University of Veterinary Medicine Hannover Diagnostic Approaches
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
FEWS Country Report BURKINA, CHAD, MALI, MAURITANIA, and NIGER
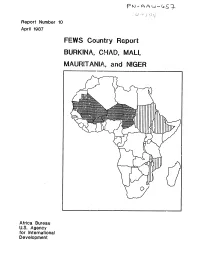
Report Number 10 April 1987 FEWS Country Report BURKINA, CHAD, MALI, MAURITANIA, and NIGER Africa Bureau U.S. Agency for International Development Summary Map __ Chad lMurltanl fL People displaced by fighting High percentage of population have bothL.J in B.E.T. un~tfood needsa nd no source of income - High crop oss cobied with WESTERN Definite increases in retes of malnutrition at CRS centers :rom scarce mrket and low SAHARA .ct 1985 through Nov 196 ,cash income Areas with high percentage MA RTAI of vulnerable LIBYA MAU~lAN~A/populations / ,,NIGER SENEGAL %.t'"S-"X UIDA Areas at-risk I/TGI IEI BurkinaCAMEROON Areas where grasshoppers r Less than 50z of food needs met combined / CENTRAL AFRICAN would have worst impact Fi with absence of government stocks REPLTL IC if expected irdestat ions occur W Less than r59 of food needs met combined ith absence of government stocks FEYIS/PWA. April 1987 Famine Early Warning System Country Report BURKINA CHAD MALI MAURITANIA NIGER Populations Under Duress Prepared for the Africa Bureau of the U.S. Agency for International Development Prepared by Price, Williams & Associates, Inc. April 1987 Contents Page i Introduction 1 Summary 2 Burkina 6 Chad 9 Mali 12 Mauritania 18 Niger 2f FiAures 3 Map 2 Burkina, Grain Supply and OFNACER Stocks 4 Table I Burkina, Production and OFNACER Stocks 6 Figure I Chad, Prices of Staple Grains in N'Djamcna 7 Map 3 Chad, Populations At-Risk 10 Table 2 Mali, Free Food Distribution Plan for 1987 II Map 4 Mali, Population to Receive Food Aid 12 Figure 2 Mauritania, Decreasing -

Data-Driven Identification of Potential Zika Virus Vectors Michelle V Evans1,2*, Tad a Dallas1,3, Barbara a Han4, Courtney C Murdock1,2,5,6,7,8, John M Drake1,2,8
RESEARCH ARTICLE Data-driven identification of potential Zika virus vectors Michelle V Evans1,2*, Tad A Dallas1,3, Barbara A Han4, Courtney C Murdock1,2,5,6,7,8, John M Drake1,2,8 1Odum School of Ecology, University of Georgia, Athens, United States; 2Center for the Ecology of Infectious Diseases, University of Georgia, Athens, United States; 3Department of Environmental Science and Policy, University of California-Davis, Davis, United States; 4Cary Institute of Ecosystem Studies, Millbrook, United States; 5Department of Infectious Disease, University of Georgia, Athens, United States; 6Center for Tropical Emerging Global Diseases, University of Georgia, Athens, United States; 7Center for Vaccines and Immunology, University of Georgia, Athens, United States; 8River Basin Center, University of Georgia, Athens, United States Abstract Zika is an emerging virus whose rapid spread is of great public health concern. Knowledge about transmission remains incomplete, especially concerning potential transmission in geographic areas in which it has not yet been introduced. To identify unknown vectors of Zika, we developed a data-driven model linking vector species and the Zika virus via vector-virus trait combinations that confer a propensity toward associations in an ecological network connecting flaviviruses and their mosquito vectors. Our model predicts that thirty-five species may be able to transmit the virus, seven of which are found in the continental United States, including Culex quinquefasciatus and Cx. pipiens. We suggest that empirical studies prioritize these species to confirm predictions of vector competence, enabling the correct identification of populations at risk for transmission within the United States. *For correspondence: mvevans@ DOI: 10.7554/eLife.22053.001 uga.edu Competing interests: The authors declare that no competing interests exist. -

