Clomipramine Suppresses ACE2-Mediated SARS-Cov-2 Entry
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -
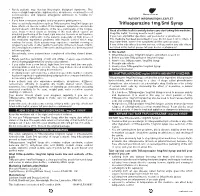
Trifluoperazine 1Mg/5Ml Syrup Can Trifluoperazine 1Mg/5Ml Syrup Have Effects on Muscle Control
• Rarely patients may develop Neuroleptic Malignant Syndrome. This causes a high temperature, rigid muscles, drowsiness, occasional loss of consciousness, and requires emergency admission to hospital for treatment. PATIENT INFORMATION LEAFLET • If you have chest pain (angina) and your pain is getting worse. • Very occasionally, medicines such as Trifluoperazine 1mg/5ml Syrup can Trifluoperazine 1mg/5ml Syrup have effects on muscle control. If this happens, symptoms can include slurred speech, odd movements of the face, particularly of the tongue, eyes, head or neck (such as twisting of the neck which causes an Read all of this leaflet carefully before you start taking this medicine. unnatural positioning of the head, rigid muscles, tremors or restlessness Keep this leaflet. You may need to read it again. and difficulty in sitting still). Some patients (especially on high doses of If you have any further questions, ask your doctor or pharmacist. this medicine) experience problems with muscle control which may This medicine has been prescribed for you. Do not pass it on to others. It continue for years. Such patients may experience constant chewing or may harm them, even if their symptoms are the same as yours. tongue movements or other gentle movements of the neck, head or trunk. If any of the side effects become serious, or if you notice any side effects Uncontrollable movements of the arms and legs have also been reported not listed in this leaflet, please tell your doctor or pharmacist. in these patients. In this leaflet: • Occasionally, some patients have complained of feeling slowed down, 1. What Trifluoperazine 1mg/5ml Syrup is and what it is used for whilst • Rarely, jaundice (yellowing of skin and whites of eyes), eye problems, 2. -

Opipramol and Trifluoperazine in the Treatment of Anxiety and Tension
A COMPARATIVE STUDY OF TWO ANTIHISTAMINES 395 In table VI are given the results of a question directed at discovering how effective the preferred treatment was compared to any other antihistamine used. Fifteen patients only were able to give this information but the results are interesting. Discussion TABLE VI The design of this study was very simple as COMPARISON WITH PREVIOUSLY USED ANTIHISTAMINE such studies must be if they are to be completed under the conditions of a busy general practice. In a condition such as hay fever where anti- Worse As good Better Total histamines are known to be etfective and where fairly rapid symptomatic relief is needed by the 2 4 9 15* patient, we did not feel justified in including a placebo. The results of the study seem fairly *In the majority of patients the previously used clear-cut that if patients are offered the choice antihistamine was the chemically related chlor- of a plain form of this antihistamine or a long- pheniramine maleate B.P. acting form more will choose the latter. Ofthose that do so, however, only about a third find a single tablet at night completely effective, the remainder have to take one further tablet during the day. Both forms of antihistamine are effective and where a retrospective comparison can be made this effectiveness is considered greater or equal to that of previously administered anti-histamines. Summary A simple comparative study under general-practice conditions of two formulations of pheniramine is described. Sixty-one per cent of patients preferred the long-acting form of this antihistamine. -

