution teams, the composition of an electoral management committee on “Somaliland” seats and arrangements for holding national elections in the Gedo Region of Jubbaland. The Council reiterated its commitment to safeguarding the 30 per cent quota for the parliamentary representation of women, but fell short of identifying an implementation mechanism. Somali leaders also -

PROTECTION of CIVILIANS REPORT Building the Foundation for Peace, Security and Human Rights in Somalia
UNSOM UNITED NATIONS ASSISTANCE MISSION IN SOMALIA PROTECTION OF CIVILIANS REPORT Building the Foundation for Peace, Security and Human Rights in Somalia 1 JANUARY 2017 – 31 DECEMBER 2019 Table of Contents Executive Summary .......................................................................................................................1 Methodology ...................................................................................................................................7 Civilian Casualties Attributed to non-State Actors ....................................................................9 A. Al Shabaab .............................................................................................................................9 B. Ahlu Sunna Wal Jama ..........................................................................................................16 C. Clan Militia ..........................................................................................................................17 D. The Islamic State Affiliated Group ......................................................................................17 Civilian Casualties Attributed to State Actors and other Actors ............................................18 A. Somali National Army ...................................................................................................18 B. Somali Police Force .......................................................................................................21 C. The National Intelligence Security Agency -
Iom Somalia Programmatic Overview
1 IOM SOMALIA 2020 PROGRAMMATIC OVERVIEW 2020 IOM SOMALIA PROGRAMMATIC OVERVIEW SOMALIA 2 IOM SOMALIA 2020 PROGRAMMATIC OVERVIEW Front-cover photo: A group of residents from Barwaaqo 2 attend an information session with IOM in the community centre constructed in 2019 in Baidoa. © IOM/Foresight 2020 Photo above: A migrant mother and her child come to the IOM Migration Response Centre in Hargeisa to get health assistance and support. © IOM/Muse Mohamed 2020 DISCLAIMER: The names and boundaries shown do not imply official endorsement nor acceptance by IOM. They are meant for illustrative purposes. EDITORS: Yuko Tomita, Claudia Barrios Rosel, Erin Bowser, Jan Van’t Land LAYOUT DESIGN: Claudia Barrios Rosel 3 IOM SOMALIA 2020 PROGRAMMATIC OVERVIEW IOM SOMALIA 2020 OVERVIEW CONTENT IOM OVERVIEW MAIN ACHIEVEMENTS HUMANITARIAN RESPONSE Camp Coordination and Camp Management (CCCM) Displacement Tracking Matrix (DTM) Water, Sanitation and Hygiene (WASH) Migration, Environment and Climate Change (MECC) Health Shelter and Non-Food Items (S-NFI) STABILIZATION, TRANSITION AND RECOVERY Recovery and Durable Solutions (RDS) Disengagement, Disassociation, Reintegration and Reconciliation (DDRR) MIGRATION GOVERNANCE & DEVELOPMENT Immigration and Border Management (IBM) Labour Mobility and Human Development (LHD) Migrant Protection and Assistance (MPA) 4 IOM SOMALIA 2020 PROGRAMMATIC OVERVIEW IOM’S PRESENCE IN SOMALIA IN 2020 BOSASO AWDAL BERBERA SANAAG DHARAR BARI HARGEISA GARADAG WOQOOYI GALBEED TOGDHEER GAROWE SOOL NUGAAL MUDUG ADADO GALGADUUD BAKOOL DOLOW -
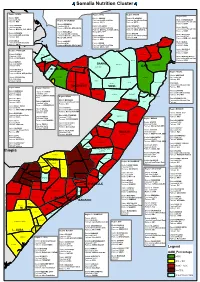
Pdf | 433.9 Kb
Somalia Nutrition Cluster Region: ADWAL Region: SOOL Region: SANAG Region:BARI District: BAKI District: AINABO District: EL AFWEIN Caseload 5,214 Region: W. GALBEED Caseload Insufficient Data Caseload Insufficient Data District: ISKUSHUBAN Partners: WVI Partners: SRCS Partners: SRCS Caseload Insufficient Data District: BERBERA Partners: HADO District BOROMA Caseload 8,274 District LAS ANOD District ERIGAVO District GARDO Caseload 36,498 Partners: MOH SL ,HPA, SRCS Caseload Insufficient Data Caseload Insufficient Data Caseload Insufficient Data Partners: MOH SL, SCI, SRCS Partners: MOH SL, SCODO,SRCS, Partners: SRCS, MOH SL Partners: HADO District HARGEISA Mercy USA, APD District LUGHAYA District BADAN Caseload Insufficient Data District BOSSASO Caseload Insufficient Data Partners: MOH SL , WVI, HPA, District TALEH Caseload Insufficient Data Partners: WVI i Caseload 26,791 t Mercy USA, SRCS Caseload Insufficient Data Partners: APD Partners: BHM , SCI, HADO u Partners: APD District ZEILA o District GABILEY District ALULA Caseload Insufficient Data ALULA b Caseload 4,741 District HUDUN Caseload 5,686 Partners: SRCS ji ZEILA Partners: MOH SL, SRCS, WVI Caseload Insufficient Data Partners: HADO D Partners: SRCS, APD ^` District QANDALA Region: TOGDHEER Caseload 6,417 QANDALA Partners: HADO District: SHEIKH ZEILA BOSSASO Caseload 4,630 EL AFWEIN District BENDER BAYLA Partners: SRCS,HPA LUGHAYA Caseload Insufficient Data BAKI ^` BADAN Partners: HADO District BURAO AWDAL BERBERA Caseload 44,341 BAKI SANAG ERIGAVO ISKUSHUBAN Partners: HPA BORAMA -