Appraisal Report
AFRICAN DEVELOPMENT FUND MAU/PAAL/2000/01 Language: English Original: French APPRAISAL REPORT LIVESTOCK DEVELOPMENT AND RANGE MANAGEMENT ISLAMIC REPUBLIC OF MAURITANIA NB: This document contains errata or corrigenda (see Annexes) COUNTRY DEPARTMENT OCDN NORTH REGION SEPTEMBER 2000 SCCD : N.G. TABLE OF CONENTS Page PROJECT BRIEF, EXECUTIVE SUMMARY, PROJECT MATRIX, CURRENCY i-ix EQUIVALENTS, LIST OF ABBREVIATIONS, LIST OF TABLES, LIST OF ANNEXES, COMPARATIVE SOCIO-ECONOMIC INDICATORS 1. ORIGIN AND PROJECT BACKGROUND 1 2. THE AGRICULTURAL SECTOR 1 2.1 Main Features 1 2.2 Natural Resources and Products 2 2.3 Land Tenure System 2 2.4 Rural Poverty 2 3. THE LIVESTOCK SUB-SECTOR 3 3.1 Importance of the Sub-Sector 3 3.2 Livestock Systems 3 3.3 Institutions of Sub-sector 4 3.4 Sub-sector Constraints 6 3.5 Government Policy and Strategy 7 3.6 Donor Interventions 7 4. THE PROJECT 8 4.1 Project Design and Rationale 8 4.2 Project Impact Area and Beneficiaries 8 4.3 Strategic Context 9 4.4 Project Objective 9 4.5 Project Description 9 4.6 Production, Marketing and Prices 13 4.7 Environmental Impact 13 4.8 Project Costs 14 4.9 Sources of Finance 15 5. PROJECT IMPLEMENTATION 16 5.1 Executing Agency 16 5.2 Institutional Provisions 18 5.3 Implementation and Supervision Schedule 19 5.4 Provisions Relating to the Procurement of Goods and Services 19 5.5 Provisions Relating to Disbursement 21 5.6 Monitoring and Evaluation 21 5.7 Financial Statements and Audit 22 5.8 Aid Coordination 22 TABLE OF CONTENTS (cont’d) Page 6. -

2020 Taxonomic Update for Phylum Negarnaviricota (Riboviria: Orthornavirae), Including the Large Orders Bunyavirales and Mononegavirales
Archives of Virology https://doi.org/10.1007/s00705-020-04731-2 VIROLOGY DIVISION NEWS 2020 taxonomic update for phylum Negarnaviricota (Riboviria: Orthornavirae), including the large orders Bunyavirales and Mononegavirales Jens H. Kuhn1 · Scott Adkins2 · Daniela Alioto3 · Sergey V. Alkhovsky4 · Gaya K. Amarasinghe5 · Simon J. Anthony6,7 · Tatjana Avšič‑Županc8 · María A. Ayllón9,10 · Justin Bahl11 · Anne Balkema‑Buschmann12 · Matthew J. Ballinger13 · Tomáš Bartonička14 · Christopher Basler15 · Sina Bavari16 · Martin Beer17 · Dennis A. Bente18 · Éric Bergeron19 · Brian H. Bird20 · Carol Blair21 · Kim R. Blasdell22 · Steven B. Bradfute23 · Rachel Breyta24 · Thomas Briese25 · Paul A. Brown26 · Ursula J. Buchholz27 · Michael J. Buchmeier28 · Alexander Bukreyev18,29 · Felicity Burt30 · Nihal Buzkan31 · Charles H. Calisher32 · Mengji Cao33,34 · Inmaculada Casas35 · John Chamberlain36 · Kartik Chandran37 · Rémi N. Charrel38 · Biao Chen39 · Michela Chiumenti40 · Il‑Ryong Choi41 · J. Christopher S. Clegg42 · Ian Crozier43 · John V. da Graça44 · Elena Dal Bó45 · Alberto M. R. Dávila46 · Juan Carlos de la Torre47 · Xavier de Lamballerie38 · Rik L. de Swart48 · Patrick L. Di Bello49 · Nicholas Di Paola50 · Francesco Di Serio40 · Ralf G. Dietzgen51 · Michele Digiaro52 · Valerian V. Dolja53 · Olga Dolnik54 · Michael A. Drebot55 · Jan Felix Drexler56 · Ralf Dürrwald57 · Lucie Dufkova58 · William G. Dundon59 · W. Paul Duprex60 · John M. Dye50 · Andrew J. Easton61 · Hideki Ebihara62 · Toufc Elbeaino63 · Koray Ergünay64 · Jorlan Fernandes195 · Anthony R. Fooks65 · Pierre B. H. Formenty66 · Leonie F. Forth17 · Ron A. M. Fouchier48 · Juliana Freitas‑Astúa67 · Selma Gago‑Zachert68,69 · George Fú Gāo70 · María Laura García71 · Adolfo García‑Sastre72 · Aura R. Garrison50 · Aiah Gbakima73 · Tracey Goldstein74 · Jean‑Paul J. Gonzalez75,76 · Anthony Grifths77 · Martin H. Groschup12 · Stephan Günther78 · Alexandro Guterres195 · Roy A. -