3,2,4 Tricyclic Antidepressants and the Risk of Congenital Malformation
Tricyclic antidepressants and the risk of congenital malformations CONFIDENTIAL Medicines Adverse Reactions Committee Meeting date 3/12/2020 Agenda item 3.2.4 Title Tricyclic antidepressants and the risk of congenital malformations Submitted by Medsafe Pharmacovigilance Paper type For advice Team Active ingredient Product name Sponsor Amitriptyline Arrow-Amitriptyline Film coated tablet, 10 mg, 25 Teva Pharm (NZ) Ltd mg & 50 mg Amirol Film coated tablet, 10 mg & 25 mg AFT Pharmaceuticals Ltd Clomipramine Apo-Clomipramine Film coated tablet, 10 mg & Apotex NZ Ltd 25 mg Anafranil Tablet, 10 mg Section 29 Dosulepin Dosulepin Mylan Film coated tablet, 75 mg Mylan New Zealand Ltd Dosulepin Mylan Capsule, 25 mg Section 29 Doxepin Anten 50 Capsule, 50 mg Mylan New Zealand Ltd Imipramine Tofranil Coated tablet, 10 mg & 25 mg AFT Pharmaceuticals Ltd Nortriptyline Norpress Tablet, 10 mg & 25 mg Mylan New Zealand Ltd PHARMAC funding Product highlighted in bold above are funded on the Community Schedule. Two products (shown in italics) are funded but only available under Section 29 of the Medicines Act (ie, the products have not been approved by Medsafe). Previous MARC In utero exposure to serotonin reuptake inhibitors and risk of congenital meetings abnormalities 141st meeting March 2010 International action None Prescriber Update The use of antidepressants in pregnancy September 2010 Classification Prescription medicine Usage data The following pregnancy usage data for 2019 was obtained from the National Collections using the Pharmaceutical Dispensing in Pregnancy application in Qlik. The table shows the total number of dispensings, repeat dispensings and number of pregnancies exposed during first trimester (defined as 30 days prior to the estimated pregnancy start date to week 13) for pregnancies that ended in 2019. -

Louisiana Fee-For-Service Medicaid Antipsychotics
Louisiana Fee-for-Service Medicaid Antipsychotics The Louisiana Uniform Prescription Drug Prior Authorization Form should be utilized to request: Authorization for non-preferred agents for recipients 6 years of age and older; AND Authorization for all preferred and non-preferred agents for recipients younger than 6 years of age; AND Authorization to exceed maximum daily dose/quantity limit for all ages. See full prescribing information for individual agents for details on the information below: *These agents have Black Box Warnings †These agents are subject to Risk Evaluation and Mitigation Strategy (REMS) under FDA safety regulations ‡ For long-acting injectable agents, it is required that the previous 60-day period of pharmacy claims show one of the following: Established tolerance to the oral formulation (as evidenced by a paid pharmacy claim for the oral formulation); OR Established therapy with the requested injectable agent (as evidenced by a paid pharmacy claim for the requested injectable agent) NOTE: Diagnosis code requirements apply to both preferred and non-preferred agents (see Table 1). Maximum daily dose edits (see Table 2), quantity limits (see Table 3), and other requirements at Point-of-Sale for select agents in this category may apply to both preferred and non-preferred agents. For additional information, see http://www.lamedicaid.com/provweb1/Pharmacy/pharmacyindex.htm. Oral Antipsychotics – Generic Name (Brand Example) * Amitriptyline/Perphenazine * Aripiprazole ODT; Oral Solution (Abilify®); Tablet (Abilify®) -

