Fundamentals of Neurologic Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Inherited Cerebellar Ataxia in Childhood: a Pattern-Recognition Approach Using Brain MRI
REVIEW ARTICLE Inherited Cerebellar Ataxia in Childhood: A Pattern-Recognition Approach Using Brain MRI L. Vedolin, G. Gonzalez, C.F. Souza, C. Lourenc¸o, and A.J. Barkovich ABSTRACT SUMMARY: Ataxia is the principal symptom of many common neurologic diseases in childhood. Ataxias caused by dysfunction of the cerebellum occur in acute, intermittent, and progressive disorders. Most of the chronic progressive processes are secondary to degen- erative and metabolic diseases. In addition, congenital malformation of the midbrain and hindbrain can also be present, with posterior fossa symptoms related to ataxia. Brain MR imaging is the most accurate imaging technique to investigate these patients, and imaging abnormalities include size, shape, and/or signal of the brain stem and/or cerebellum. Supratentorial and cord lesions are also common. This review will discuss a pattern-recognition approach to inherited cerebellar ataxia in childhood. The purpose is to provide a comprehensive discussion that ultimately could help neuroradiologists better manage this important topic in pediatric neurology. ABBREVIATIONS: AR ϭ autosomal recessive; CAC ϭ cerebellar ataxia in childhood; 4H ϭ hypomyelination with hypogonadotropic hypogonadism and hypodon- tia; JSRD ϭ Joubert syndrome and related disorders; OPHN1 ϭ oligophrenin-1 taxia is an inability to coordinate voluntary muscle move- plastic/paraneoplastic disorders, immune-mediated/demyelinat- Aments that cannot be attributed to weakness or involuntary ing disorders, and drugs/toxins (antiepileptic medications, -

Pearls: Infectious Diseases
Pearls: Infectious Diseases Karen L. Roos, M.D.1 ABSTRACT Neurologists have a great deal of knowledge of the classic signs of central nervous system infectious diseases. After years of taking care of patients with infectious diseases, several symptoms, signs, and cerebrospinal fluid abnormalities have been identified that are helpful time and time again in determining the etiological agent. These lessons, learned at the bedside, are reviewed in this article. KEYWORDS: Herpes simplex virus, Lyme disease, meningitis, viral encephalitis CLINICAL MANIFESTATIONS does not have an altered level of consciousness, sei- zures, or focal neurologic deficits. Although the ‘‘classic triad’’ of bacterial meningitis is The rash of a viral exanthema typically involves the fever, headache, and nuchal rigidity, vomiting is a face and chest first then spreads to the arms and legs. common early symptom. Suspect bacterial meningitis This can be an important clue in the patient with in the patient with fever, headache, lethargy, and headache, fever, and stiff neck that the meningitis is vomiting (without diarrhea). Patients may also com- due to echovirus or coxsackievirus. plain of photophobia. An altered level of conscious- Suspect tuberculous meningitis in the patient with ness that begins with lethargy and progresses to stupor either several weeks of headache, fever, and night during the emergency evaluation of the patient is sweats or a fulminant presentation with fever, altered characteristic of bacterial meningitis. mental status, and focal neurologic deficits. Fever (temperature 388C[100.48F]) is present in An Ixodes tick must be attached to the skin for at least 84% of adults with bacterial meningitis and in 80 to 24 hours to transmit infection with the spirochete 1–3 94% of children with bacterial meningitis. -

Acquired Aphasia in Children
13 Acquired Aphasia in Children DOROTHY M. ARAM Introduction Children versus Adults Language disruptions secondary to acquired central nervous system (CNS) lesions differ between children and adults in multiple respects. Chief among these differences are the developmental stage of language ac- quisition at the time of insult and the developmental stage of the CNS. In adult aphasia premorbid mastery of language is assumed, at least to the level of the aphasic's intellectual ability and educational opportunities. Acquired aphasia sustained in childhood, however, interferes with the de- velopmental process of language learning and disrupts those aspects of language already mastered. The investigator and clinician thus are faced with sorting which aspects of language have been lost or impaired from those yet to emerge, potentially in an altered manner. Complicating re- search and clinical practice in this area is the need to account continually for the developmental stage of that aspect of language under consideration for each child. In research, stage-appropriate language tasks must be se- lected, and comparison must be made to peers of comparable age and lan- guage stage. Also, appropriate controls common in adult studies, such as social class and gender, are critical. These requirements present no small challenge, as most studies involve a wide age range of children and ado- lescents. In clinical practice, the question is whether assessment tools used for developmental language disorders should be used or whether adult aphasia batteries should be adapted for children. The answer typically de- pends on the age of the child and the availability of age- and stage-appro- 451 ACQUIRED APHASIA, THIRD EDITION Copyright 1998 by Academic Press. -