Pastoralism and Security in West Africa and the Sahel
Pastoralism and Security in West Africa and the Sahel Towards Peaceful Coexistence UNOWAS STUDY 1 2 Pastoralism and Security in West Africa and the Sahel Towards Peaceful Coexistence UNOWAS STUDY August 2018 3 4 TABLE OF CONTENTS Abbreviations p.8 Chapter 3: THE REPUBLIC OF MALI p.39-48 Acknowledgements p.9 Introduction Foreword p.10 a. Pastoralism and transhumance UNOWAS Mandate p.11 Pastoral Transhumance Methodology and Unit of Analysis of the b. Challenges facing pastoralists Study p.11 A weak state with institutional constraints Executive Summary p.12 Reduced access to pasture and water Introductionp.19 c. Security challenges and the causes and Pastoralism and Transhumance p.21 drivers of conflict Rebellion, terrorism, and the Malian state Chapter 1: BURKINA FASO p.23-30 Communal violence and farmer-herder Introduction conflicts a. Pastoralism, transhumance and d. Conflict prevention and resolution migration Recommendations b. Challenges facing pastoralists Loss of pasture land and blockage of Chapter 4: THE ISLAMIC REPUBLIC OF transhumance routes MAURITANIA p.49-57 Political (under-)representation and Introduction passivity a. Pastoralism and transhumance in Climate change and adaptation Mauritania Veterinary services b. Challenges facing pastoralists Education Water scarcity c. Security challenges and the causes and Shortages of pasture and animal feed in the drivers of conflict dry season Farmer-herder relations Challenges relating to cross-border Cattle rustling transhumance: The spread of terrorism to Burkina Faso Mauritania-Mali d. Conflict prevention and resolution Pastoralists and forest guards in Mali Recommendations Mauritania-Senegal c. Security challenges and the causes and Chapter 2: THE REPUBLIC OF GUINEA p.31- drivers of conflict 38 The terrorist threat Introduction Armed robbery a. -

Genetic and Phylogenetic Characterization Of
Article Genetic and Phylogenetic Characterization of Tataguine and Witwatersrand Viruses and Other Orthobunyaviruses of the Anopheles A, Capim, Guamá, Koongol, Mapputta, Tete, and Turlock Serogroups Alexey M. Shchetinin 1, Dmitry K. Lvov 1, Petr G. Deriabin 1, Andrey G. Botikov 1, Asya K. Gitelman 1, Jens H. Kuhn 2 and Sergey V. Alkhovsky 1,* Received: 2 September 2015; Accepted: 7 November 2015; Published: 23 November 2015 Academic Editors: Jane Tao and Pierre-Yves Lozach 1 D.I. Ivanovsky Institute of Virology, Gamaleya Federal Research Center for Epidemiology and Microbiology, Ministry of Health of the Russian Federation, 123098, Moscow, Russia; [email protected] (A.M.S.); [email protected] (D.K.L.); [email protected] (P.G.D.); [email protected] (A.G.B.); [email protected] (A.K.G.) 2 Integrated Research Facility at Fort Detrick, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Fort Detrick, Frederick, MD 21702, USA; [email protected] * Correspondence: [email protected]; Tel.: +7-499-190-3043; Fax: +7-499-190-2867 Abstract: The family Bunyaviridae has more than 530 members that are distributed among five genera or remain to be classified. The genus Orthobunyavirus is the most diverse bunyaviral genus with more than 220 viruses that have been assigned to more than 18 serogroups based on serological cross-reactions and limited molecular-biological characterization. Sequence information for all three orthobunyaviral genome segments is only available for viruses belonging to the Bunyamwera, Bwamba/Pongola, California encephalitis, Gamboa, Group C, Mapputta, Nyando, and Simbu serogroups. Here we present coding-complete sequences for all three genome segments of 15 orthobunyaviruses belonging to the Anopheles A, Capim, Guamá, Kongool, Tete, and Turlock serogroups, and of two unclassified bunyaviruses previously not known to be orthobunyaviruses (Tataguine and Witwatersrand viruses). -

