Pathology of the Skin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Inflammatory Skin Disease Every Pathologist Should Know
Inflammatory skin disease every pathologist should know Steven D. Billings Cleveland Clinic [email protected] General Concepts • Pattern recognition – Epidermal predominant vs. dermal predominant • Epidermal changes trump dermal changes – Distribution of the inflammatory infiltrate • Superficial vs. superficial and deep • Location: perivascular, interstitial, nodular – Nature of inflammatory infiltrate • Mononuclear (lymphocytes and histiocytes) • Mixed (mononuclear and granulocytes) • Granulocytic • Correlation with clinical presentation • Never diagnose “chronic nonspecific dermatitis” Principle Patterns: Epidermal Changes Predominant • Spongiotic pattern • Psoriasiform pattern – Spongiotic and psoriasiform often co-exist • Interface pattern – Basal vacuolization • Perivascular infiltrate or • Lichenoid infiltrate Principle Patterns: Dermal Changes Predominant • Superficial perivascular • Superficial and deep perivascular • Interstitial pattern – Palisading granulomatous – Nodular and diffuse • Sclerosing pattern • Panniculitis • Bullous disease • Miscellaneous Spongiotic Dermatitis • Three phases – Acute – Subacute – Chronic • Different but overlapping histologic features Spongiotic Dermatitis • Acute spongiotic dermatitis – Normal “basket-weave” stratum corneum – Pale keratinocytes – Spongiosis – Spongiotic vesicles (variable) – Papillary dermal edema – Variable superficial perivascular infiltrate of lymphocytes often with some eosinophils – Rarely biopsied in acute phase Spongiotic Dermatitis • Subacute spongiotic dermatitis – Parakeratosis -

ECZEMA) Shankar Pratap K
Research Article International Ayurvedi c Medical Journal ISSN:2320 5091 A HISTOPATHOLOGICAL STUDY ON LEECH APPLICATION IN THE MANAGEMENT OF VICARCIKA (ECZEMA) Shankar Pratap K. M.1 Rao Dattatreya 2 Sai Prasad 3 1Dept. of Shalya Tantra , Santhigiri Ayurvedic College , Palakkad, Kerala, India 2Dept. of Shalya Tantra, S.V. Ayurvedic College, Tirupati , Andhra Pradesh , India 3Dept. of Pathology, S. V. Medical College, Tirupati, Andhra Pradesh, India ABSTRACT To assess the efficacy of Leech application in the management of Vicarcik a (Eczema) with Histopathological study, the present study with 10 patients having the classical symptoms of Vicarcika, were randomly selected as per the inclusion and exclusion criteria from O.P.D. & I.P.D. sections of Shalya department, S.V. Ayurvedic Hospital, Tirupati. Minimum 4 sittings of Leech application was carried out with seven days interval. Total duration of treatment was 6 weeks. Biopsy samples were collected from the lesion site before and after treatment. Histopathological examination was done by the pathologist. In eczema (dermatitis) the leech application therapy gives excellent response by reducing the inflammatory component, hyperkeratosis, spongiosis, irregular acanthosis and by evoking a granulation tissue response in the dermis and in most of the cases with complete recovery from the lesion. Most of the cases in the study were chronic dermatitis and sebhoric keratosis, almost all local/focal pigmented lesion is totally relieved by leech therapy especially in cases of sebhoric keratos is. In the present study it was found that, leech application evokes significant changes at histological level specifically in reduction of inflammatory component, hyperkeratosis, spongiosis and irregular acanthosis. -
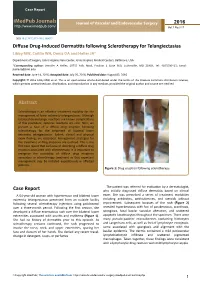
Diffuse Drug-Induced Dermatitis Following Sclerotherapy for Telangiectasias Libby MW, Caitlin WH, Deniz OA and Heller JA*
Case Report iMedPub Journals Journal of Vascular and Endovascular Surgery 2016 http://www.imedpub.com/ Vol.1 No.3:17 DOI: 10.21767/2573-4482.100017 Diffuse Drug-Induced Dermatitis following Sclerotherapy for Telangiectasias Libby MW, Caitlin WH, Deniz OA and Heller JA* Department of Surgery, Johns Hopkins Vein Center, Johns Hopkins Medical Centers, Baltimore, USA *Corresponding author: Jennifer A Heller, 10755 Falls Road, Pavilion 1 Suite 360, Lutherville, MD 21903, Tel: 4105500415; Email: [email protected] Received date: June 14, 2016; Accepted date: July 26, 2016; Published date: August 02, 2016 Copyright: © 2016 Libby MW, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Sclerotherapy is an effective treatment modality for the management of lower extremity telangiectasias. Although localized dermatologic reactions are known complications of this procedure, systemic reactions are rare. Here, we present a case of a diffuse drug eruption following sclerotherapy for the treatment of bilateral lower extremity telangiectasias. Salient clinical and physical exam findings are described. Management strategies for the treatment of drug eruptions are outlined. This is the first case report that we know of describing a diffuse drug eruption associated with sclerotherapy. It is important to recognize the possibility of diffuse drug eruptions secondary to sclerotherapy treatment so that expectant management may be initiated expeditiously in affected patients. Figure 1: Drug eruption following sclerotherapy. The patient was referred for evaluation by a dermatologist, Case Report who initially diagnosed diffuse dermatitis based on clinical A 64-year-old woman with hypertension and bilateral lower exam. -