Overview of Stroke: Etiologies, Demographics, Syndromes, And
Overview of Stroke: Etiologies, Demographics, Syndromes, and Outcomes Alex Abou-Chebl, MD, FSVIN Medical Director, Stroke Baptist Health Louisville Disclosure Statement of Financial Interest Within the past 12 months, I or my spouse/partner have had a financial interest/arrangement or affiliation with the organization(s) listed below. Affiliation/Financial Relationship Company Consulting Fees/Honoraria The Medicines Co. Silk Road Medical Definitions Stroke - abrupt development of a focal neurological deficit due to a vascular cause associated with permanent neuronal injury Transient ischemic attack (TIA)- same clinical syndrome as a stroke but resolves completely < 24 hours i.e. without permanent brain injury (old definition) With modern imaging most events >several hours duration are associated with infarction. Epidemiology- USA ~795,000 new or recurrent stroke per year 610,000 first attacks 185,000 recurrent attacks 2001 to 2011 relative rate of stroke death fell 35.1% Actual number of stroke deaths declined 23.0% In 2011 stroke caused ~1 of every 20 deaths in USA On average,1 stroke every 40 seconds in USA 1 Stroke death every 4 minutes There are ~ 4.5-5 million Stroke survivors Stroke is the leading cause of adult disability in USA 15-30% of all stroke leads to permanent disability Mozaffarian D, et al. Heart Disease and Stroke Statistics- 2015 Update. Circulation 2015;131:e29-322. Prevalence of Stroke by Age and Sex (National Health and Nutrition Examination Survey: 2009–2012). Dariush Mozaffarian et al. Circulation. 2015;131:e29-e322 Copyright © American Heart Association, Inc. All rights reserved. Annual Age-adjusted Incidence of First-ever Stroke by Race. -

Synchronized Babinski and Chaddock Signs Preceded the MRI Findings in a Case of Repetitive Transient Ischemic Attack
□ CASE REPORT □ Synchronized Babinski and Chaddock Signs Preceded the MRI Findings in a Case of Repetitive Transient Ischemic Attack Kosuke Matsuzono 1,2, Takao Yoshiki 1, Yosuke Wakutani 1, Yasuhiro Manabe 3, Toru Yamashita 2, Kentaro Deguchi 2, Yoshio Ikeda 2 and Koji Abe 2 Abstract We herein report a 53-year-old female with repeated transient ischemic attack (TIA) symptoms including 13 instances of right hemiparesis that decreased in duration over 4 days. Two separate examinations using diffusion weighted image (DWI) in magnetic resonance imaging (MRI) revealed normal findings, but we ob- served that both Babinski and Chaddock signs were completely synchronized with her right hemiparesis. We were only able to diagnose this case of early stage TIA using clinical signs. This diagnosis was confirmed 4 days after the onset by the presence of abnormalities on the MRI. DWI-MRI is generally useful when diag- nosing TIA, but a neurological examination may be more sensitive, especially in the early stages. Key words: Babinski sign, Chaddock sign, TIA, diffusion weighted image (Intern Med 52: 2127-2129, 2013) (DOI: 10.2169/internalmedicine.52.0190) Introduction Case Report Transient ischemic attack (TIA) is a clinical syndrome A 53-year-old woman suddenly developed right hemipare- that consists of sudden focal neurologic signs and a com- sis, and she was admitted to our hospital 30 minutes after plete recovery usually within 24 hours (1). Because TIA can the onset. She had smoked 10 cigarettes daily for 23 years, sometimes develop into a cerebral infarction, an early diag- and quit at 43 years of age. -