The United States Army Medical Department
THE UNITED STATES ARMY MEDICAL DEPARTMENT OURNAL THE MULTIDISCIPLINARY ASPECTS OF PUBLIC HEALTH January-June 2018 FirstJ Record of Aedes (Stegomyia) malayensis Colless (Diptera: Culicidae) in the Lao People’s Democratic Republic, Based on Morphological Diagnosis and Molecular Analysis 1 Maysa T. Motoki, PhD; Elliott F. Miot, MS; Leopoldo M. Rueda, PhD; et al Mosquito Surveillance Conducted by US Military Personnel in the Aftermath of the Nuclear Explosion at Nagasaki, Japan, 1945 8 David B. Pecor, BS; Desmond H. Foley, PhD; Alexander Potter Georgia’s Collaborative Approach to Expanding Mosquito Surveillance in Response to Zika Virus: Year Two 14 Thuy-Vi Nguyen, PhD, MPH; Rosmarie Kelly, PhD, MPH; et al An Excel Spreadsheet Tool for Exploring the Seasonality of Aedes Vector Hazard for User-Specified Administrative Regions of Brazil 22 Desmond H. Foley, PhD; David B. Pecor, BS Surveillance for Scrub Typhus, Rickettsial Diseases, and Leptospirosis in US and Multinational Military Training Exercise Cobra Gold Sites in Thailand 29 Piyada Linsuwanon, PhD; Panadda Krairojananan, PhD; COL Wuttikon Rodkvamtook, PhD, RTA; et al Risk Assessment Mapping for Zoonoses, Bioagent Pathogens, and Vectors at Edgewood Area, Aberdeen Proving Ground, Maryland 40 Thomas M. Kollars, Jr, PhD; Jason W. Kollars Optimizing Mission-Specific Medical Threat Readiness and Preventive Medicine for Service Members 49 COL Caroline A. Toffoli, VC, USAR Public Health Response to Imported Mumps Cases–Fort Campbell, Kentucky, 2018 55 LTC John W. Downs, MC, USA Developing Medical Surveillance Examination Guidance for New Occupational Hazards: The IMX-101 Experience 60 W. Scott Monks, MPAS, PA-C Missed Opportunities in Human Papillomavirus Vaccination Uptake Among US Air Force Recruits, 2009-2015 67 COL Paul O. -

World Bank Document
ReportNo. 12606-MAU Mauritania Country EnvironmentalStrategy Paper Public Disclosure Authorized June30, 1994 Africa Region Sahelian Departnient Public Disclosure Authorized U Public Disclosure Authorized Documentof the World Bank Public Disclosure Authorized I ABBREVIATIONS AND ACRONYMS AMEXTIPE Mauritanian Agency for Public Works AgenceMauritanienne d'Execution des and Employment Travauxdlnteret Publicet pour l'Emploi CESP CountryEnvironumental Strategy Paper Documentde Strategie Environnementale CNEA NationalCenter for AlternativeEnergy Cellule Nationale des Energies Alternatives DEAR Departmentof Environmentand Rural Direction de lEnvironnement et de Planning l'Am6nagementRural EC EuropeanCommunity CommunauteEuropeene GEF GlobalEnvironment Facility Fondspour l'EnvironnementMondial IUCN WorldConservation Union Union Mondialepour la Nature LPG LiquidPropane Gas MDRE Ministry of Rural Development and Minist&re du Developpement et de Envirorunent l'Environnement MHE Ministryof Water and Energy Ministere de lHydraulique et de lEnergie MS Ministryof Health Ministerede la Sante NEAP NationalEnvironmental Action Plan Plan dAction National pour l'Environnement NRM Natural ResourceManagement Gestiondes RessourcesNaturelles OMVS Organization for the Development of Organisation pour la Mise en Valeur the SenegalRiver Valley du FleuveSenegal PAs PastoralAssociations AssociationsPastorales UNCED United Nations Conference on Environmentand Development UNDP United Nations Development Programmedes Nations Unies pour la Programme Developpement UNSO -