JMSCR Vol||07||Issue||03||Page 281-286||March 2019
JMSCR Vol||07||Issue||03||Page 281-286||March 2019 www.jmscr.igmpublication.org Index Copernicus Value: 79.54 ISSN (e)-2347-176x ISSN (p) 2455-0450 DOI: https://dx.doi.org/10.18535/jmscr/v7i3.51 Histopathological Evaluation of Collagen Profiles in Spongiotic Dermatitis Authors Anjali Patankar, Ramya Gandhi*, Erli Amel Ivan Department of Pathology, Sri Manakula Vinayagar Medical College and Hospital, Kalitheerthalkuppam, Puducherry, 605 107 India *Corresponding Author Dr Ramya Gandhi Associate Professor, Department of Pathology, Sri Manakula Vinayagar Medical College and Hospital, Kalitheerthalkuppam, Puducherry, 605 107, India Email: [email protected], Mobile no- 9787740891 Abstract Context: Spongiotic Dermatitis is a common clinical condition also known as eczema, characterized by rashes and itching further may progress to scarring. The terms eczema and dermatitis are often used interchangeably to denote a polymorphic inflammatory reaction pattern involving the epidermis and dermis. Spongiosis refers to intraepidermal edema. Aim: To assess the orientation of collagen in eczematous spongiotic dermatitis. Material and Methods: The present study was done in the Department of Pathology, Sri Manakula Vinayagar Medical College, Pondicherry. Sixty diagnosed cases of spongiotic dermatitis diagnosed over a period of five years were taken in the study. Orientation of collagen was evaluated using Masson’s trichrome stain. Results: Spongiotic dermatitis occurred in all age groups but commonly seen in middle age to elderly. Male to female ratio was 1:1.2 The most common symptom was itching (85%) followed by scaling (63.3%). Most common site was upper extremities (80%). subacute cases were predominantly seen (38.3%) followed by chronic cases (33.3%). -

Review of the Literature
Review Clinical and Histopathological Features and Potential Pathological Mechanisms of Skin Lesions in COVID-19: Review of the Literature Gürkan Kaya 1,*, Aysin Kaya 2 and Jean-Hilaire Saurat 2 1 Departments of Dermatology and Clinical Pathology, University Hospital of Geneva, 1205 Geneva, Switzerland 2 Department of Clinical Pharmacology and Toxicology, University of Geneva, 1205 Geneva, Switzerland; [email protected] (A.K.); [email protected] (J.-H.S.) * Correspondence: [email protected] Received: 24 June 2020; Accepted: 29 June 2020; Published: 30 June 2020 Abstract: In recent weeks, several reports have emerged of skin lesions with different clinical presentations in COVID-19 cases. All dermatologists should be aware of these cutaneous lesions, which may be early clinical symptoms of infection. We reviewed the literature on cutaneous manifestations in the PubMed database from December 2019 and June 2020. From the cases described as case reports or series in 57 recent articles, it appears that skin lesions (i) are highly varied, (ii) may not be related to the severity of the condition and (iii) resolve spontaneously in a few days. The frequency of these lesions in COVID-19 patients varies between 1.8% and 20.4%. The major clinical forms described were maculopapular eruptions, acral areas of erythema with vesicles or pustules (pseudochilblain), urticarial lesions, other vesicular eruptions and livedo or necrosis. The lesions were mainly localized in the trunk and extremities. The majority of patients were male, aged between 4.5 and 89 years. A minority of the patients were children presenting with acral, chilblain-like lesions, papulo-vesicular eruptions or Kawasaki disease-like pediatric inflammatory multisystem syndrome. -