Cerebritis: an Unusual Complication of Klebsiella Pneumoniae
Case Report Cerebritis: An unusual complication of Klebsiella pneumoniae Mainak Majumdar, David C. Simes1, Ramesh D. Prabha1 Cerebritis is part of a continuum of brain infection and is difficult to diagnose. Cerebritis caused by Klebsiella in immunocompetent adults without predisposing factors such as neurosurgery or penetrating brain injury has not been reported before. We report a case of Klebsiella cerebritis in an adult patient with a proven extracranial focus of infection. We suggest considering cerebritis as a differential diagnosis for altered level of consciousness in patients Abstract of severe sepsis, even if an extracranial source of infection is proven. Key words: Alcohol, cerebritis, Klebsiella DOI: 10.4103/0972-5229.53116 Introduction heavy smoking, heavy ethanol use, and two prior hospital admissions for pneumonia and exacerbation of Cerebritis without a history of penetrating head chronic obstructive airways disease. trauma or neurosurgery is a rarely suspected cause of coma. Bacteria gain entry to brain tissue and cause infection either by direct spread or through At presentation she was febrile, delirious, and hematogenous seeding.[1] In Gram-negative CNS tachypneic with low oxygen saturations, relative infections, a primary focus of infection may be found hypotension, and new onset atrial fibrillation with a rapid ventricular response. Her chest X-ray revealed dense right in neonates and in trauma and neurosurgical patients, upper and middle lobe consolidation. Initial treatment but in adults without antecedent surgery, there will consisted of oxygen therapy, intravenous fluid resuscitation, be no primary focus of infection detected in up to noninvasive ventilation, and antibiotics (ceftriaxone and 60% of cases.[2] Further, sedation in the intensive care azithromycin) for her community acquired pneumonia. -

Neuropathology Category Code List
Neuropathology Page 1 of 27 Neuropathology Major Category Code Headings Revised 10/2018 1 General neuroanatomy, pathology, and staining 65000 2 Developmental neuropathology, NOS 65400 3 Epilepsy 66230 4 Vascular disorders 66300 5 Trauma 66600 6 Infectious/inflammatory disease 66750 7 Demyelinating diseases 67200 8 Complications of systemic disorders 67300 9 Aging and neurodegenerative diseases 68000 10 Prion diseases 68400 11 Neoplasms 68500 12 Skeletal Muscle 69500 13 Peripheral Nerve 69800 14 Ophthalmic pathology 69910 Neuropathology Page 2 of 27 Neuropathology 1 General neuroanatomy, pathology, and staining 65000 A Neuroanatomy, NOS 65010 1 Neocortex 65011 2 White matter 65012 3 Entorhinal cortex/hippocampus 65013 4 Deep (basal) nuclei 65014 5 Brain stem 65015 6 Cerebellum 65016 7 Spinal cord 65017 8 Pituitary 65018 9 Pineal 65019 10 Tracts 65020 11 Vascular supply 65021 12 Notochord 65022 B Cell types 65030 1 Neurons 65031 2 Astrocytes 65032 3 Oligodendroglia 65033 4 Ependyma 65034 5 Microglia and mononuclear cells 65035 6 Choroid plexus 65036 7 Meninges 65037 8 Blood vessels 65038 C Cerebrospinal fluid 65045 D Pathologic responses in neurons and axons 65050 1 Axonal degeneration/spheroid/reaction 65051 2 Central chromatolysis 65052 3 Tract degeneration 65053 4 Swollen/ballooned neurons 65054 5 Trans-synaptic neuronal degeneration 65055 6 Olivary hypertrophy 65056 7 Acute ischemic (hypoxic) cell change 65057 8 Apoptosis 65058 9 Protein aggregation 65059 10 Protein degradation/ubiquitin pathway 65060 E Neuronal nuclear inclusions 65100 -
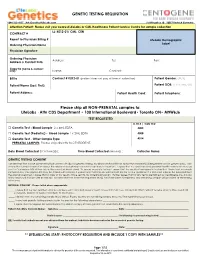
GENETIC TESTING REQUISITION Please Ship All
GENETIC TESTING REQUISITION 1-844-363-4357· [email protected] Schillingallee 68 · 18057 Rostock Germany Attention Patient: Please visit your nearest LifeLabs or CML Healthcare Patient Service Centre for sample collection LL: K012-01/ CML: CEN CONTRACT # Report to Physician Billing # LifeLabs Demographic Ordering Physician Name Label Physician Signature: Ordering Physician Address: Tel: Fax: Address & Contact Info: Copy to (name & contact info): Name: Contact: Bill to Contract # K012-01 (patient does not pay at time of collection) Patient Gender: (M/F) Patient Name (Last, First): Patient DOB: (YYYY/MM/DD) Patient Address: Patient Health Card: Patient Telephone: Please ship all NON-PRENATAL samples to: LifeLabs · Attn CDS Department • 100 International Boulevard• Toronto ON• M9W6J6 TEST REQUESTED LL TR # / CML TC# □ Genetic Test - Blood Sample 2 x 4mL EDTA 4005 □ Genetic Test (Pediatric) - Blood Sample 1 x 2mL EDTA 4008 □ Genetic Test - Other Sample Type 4014 PRENATAL SAMPLES: Please ship directly to CENTOGENE. Date Blood Collected (YYYY/MM/DD): ___________ Time Blood Collected (HH:MM)) :________ Collector Name: ___________________ GENETIC TESTING CONSENT I understand that a DNA specimen will be sent to LifeLabs for genetic testing. My physician has told me about the condition(s) being tested and its genetic basis. I am aware that correct information about the relationships between my family members is important. I agree that my specimen and personal health information may be sent to Centogene AG at their lab in Germany (address below). To ensure accurate testing, I agree that the results of any genetic testing that I have had previously completed by Centogene AG may be shared with LifeLabs. -