Promethazine-Chlorpromazine Combination in the Treatment of Unmanageable Psychotic Patients Armando R
Henry Ford Hospital Medical Journal Volume 17 | Number 4 Article 10 12-1969 Promethazine-Chlorpromazine Combination in the Treatment of Unmanageable Psychotic Patients Armando R. Favazza Follow this and additional works at: https://scholarlycommons.henryford.com/hfhmedjournal Part of the Chemicals and Drugs Commons, Life Sciences Commons, Medical Specialties Commons, Psychiatry and Psychology Commons, and the Public Health Commons Recommended Citation Favazza, Armando R. (1969) "Promethazine-Chlorpromazine Combination in the Treatment of Unmanageable Psychotic Patients," Henry Ford Hospital Medical Journal : Vol. 17 : No. 4 , 305-310. Available at: https://scholarlycommons.henryford.com/hfhmedjournal/vol17/iss4/10 This Article is brought to you for free and open access by Henry Ford Health System Scholarly Commons. It has been accepted for inclusion in Henry Ford Hospital Medical Journal by an authorized editor of Henry Ford Health System Scholarly Commons. Henry Ford Hosp. Med. Journal VoL 17, No. 4, 1969 Promethazine-chlorpromazine Combination in the Treatment of Unmanageable Psychotic Patients Armando R. Favazza, M.D.* Administering a combination of promethazine and chlorpromazine to patients with a "galloping psychosis" has an antipsychotic and tranquilizing effect which calms them down to a more manageable and less aggressive state. The drugs are chemically similar; promethazine's actions are strongly potentiated in the combina tion, so large doses must be given under careful supervision. Case histories demonstrate successful short term management of acutely psychotic, aggressive patients who were a danger to themselves and others. Acute, intense psychotic episodes common in the author's experience for can pose difficult problems for both some patients to receive massive doses the patient and those who care for him. -

Medications to Be Avoided Or Used with Caution in Parkinson's Disease
Medications To Be Avoided Or Used With Caution in Parkinson’s Disease This medication list is not intended to be complete and additional brand names may be found for each medication. Every patient is different and you may need to take one of these medications despite caution against it. Please discuss your particular situation with your physician and do not stop any medication that you are currently taking without first seeking advice from your physician. Most medications should be tapered off and not stopped suddenly. Although you may not be taking these medications at home, one of these medications may be introduced while hospitalized. If a hospitalization is planned, please have your neurologist contact your treating physician in the hospital to advise which medications should be avoided. Medications to be avoided or used with caution in combination with Selegiline HCL (Eldepryl®, Deprenyl®, Zelapar®), Rasagiline (Azilect®) and Safinamide (Xadago®) Medication Type Medication Name Brand Name Narcotics/Analgesics Meperidine Demerol® Tramadol Ultram® Methadone Dolophine® Propoxyphene Darvon® Antidepressants St. John’s Wort Several Brands Muscle Relaxants Cyclobenzaprine Flexeril® Cough Suppressants Dextromethorphan Robitussin® products, other brands — found as an ingredient in various cough and cold medications Decongestants/Stimulants Pseudoephedrine Sudafed® products, other Phenylephrine brands — found as an ingredient Ephedrine in various cold and allergy medications Other medications Linezolid (antibiotic) Zyvox® that inhibit Monoamine oxidase Phenelzine Nardil® Tranylcypromine Parnate® Isocarboxazid Marplan® Note: Additional medications are cautioned against in people taking Monoamine oxidase inhibitors (MAOI), including other opioids (beyond what is mentioned in the chart above), most classes of antidepressants and other stimulants (beyond what is mentioned in the chart above). -

Perphenazine Shortage
Perphenazine Shortage Perphenazine is currently only marketed by one company, AA Pharma Inc.1 DIN Company Brand Name Active ingredient Strength 00335096 AA PHARMA INC PERPHENAZINE PERPHENAZINE 16 MG 00335118 AA PHARMA INC PERPHENAZINE PERPHENAZINE 8 MG 00335126 AA PHARMA INC PERPHENAZINE PERPHENAZINE 4 MG 00335134 AA PHARMA INC PERPHENAZINE PERPHENAZINE 2 MG Perphenazine is a piperazine phenothiazine.2 Indications3: Psychotic disorders Nausea and vomiting Shortage management strategies: 1. Ensure medication is indicated. For example, first general antipsychotics should be avoided if possible in elderly patients.4 If no clear indication, consider tapering patient off the medication. 2. Therapeutic alternatives2,4: a) Phenothiazines are the most similar pharmacologic alternatives: CPE* Drug Psychotic Disorder: Nausea and Vomiting: (perphenazine Suggested Dose Suggested Dose = 10 mg) Initial dose: 25–75 mg daily in 2–4 divided doses. Daily dose may be ↑twice weekly by 25– 50 mg until symptoms are controlled. During an acute 12.5–25 mg Q 4–6H Chlorpromazine 100 mg episode of schizophrenia: 300– Increase dose as needed and 1000 mg/day tolerated Maintenance dose: 300–600 mg/day given in 1 or 2 divided doses with larger dose at bedtime 2.5–10 mg daily in divided doses Q6–8H Fluphenazine 2 mg Usual dose: 1–5 mg daily as a single dose Initial dose: 25–75 mg/day; use caution if starting with >100 Methotrimeprazine 70 mg mg/day Usual dose: 50–200 mg/day Divided in 1–3 doses Prochlorperazine ? 5–10 mg 3–4 times daily 2–5 mg BID or TID Trifluoperazine 5 mg Usual dose: 15–20 mg/day * Chlorpromazine 100 mg equivalent b) Other first generation antipsychotics e.g. -