Fig. 1. Lentigo Simplex. Elongated Rete Ridges, Hyperpigmentation of The
97 Fig. 1. Lentigo simplex. Elongated rete ridges, hyperpigmentation of the basal layer and increase in number of enlarged melanocytes arranged singly along the basal layer Fig. 2. Junctional melanocytic naevus. Nests of melanocytes are present at the dermo-epidermal junction, predominantly at the bases of elongated rete ridges 98 a b Fig.3a,b. Compound melanocytic naevus. a Nests of melanocytes in the dermis as well as the derma-epidermal junction, smaller and more diffusely arranged in the deeper dermis. b The nests of melanocytes include multinucleated giant cells 99 Fig. 4. Dermal melanocytic naevus. Entirely intradermal tumour in a nested pattern in the superficial layers, composed of small naevoid melanocytes in the deep dermis Fig. 5. Dermal melanocytic naevus. The deeper layers of this dermal melanocytic naevus include neuroid structures similar to Wagner-Meissner corpuscles (neuroid dermal melanocytic naevus) 100 Fig. 6. Balloon cell naevus. The tumour is composed mainly of melanocytes with abundant clear cytoplasm and central nuclei Fig. 7. Halo naevus. Compound naevus with a dense lymphocytic infiltrate between the naevoid melanocytes of the dermal component Fig. 8. Combined intradermal naevus and blue naevus. Nests of epithelioid naevus cells in the dermis (right) and heavily pigmented spindle and dendritic cells arranged between collagen bundles in the adjacent stroma (left) Fig. 9a. Deep penetrating naevus. A wedge-shaped lesion composed of irregu lar collections of variably pigmented cells extending into the deep dermis. 102 Fig. 9b. Deep penetrating naevus. In the deep dermis the lesion includes large cells with nuclear pseudo-inclusions, smaller naevoid melanocytes and groups of melanophages in the intervening stroma Fig. -

The Best Diagnosis Is: A
DERMATOPATHOLOGY DIAGNOSIS H&E, original magnification ×40. The best diagnosis is: a. lichen striatus copy b. linear epidermolytic hyperkeratosis c. linear lichen planus d. linear porokeratosisnot e. linear psoriasis Do A H&E, original magnification ×CUTIS40. B H&E, original magnification ×200 for both. PLEASE TURN TO PAGE 120 FOR DERMATOPATHOLOGY DIAGNOSIS DISCUSSION Jacqueline N. Graham, BS; Eric W. Hossler, MD Ms. Graham is from Northeast Ohio Medical University, Rootstown. Dr. Hossler is from the Departments of Dermatology and Pathology, Geisinger Medical Center, Danville, Pennsylvania. The authors report no conflict of interest. Correspondence: Jacqueline N. Graham, BS, 4249 Pine Dr, Rootstown, OH 44272 ([email protected]). 86 CUTIS® WWW.CUTIS.COM Copyright Cutis 2015. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. Dermatopathology Diagnosis Discussion Lichen Striatus ichen striatus (LS) is a benign, uncommon, self-limited, linear inflammatory skin disorder Lthat primarily affects children up to 15 years of age, most commonly around 2 to 3 years of age, and is seen more frequently in girls.1 It presents with a sudden eruption of asymptomatic small, flat- topped, lichenoid, scaly papules in a linear array on a single extremity. The lesions may be erythematous, flesh colored, or hypopigmented.1,2 Multiple lesions appear over days to weeks and coalesce into linear plaques in a continuous or interrupted pattern along the lines of Blaschko, indicating possible -