S/2019/799 Security Council
United Nations S/2019/799 Security Council Distr.: General 7 October 2019 Original: English Letter dated 7 October 2019 from the Chair of the Security Council Committee pursuant to resolution 751 (1992) concerning Somalia addressed to the President of the Security Council On behalf of the Security Council Committee pursuant to resolution 751 (1992) concerning Somalia, I have the honour to transmit herewith the report of the Under- Secretary-General for Humanitarian Affairs and Emergency Relief Coordinator pursuant to paragraph 49 of Security Council resolution 2444 (2018) on the delivery of humanitarian assistance in Somalia and any impediments to the delivery of humanitarian assistance in Somalia. I would appreciate it if the present letter and the report were brought to the attention of the members of the Security Council and issued as a document of the Council. (Signed) Marc Pecsteen de Buytswerve Chair Security Council Committee pursuant to resolution 751 (1992) concerning Somalia 19-15937 (E) 091019 *1915937* S/2019/799 Letter dated 13 September 2019 from the Under-Secretary-General for Humanitarian Affairs and Emergency Relief Coordinator addressed to the Chair of the Security Council Committee pursuant to resolution 751 (1992) concerning Somalia In accordance with paragraph 49 of Security Council resolution 2444 (2018), I have the honour to transmit the requested report on the implementation of paragraphs 48 and 49 and on any impediments to the delivery of humanitarian assistance in Somalia. The humanitarian community working in Somalia wishes to advise that, as with the previous 13 reports, it maintains the definition of “implementing partner” pursuant to paragraph 5 of Security Council resolution 1916 (2010), which is as follows: “Implementing partner” – a non-governmental organization (NGO) or community-based organization that has undergone due diligence to establish its bona fides by a United Nations agency or another NGO and that reports when requested to the Resident and Humanitarian Coordinator for Somalia on mitigation measures. -

Somalia Polio Outbreak Update for the Polio Eradication Independent Monitoring Board - October 2013
Somalia polio outbreak update For the Polio Eradication Independent Monitoring Board - October 2013 - Somalia Ministry of Health WHO/UNICEF – Somalia Layout 1.Epidemiology update 2.Outbreak response activities 3.Impact of outbreak response activities 4.Additional activities 5.What is next? History of WPV circulation, Somalia Districts with WPV cases, 2000 Districts with WPV cases after re-introduction from 2005 2007 2000 2005 2006 2007 Re-introduction Re-introduction WPV Non Polio AFP 120 Circulation interrupted 100 Last indigenous case 80 60 40 20 0 1 3 5 7 9 11 1 3 5 7 9 11 1 3 5 7 9 11 1 3 5 7 9 11 1 3 5 7 9 11 1 3 5 7 9 11 1 3 5 7 9 11 1 3 5 7 9 11 1 3 5 7 9 11 1 3 5 7 9 11 1 3 5 7 9 11 1 3 5 7 9 11 1 3 5 7 9 11 1 3 5 7 9 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2013 WPV update* On May 2013, a WPV case was notified from Somalia, from a 32 months old girl, date of onset 18 April 2013, resident of Hamar Jabjab district in (Mogadishu) WPV NON POLIO AFP PENDING LAB RESULTS 50 40 30 20 10 Case Case Count 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 Epi Weeks April: 4 districts infected May: 23 districts infected June: 36 districts infected July: 45 districts infected Sept: 46 districts infected From its epicenter in Mogadishu, the outbreak expanded to the other districts of South and Central Somalia and more recently to the Somaliland and Puntland * Data as of Sept 20, 2013 WPV outbreak and accessibility • Since 2010, 40 districts in South and Somaliland -

Ministry of Interior, Federal Affairs and Reconciliation Federal Government of Somalia S2S II
Ministry of Interior, Federal Affairs and Reconciliation Federal Government of Somalia S2S II CAS Stabilization Coordination Meeting Note 30th September 2019 Venue: VIP AMISOM, Mogadishu, Somalia + VTC with UNON, Nairobi, Kenya Agenda: 1. Welcoming remarks / Introduction 2. Lower-Shabelle Stabilization Support (progress and challenges) 3. FIMM (Data collection and analytical tool) presentation 4. Support to Stabilization Phase II (S2S project) 5. FMS update (resource mobilization and gaps) 6. Partners update 7. AoB and next steps Opening Remarks: MoIFAR: Senior Stabilization Advisor, opened the meeting and noted that the Minister was continuing to support efforts on reconciliation in Galmudug. The importance of the coordination forum for both federal and state governments for information sharing on achievements, plans and challenges was highlighted. MoIFAR commended the generosity of donors and commitments by the partners in implementing the stabilization projects effectively and efficiently. UNSOM/Stabilization: commended the stabilization efforts by partners around the country with the lead and coordination of MoIFAR. They highlighted how this meeting is important for the stakeholders to understand the stabilization interventions and challenges in the states since the last meeting. While appreciating the progress made in Lower Shabelle operations in terms of early recovery initiatives, UNSOM emphasized the need to think of long term interventions. AMISOM Head of Support provided a briefing that underscored the progress made in stabilization in Somalia as whole, and Lower Shabelle in particular. AMISOM commended the stabilization efforts especially community recovery projects implemented in Sabiid, Bariire and Awdheegle towns of Lower Shabelle as well as joint planning sand the PM’s visit to Marka as evidence of the current momentum.