Schizoaffective Disorder?
WHAT IS SCHIZOAFFECTIVE DISORDER? BASIC FACTS • SYMPTOMS • FAMILIES • TREATMENTS RT P SE A Mental Illness Research, Education and Clinical Center E C I D F I A C VA Desert Pacific Healthcare Network V M R E E Long Beach VA Healthcare System N T T N A E L C IL L LN A E IC S IN Education and Dissemination Unit 06/116A S R CL ESE N & ARCH, EDUCATIO 5901 E. 7th street | Long Beach, CA 90822 basic facts Schizoaffective disorder is a chronic and treatable psychiatric Causes illness. It is characterized by a combination of 1) psychotic symp- There is no simple answer to what causes schizoaffective dis- toms, such as those seen in schizophrenia and 2) mood symptoms, order because several factors play a part in the onset of the dis- such as those seen in depression or bipolar disorder. It is a psychi- order. These include a genetic or family history of schizoaffective atric disorder that can affect a person’s thinking, emotions, and be- disorder, schizophrenia, or bipolar disorder, biological factors, en- haviors and can impact all aspects of daily living, including work, vironmental stressors, and stressful life events. school, social relationships, and self-care. Research shows that the risk of schizoaffective disorder re- Schizoaffective disorder is considered a psychotic disorder sults from the influence of genes acting together with biological because of its prominent features of hallucinations and delusions. and environmental factors. A family history of schizoaffective dis- Therefore, people with this illness have periods when they have order does not necessarily mean children or other relatives will difficulty understanding the reality around them. -

207533Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 207533Orig1s000 MEDICAL REVIEW(S) CLINICAL REVIEW Application Type NDA Application Number(s) 207553 Priority or Standard Standard Submit Date(s) 8/22/2014 Received Date(s) 8/22/2014 PDUFA Goal Date 8/22/2015 Division / Office DPP/ODE1 Reviewer Name(s) Lucas Kempf, MD Review Completion Date October 2, 2015 Established Name Aripiprazole lauroxil (Proposed) Trade Name Aristada Therapeutic Class Antipsychotic Applicant Alkermes Inc. Formulation(s) Extended release injection Dosing Regimen Suspension/ IM up to 6 weeks Indication(s) Schizophrenia Intended Population(s) Schizophrenia Template Version: March 6, 2009 Reference ID: 3806701 Clinical Review Lucas Kempf, MD NDA 207533 Aristada, Aripiprazole lauroxil Table of Contents 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT ......................................... 7 1.1 Recommendation on Regulatory Action ............................................................. 7 1.2 Risk Benefit Assessment .................................................................................... 7 1.3 Recommendations for Postmarket Risk Evaluation and Mitigation Strategies ... 8 1.4 Recommendations for Postmarket Requirements and Commitments ................ 8 2 INTRODUCTION AND REGULATORY BACKGROUND ........................................ 8 2.1 Product Information ............................................................................................ 8 2.2 Currently Available Treatments for Proposed Indications .................................. -