Mauritania's Campaign of Terror: State-Sponsored Repression of Black Africans
MAURITANIA'S CAMPAIGN OF TERROR State-Sponsored Repression of Black Africans Human Rights Watch/Africa (formerly Africa Watch) Human Rights Watch New York $ Washington $ Los Angeles $ London Copyright 8 April 1994 by Human Rights Watch All rights reserved. Printed in the United States of America. Library of Congress Catalog Card Number: 94-75822 ISBN: 1-56432-133-9 Human Rights Watch/Africa (formerly Africa Watch) Human Rights Watch/Africa is a non-governmental organization established in 1988 to monitor promote the observance of internationally recognized human rights in Africa. Abdullahi An- Na'im is the director; Janet Fleischman is the Washington representative; Karen Sorensen, Alex Vines, and Berhane Woldegabriel are research associates; Kimberly Mazyck and Urmi Shah are associates; Bronwen Manby is a consultant. William Carmichael is the chair of the advisory committee and Alice Brown is the vice-chair. ACKNOWLEDGEMENTS This report was written by Janet Fleischman, Washington representative of Human Rights Watch/Africa. It is based on three fact-finding missions to Senegal - - in May-June 1990, February-March 1991, and October-November 1993 -- as well as numerous interviews conducted in Paris, New York, and Washington. Human Rights Watch/Africa gratefully acknowledges the following staff members who assisted with editing and producing this report: Abdullahi An-Na'im; Karen Sorensen; and Kim Mazyck. In addition, we would like to thank Rakiya Omaar and Alex de Waal for their contributions. Most importantly, we express our sincere thanks to the many Mauritanians, most of whom must remain nameless for their own protection and that of their families, who provided invaluable assistance throughout this project. -
Food Insecurity and Complex Emergency
FACT SHEET #16, FISCAL YEAR (FY) 2012 SEPTEMBER 14, 2012 SAHEL – FOOD INSECURITY AND COMPLEX EMERGENCY KEY DEVELOPMENTS In general, food security conditions in most of the Sahel have stabilized and are expected to improve to No Acute Food Insecurity—Integrated Food Security Phase Classification (IPC) 1—in October and November, according to the USAID-funded Famine Early Warning Systems Network (FEWS NET). Nonetheless, FEWS NET notes that ongoing flooding and increasing numbers of desert locusts remain significant threats and could reduce this year’s agricultural production in some areas. Continuing insecurity and related displacement could also prompt above- average food assistance needs in Burkina Faso, Mali, Mauritania, and Niger in early 2013. To date, floods—resulting from heavy seasonal rains in parts of the Sahel—have affected or displaced approximately 21,000 people throughout Burkina Faso, 25,000 people in northern Cameroon, 500,000 people in Chad, 9,000 people in Mali, and 527,000 people in Niger, according to international media and relief agency sources. In Senegal, flooding triggered by severe rainfall since mid-August has affected more than 260,000 people, according to a recent U.N. rapid assessment of the country’s flooded areas. On September 13, U.S. Ambassador Lewis A. Lukens declared a disaster due to the effects of the floods. In response, USAID’s Office of U.S. Foreign Disaster Assistance (USAID/OFDA) is providing $50,000 to Catholic Relief Services (CRS) for flood-relief activities in affected communities, including a hygiene awareness campaign and the provision of supplies such as mosquito nets, boots, and pumps to help remove standing water. -

Data-Driven Identification of Potential Zika Virus Vectors Michelle V Evans1,2*, Tad a Dallas1,3, Barbara a Han4, Courtney C Murdock1,2,5,6,7,8, John M Drake1,2,8