UCSD Moores Cancer Center Neuro-Oncology Program
UCSD Moores Cancer Center Neuro-Oncology Program Recent Progress in Brain Tumors 6DQWRVK.HVDUL0'3K' 'LUHFWRU1HXUR2QFRORJ\ 3URIHVVRURI1HXURVFLHQFHV 0RRUHV&DQFHU&HQWHU 8QLYHUVLW\RI&DOLIRUQLD6DQ'LHJR “Brain Cancer for Life” Juvenile Pilocytic Astrocytoma Metastatic Brain Cancer Glioblastoma Multiforme Glioblastoma Multiforme Desmoplastic Infantile Ganglioglioma Desmoplastic Variant Astrocytoma Medulloblastoma Atypical Teratoid Rhabdoid Tumor Diffuse Intrinsic Pontine Glioma -Mutational analysis, microarray expression, epigenetic phenomenology -Age-specific biology of brain cancer -Is there an overlap? ? Neuroimmunology ? Stem cell hypothesis Courtesy of Dr. John Crawford Late Effects Long term effect of chemotherapy and radiation on neurocognition Risks of secondary malignancy secondary to chemotherapy and/or radiation Neurovascular long term effects: stroke, moya moya Courtesy of Dr. John Crawford Importance Increase in aging population with increased incidence of cancer Patients with cancer living longer and developing neurologic disorders due to nervous system relapse or toxicity from treatments Overview Introduction Clinical Presentation Primary Brain Tumors Metastatic Brain Tumors Leptomeningeal Metastases Primary CNS Lymphoma Paraneoplastic Syndromes Classification of Brain Tumors Tumors of Neuroepithelial Tissue Glial tumors (astrocytic, oligodendroglial, mixed) Neuronal and mixed neuronal-glial tumors Neuroblastic tumors Pineal parenchymal tumors Embryonal tumors Tumors of Peripheral Nerves Shwannoma Neurofibroma -

Atypical Development of the Cerebellum : Impact on Language Function Lynette M
University of New Mexico UNM Digital Repository Psychology ETDs Electronic Theses and Dissertations 8-28-2012 Atypical development of the cerebellum : impact on language function Lynette M. Silva Follow this and additional works at: https://digitalrepository.unm.edu/psy_etds Recommended Citation Silva, Lynette M.. "Atypical development of the cerebellum : impact on language function." (2012). https://digitalrepository.unm.edu/psy_etds/129 This Dissertation is brought to you for free and open access by the Electronic Theses and Dissertations at UNM Digital Repository. It has been accepted for inclusion in Psychology ETDs by an authorized administrator of UNM Digital Repository. For more information, please contact [email protected]. Lynette M. Silva Candidate Psychology Department This dissertation is approved, and it is acceptable in quality and form for publication: Approved by the Dissertation Committee: Steven Verney, Co-Chairperson Ron Yeo, Co-Chairperson Robert Thoma Jean Lowe ATYPICAL DEVELOPMENT OF THE CEREBELLUM: IMPACT ON LANGUAGE FUNCTION By LYNETTE M. SILVA B.A., English, Stanford University, 1996 M.S., Psychology, University of New Mexico, 2009 DISSERTATION Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy Psychology The University of New Mexico Albuquerque, New Mexico July 2012 iii Dedication For my parents, extended family, and valued friends, because it took a village. And for Martin Rodriguez, who served as my Virgil, and showed me the way. iv Acknowledgements I would like to thank Drs. Steven Verney, Ron Yeo, Robert Thoma, and Jean Lowe for their guidance and support as members of my dissertation committee. I am very thankful for the encouragement and supervision I continue to receive from Dr. -