WSC 14-15 Conf 7 Layout
Joint Pathology Center Veterinary Pathology Services WEDNESDAY SLIDE CONFERENCE 2014-2015 Conference 7 22 October 2014 CASE I: B13-962 (JPC 4049563). performed at that time. The dog presented again in July 2013 with continued hematuria. On Signalment: 10-year-old spayed female Welsh ultrasound, the left renal cortex had a 2.2 cm, corgi dog, Canis familiaris. round, heterogeneous mass with multiple, internal, anechoic regions. History: The dog presented in 2011 for a 6-week history of hematuria. Urine culture was negative Gross Pathology: The renal cortex was and no signs of uroliths were seen on radiographs. extensively disrupted by coalescing, dark red, Ultrasound revealed two, 1.7 mm, mineralized blood-filled nodules ranging from 0.7 x 0.5 x 0.2 foci in the left renal pelvis, but the kidneys were cm to 2.5 x 2 x 2 cm. normal in shape and size. No further workup was Histopathologic Description: Kidney: The renal interstitium is markedly expanded by many, severely dilated, blood-filled vascular spaces lined by mature endothelial cells surrounded by abundant fibrous tissue. Some vascular spaces contain thrombi with fibrin arranged as lines of Zahn separated by red and white blood cells that are occasionally attached to the vascular wall by fibrous tissue. The intervening and adjacent renal parenchyma is markedly atrophic with replacement of many nephrons by fibrosis, many lymphocytes and plasma cells, and variable 1-1. Kidney, Welsh corgi: The cortex is expanded by large, ectatic, thin-walled vessels which efface renal parenchyma. (HE 6.3X) hemorrhage. Remaining tubules 1 WSC 2014-2015 1-2. -

Plasma Cell Gingivitis
Plasma Cell Gingivitis C. Román Curto, MD; M. Yuste Chaves, MD; A. González Morán, MD; P. González Asensio, MD; G. López, MD Plasma cell gingivitis (PCG), an infrequent benign inflammatory condition of unknown etiology, is a type of plasma cell orificial mucositis, which includes a wide spectrum of conditions. We pre- sent the case of a 13-year-old girl who had PCG with an erythematous congestive plaque on the anterior maxillary gingiva for 4 years. Occasion- ally, the lesion became increasingly swollen and painful and bled. Results of a histopathologic examination showed dense plasmacytic infiltrate in the dermis, affecting the dermoepidermal bor- der, with immunohistochemical positivity in the and light chains and vascular proliferation. “Lozenge” keratinocytes, “watery” spongiosis, and exocytosis were seen in the epidermis. Figure 1. A bright red, slightly elevated plaque on the Laboratory analysis showed notably low levels of upper gum with a fine, whitish, superficial network. both serum IgA and secretory IgA. We consider whether secretory IgA at low levels has an impor- tant etiopathogenic role favoring the develop- Case Report ment of localized subclinical repetitive infections A 13-year-old girl without significant pathologic or that could lead to chronic PCG. dental history (other than the habit of chewing gum 2 or 3 times a week) had a bright red, congestive, lasma cell gingivitis (PCG) is a benign inflam- asymptomatic plaque on her upper gum for 4 years. matory condition that is uncommon (at least Occasionally and without any clear association with P in the dermatologic literature) and of unclear the girl’s menstrual cycle, the lesion became increas- etiology. -