RESEARCH ARTICLE Data-driven identification of potential Zika virus vectors Michelle V Evans1,2*, Tad A Dallas1,3, Barbara A Han4, Courtney C Murdock1,2,5,6,7,8, John M Drake1,2,8 1Odum School of Ecology, University of Georgia, Athens, United States; 2Center for the Ecology of Infectious Diseases, University of Georgia, Athens, United States; 3Department of Environmental Science and Policy, University of California-Davis, Davis, United States; 4Cary Institute of Ecosystem Studies, Millbrook, United States; 5Department of Infectious Disease, University of Georgia, Athens, United States; 6Center for Tropical Emerging Global Diseases, University of Georgia, Athens, United States; 7Center for Vaccines and Immunology, University of Georgia, Athens, United States; 8River Basin Center, University of Georgia, Athens, United States Abstract Zika is an emerging virus whose rapid spread is of great public health concern. Knowledge about transmission remains incomplete, especially concerning potential transmission in geographic areas in which it has not yet been introduced. To identify unknown vectors of Zika, we developed a data-driven model linking vector species and the Zika virus via vector-virus trait combinations that confer a propensity toward associations in an ecological network connecting flaviviruses and their mosquito vectors. Our model predicts that thirty-five species may be able to transmit the virus, seven of which are found in the continental United States, including Culex quinquefasciatus and Cx. pipiens. We suggest that empirical studies prioritize these species to confirm predictions of vector competence, enabling the correct identification of populations at risk for transmission within the United States. *For correspondence: mvevans@ DOI: 10.7554/eLife.22053.001 uga.edu Competing interests: The authors declare that no competing interests exist. -

Sahel Food Security and Complex Emergency
FACT SHEET #17, FISCAL YEAR (FY) 2012 SEPTEMBER 30, 2012 SAHEL – FOOD INSECURITY AND COMPLEX EMERGENCY This is the final Sahel fact sheet for FY 2012. KEY DEVELOPMENTS Nearly one year since the onset of the food insecurity and nutrition crisis in the Sahel, food security conditions have stabilized and are expected to improve to No Acute Food Insecurity—Integrated Food Security Phase Classification (IPC) 1—in most areas by November due in part to positive agricultural production forecasts, according to the USAID-funded Famine Early Warning Systems Network (FEWS NET). Nonetheless, FEWS NET notes that recent flooding and increasing numbers of desert locusts remain significant threats and could reduce this year’s agricultural output in some areas. Ongoing insecurity in Mali and related displacement could also result in continuing above- average humanitarian assistance needs in parts of Burkina Faso, Mali, Mauritania, and Niger through late 2012. The rate at which Malians are fleeing to neighboring countries recently slowed, according to the Office of the U.N. High Commissioner for Refugees (UNHCR). In August, the number of new arrivals in Burkina Faso, Mauritania, and Niger declined by 61 percent compared to the preceding month, decreasing from an estimated 60,000 people per month to approximately 23,500 people per month. In mid-September, the Mali Protection Cluster—the coordinating body for humanitarian protection activities in the country—revised the estimated number of internally displaced persons (IDPs) in Mali from 174,000 to 118,795, reflecting a decrease of 32 percent. Due to access challenges in the north, the new estimates may not represent the full number of IDPs in Mali, and the cluster continues working to obtain a more comprehensive count of IDPs.