Drug-Induced Parkinsonism
InformationInformation Sheet Sheet Drug-induced Parkinsonism Terms highlighted in bold italic are defined in increases with age, hypertension, diabetes, the glossary at the end of this information sheet. atrial fibrillation, smoking and high cholesterol), because of an increased risk of stroke and What is drug-induced parkinsonism? other cerebrovascular problems. It is unclear About 7% of people with parkinsonism whether there is an increased risk of stroke with have developed their symptoms following quetiapine and clozapine. See the Parkinson’s treatment with particular medications. This UK information sheet Hallucinations and form of parkinsonism is called ‘drug-induced Parkinson’s. parkinsonism’. While these drugs are used primarily as People with idiopathic Parkinson’s disease antipsychotic agents, it is important to note and other causes of parkinsonism may also that they can be used for other non-psychiatric develop worsening symptoms if treated with uses, such as control of nausea and vomiting. such medication inadvertently. For people with Parkinson’s, other anti-sickness drugs such as domperidone (Motilium) or What drugs cause drug-induced ondansetron (Zofran) would be preferable. parkinsonism? Any drug that blocks the action of dopamine As well as neuroleptics, some other drugs (referred to as a dopamine antagonist) is likely can cause drug-induced parkinsonism. to cause parkinsonism. Drugs used to treat These include some older drugs used to treat schizophrenia and other psychotic disorders high blood pressure such as methyldopa such as behaviour disturbances in people (Aldomet); medications for dizziness and with dementia (known as neuroleptic drugs) nausea such as prochlorperazine (Stemetil); are possibly the major cause of drug-induced and metoclopromide (Maxolon), which is parkinsonism worldwide. -

The Effects of Stimulants and Depressants on Cocaine Self-Administration Behavior in the Rhesus Monkey
Psychopharmacologia (Bed.) 31, 291--304 (1973) by Springer-Verlag 1973 The Effects of Stimulants and Depressants on Cocaine Self-Administration Behavior in the Rhesus Monkey M. C. Wilson* and C. R. Schuster** Pharmacology Department, University of Michigan Medical School Ann Arbor, Michigan Received June 22, 1972 Abstract. The effects of acute intramuscular pretreatment with several dosages of a variety of centrally acting compounds on intravenous cocaine self-administra- tion behavior were ascertained. Pretreatment with morphine and pentobarbital produced no change in this behavior until dosages (2.0 mg/kg and 15.0 mg/kg respectively) were administered which grossly depressed grooming, exploratory, and locomotor activity behaviors, d-amphetamine (0.5--4.0 mg/kg) and phenmetra- zine (2.0--12.0 mg/kg) pretreatment produced a dose-related decrease in cocaine self-administration. Trifluoperazine in dosages of 0.01--0.1 mg/kg increased the frequency of this behavior; whereas, higher dosages (0,2, 0.4mg/kg) grossly depressed behavior. Imipramine (10--50 mg/kg) produced a dose-related decrease in cocaine self-administration. Potential mechanisms of these drug--behavior and drug--drug interactions are discussed. Key words: Self-Administration -- Cocaine -- Morphine -- Pentobarbital -- Trifluoperazine. Previous investigations have demonstrated an inverse relationship between reinforcing unit dosages (dosage per injection) and the fre- quency of psychomotor stimulant (including cocaine) intravenous self- administration behavior in Rhesus monkeys (Wilson, Hitomi, and Schuster, 1971; Woods and Schuster, 1968; Goldberg, Hoffmeister, Sehlichting, and Wuttke, 1971). Furthermore, when allowed limited daily access to these agents, a subject's total daily drug intake was very stable. Similar results have also been reported by several authors using rats as experimental subjects with intravenously self-administered eoeaine (Piekens and Thomson, 1968), methamphetamine (Piekens, Meisch, and McGuire, 1967) and d-amphetamine (Piekens and Harris, 1968).