Polymorphous Light Eruption
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Polymorphous Light Eruption Erhard Holzle, M.D., Gerd Plewig, M.D., Renate von Kries, M.D., Percy Lehmann, M.D. Department of Dermatology, University of Diisseldorf, Diisseldorf, F. R. G. Polymorphous light eruption (PLE) is a common photo cells, and spongiosis in the lower epidermis. The most dermatosis of unknown etiology. It affiicts mainly fair important differential diagnoses are solar urticaria, pho skinned patients, with a preponderance of young females. tosensitive erythema multiforme, and lupus erythemato There is, however, no absolute restriction as to age, sex, sus. or race. The action spectrum of PLE is under debate. Repro Clinical variants include the papular, vesiculo-bullous, duction of skin lesions has been reported with UVB, UV A, and hemorrhagic variety, as well as plaque, erythema mul and, rarely, visible light, with UVA probably being the tiforme-like, and insect bite (strophulus)-like types. Skin most effective part of the spectrum. lesions appear only in certain exposed areas hours or a few More important than treatment of PLE is prophylaxis. days after intense sunshine, and are nearly always mono UV A- and UVB-effective sunscreens are of some help. morphous in the same patient. The rash subsides sponta Phototherapy and especially photochemotherapy (psoralen neously within several days without leaving scars. + UVA; PUV A) offer effective ways to decrease light The histopathologic picture is characteristic and shows sensitivity. Systemic treatment with chloroquine or f3-car a perivascular lymphocytic inftltrate in the upper and mid otene has been disappointing. -
The Interface Reaction Pattern in the Skin: an Integrated Review of Clinical and Pathological Features☆,☆☆ Maria A
Human Pathology (2019) 91,86–113 www.elsevier.com/locate/humpath Current topics The interface reaction pattern in the skin: an integrated review of clinical and pathological features☆,☆☆ Maria A. Deschaine MD a, Julia S. Lehman MD a,b,⁎ aDepartment of Dermatology, Mayo Clinic, Rochester, MN 55905 bDepartment of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, MN 55905 Received 9 May 2019; revised 18 June 2019; accepted 20 June 2019 Keywords: Summary Not uncommonly, pathologists encounter biopsies displaying inflammation at the dermoepi- Interface; dermal junction and confronted with its numerous diagnostic possibilities. As with other inflammatory Lichenoid; dermatoses, the correct diagnosis relies on careful integration of clinical, laboratory, and histopathologi- Vacuolar; cal features. Knowledge of clinical aspects of these disorders is crucial, and at times, lack of training Inflammatory dermatoses in clinical dermatology can make clinicopathological correlation challenging for the pathologist. This re- view is organized following the classical classification of cell-poor (vacuolar) and cell-rich (lichenoid) interface processes. The various entities are described based on their clinical presentation along their clinical differential diagnosis followed by their histopathological features and pathological differential diagnosis. Our aim is to provide an updated, clinically relevant review that integrates nuanced clinical and pathological features, with an emphasis on clues that may help differentiate entities in the differential -

Boards' Fodder
boards’ fodder Oral Disease, Part 1 by Helena Pasieka, MD CLINICAL PATHOLOGY TREATMENT ASSOCIATIONS DEVELOPMENTAL CONDITIONS Fordyce Granules 1-2mm yellowish papules on buccal “Free” sebaceous glands. None indicated. mucosa and vermillion. Asymptomatic. Geographic Well-defined red patches on lateral & Psoriasiform mucositis. If symptoms, potent topical Tongue dorsal tongue with a serpiginous white steroids. border. Fissured Tongue Multiple grooves on dorsum of tongue. Numerous grooves on dorsum of None indicated. Melkerson-Rosenthal (“Scrotal tongue”) Asymptomatic. tongue. & Down syndrome. Occasionally in Cowden, pachyo- nychia congenita & acromegaly (in set- ting of macroglossia). Hairy Tongue Hair-like elongation of lengthening of Pronounced accumulation of para- Identification & cessation of cause Smoking, poor papillae on dorsum of tongue, espe- keratosis at tips of otherwise normal and if symptoms, scraping or hygiene, oxidizing cially in central area. filiform papillae. brushing tongue. mouthwashes, and hot beverages. Median Rhomboid Well-demarcated, diamond-shaped Loss of filiform papillae. Consistently Anticandidal treatment, such as Glossitis eroded area in midline of posterior dor- associated with candidiasis. clotrimazole troches or PO fluco- sal tongue. nazole. PERIODONTAL AND GINGIVAL DISEASE Necrotizing Necrosis and/or ulceration of the inter- Non-specific, as disease etiology is Debridement of necrotic areas, Ulcerative dental papillae “punched-out papillae”. bacteria from normal oral flora. oral hygiene instruction, and con- Gingivitis Painful and hemorrhagic. trol of pain. Desquamative Diffuse painful gingival erythema. Depends on the vesiculoerosive dis- Treatment directed at underlying Erosive lichen pla- Gingivitis Epithelium readily mechanically sloughs ease it represents. Biopsy for H&E + dx. Meticulous dental prophylaxis nus, cicatricial pem- leaving behind a smooth appearance. DIF should be performed.