Clinical Characteristics and Prognostic Factors in Childhood
BALKAN MEDICAL JOURNAL 80 THE OFFICIAL JOURNAL OF TRAKYA UNIVERSITY FACULTY OF MEDICINE © Trakya University Faculty of Medicine Balkan Med J 2013; 30: 80-4 • DOI: 10.5152/balkanmedj.2012.092 Available at www.balkanmedicaljournal.org Original Article Clinical Characteristics and Prognostic Factors in Childhood Bacterial Meningitis: A Multicenter Study Özden Türel1, Canan Yıldırım2, Yüksel Yılmaz2, Sezer Külekçi3, Ferda Akdaş3, Mustafa Bakır1 1Department of Pediatrics, Section of Pediatric Infectious Diseases, Faculty of Medicine, Marmara University, İstanbul, Turkey 2Department of Pediatrics, Section of Pediatric Neurology, Faculty of Medicine, Marmara University, İstanbul, Turkey 3Department of Audiology, Faculty of Medicine, Marmara University, İstanbul, Turkey İstanbul, Turkey ABSTRACT Objective: To evaluate clinical features and sequela in children with acute bacterial meningitis (ABM). Study Design: Multicenter retrospective study. Material and Methods: Study includes retrospective chart review of children hospitalised with ABM at 11 hospitals in İstanbul during 2005. Follow up visits were conducted for neurologic examination, hearing evaluation and neurodevelopmental tests. Results: Two hundred and eighty three children were included in the study. Median age was 12 months and 68.6% of patients were male. Almost all patients had fever at presentation (97%). Patients younger than 6 months tended to present with feeding difficulties (84%), while patients older than 24 months were more likely to present with vomitting (93%) and meningeal signs (84%). Seizures were present in 65 (23%) patients. 26% of patients were determined to have at least one major sequela. The most common sequelae were speech or language problems (14.5%). 6 patients were severely disabled because of meningitis. Presence of focal neurologic signs at presentation and turbid cerebrospinal fluid appearance increased sequelae signifi- cantly. -

Pharmacologic Treatment of Meningitis and Encephalitis in Adult Patients
Published online: 2019-06-19 THIEME Review Article 145 Pharmacologic Treatment of Meningitis and Encephalitis in Adult Patients Andrew K. Treister1 Ines P. Koerner2 1Department of Neurology, Oregon Health & Science University, Address for correspondence Andrew K. Treister, MD, Department Portland, Oregon, United States of Neurology, Oregon Health & Science University, 3181 SW Sam 2Department of Anesthesiology and Perioperative Medicine, Jackson Park, CR 120, Portland, OR 97239-3098, United States Oregon Health & Science University, Portland, Oregon, (e-mail: [email protected]). United States J Neuroanaesthesiol Crit Care 2019;6:145–152 Abstract Meningitis and encephalitis are two inflammatory, often infectious, disorders of the meninges and the central nervous system. Both are associated with significant morbidity and mortality, and require early and aggressive targeted treatment. This article reviews pharmacologic treatment strategies for infectious meningitis and encephalitis, using Keywords the latest available research and guidelines. It provides an overview of empiric anti- ► meningitis microbial treatment approaches for a variety of organisms, including a discussion of ► encephalitis trends in antibiotic resistance where applicable. Key steps in diagnosis and general ► antibiotic resistance management are briefly reviewed. Introduction care–associated infections are not covered in detail, as they are excellently discussed in a recent guideline statement.4 The terms meningitis and encephalitis comprise a broad array of infectious and inflammatory processes involving the central nervous system (CNS) that carry significant morbidity Literature Review 1,2 and mortality. Meningitis refers to inflammation of PubMed was searched in January 2019 for articles published primarily the meninges, although it may spread to involve the between January 1, 2009, and December 31, 2018.