Expression of a Novel CNPY2 Isoform in Colorectal Cancer and Its Association with Oncologic Prognosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Molecular Profile of Tumor-Specific CD8+ T Cell Hypofunction in a Transplantable Murine Cancer Model
Downloaded from http://www.jimmunol.org/ by guest on September 25, 2021 T + is online at: average * The Journal of Immunology , 34 of which you can access for free at: 2016; 197:1477-1488; Prepublished online 1 July from submission to initial decision 4 weeks from acceptance to publication 2016; doi: 10.4049/jimmunol.1600589 http://www.jimmunol.org/content/197/4/1477 Molecular Profile of Tumor-Specific CD8 Cell Hypofunction in a Transplantable Murine Cancer Model Katherine A. Waugh, Sonia M. Leach, Brandon L. Moore, Tullia C. Bruno, Jonathan D. Buhrman and Jill E. Slansky J Immunol cites 95 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html http://www.jimmunol.org/content/suppl/2016/07/01/jimmunol.160058 9.DCSupplemental This article http://www.jimmunol.org/content/197/4/1477.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2016 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 25, 2021. The Journal of Immunology Molecular Profile of Tumor-Specific CD8+ T Cell Hypofunction in a Transplantable Murine Cancer Model Katherine A. -

Engineered Type 1 Regulatory T Cells Designed for Clinical Use Kill Primary
ARTICLE Acute Myeloid Leukemia Engineered type 1 regulatory T cells designed Ferrata Storti Foundation for clinical use kill primary pediatric acute myeloid leukemia cells Brandon Cieniewicz,1* Molly Javier Uyeda,1,2* Ping (Pauline) Chen,1 Ece Canan Sayitoglu,1 Jeffrey Mao-Hwa Liu,1 Grazia Andolfi,3 Katharine Greenthal,1 Alice Bertaina,1,4 Silvia Gregori,3 Rosa Bacchetta,1,4 Norman James Lacayo,1 Alma-Martina Cepika1,4# and Maria Grazia Roncarolo1,2,4# Haematologica 2021 Volume 106(10):2588-2597 1Department of Pediatrics, Division of Stem Cell Transplantation and Regenerative Medicine, Stanford School of Medicine, Stanford, CA, USA; 2Stanford Institute for Stem Cell Biology and Regenerative Medicine, Stanford School of Medicine, Stanford, CA, USA; 3San Raffaele Telethon Institute for Gene Therapy, Milan, Italy and 4Center for Definitive and Curative Medicine, Stanford School of Medicine, Stanford, CA, USA *BC and MJU contributed equally as co-first authors #AMC and MGR contributed equally as co-senior authors ABSTRACT ype 1 regulatory (Tr1) T cells induced by enforced expression of interleukin-10 (LV-10) are being developed as a novel treatment for Tchemotherapy-resistant myeloid leukemias. In vivo, LV-10 cells do not cause graft-versus-host disease while mediating graft-versus-leukemia effect against adult acute myeloid leukemia (AML). Since pediatric AML (pAML) and adult AML are different on a genetic and epigenetic level, we investigate herein whether LV-10 cells also efficiently kill pAML cells. We show that the majority of primary pAML are killed by LV-10 cells, with different levels of sensitivity to killing. Transcriptionally, pAML sensitive to LV-10 killing expressed a myeloid maturation signature. -

Downregulation of Carnitine Acyl-Carnitine Translocase by Mirnas
Page 1 of 288 Diabetes 1 Downregulation of Carnitine acyl-carnitine translocase by miRNAs 132 and 212 amplifies glucose-stimulated insulin secretion Mufaddal S. Soni1, Mary E. Rabaglia1, Sushant Bhatnagar1, Jin Shang2, Olga Ilkayeva3, Randall Mynatt4, Yun-Ping Zhou2, Eric E. Schadt6, Nancy A.Thornberry2, Deborah M. Muoio5, Mark P. Keller1 and Alan D. Attie1 From the 1Department of Biochemistry, University of Wisconsin, Madison, Wisconsin; 2Department of Metabolic Disorders-Diabetes, Merck Research Laboratories, Rahway, New Jersey; 3Sarah W. Stedman Nutrition and Metabolism Center, Duke Institute of Molecular Physiology, 5Departments of Medicine and Pharmacology and Cancer Biology, Durham, North Carolina. 4Pennington Biomedical Research Center, Louisiana State University system, Baton Rouge, Louisiana; 6Institute for Genomics and Multiscale Biology, Mount Sinai School of Medicine, New York, New York. Corresponding author Alan D. Attie, 543A Biochemistry Addition, 433 Babcock Drive, Department of Biochemistry, University of Wisconsin-Madison, Madison, Wisconsin, (608) 262-1372 (Ph), (608) 263-9608 (fax), [email protected]. Running Title: Fatty acyl-carnitines enhance insulin secretion Abstract word count: 163 Main text Word count: 3960 Number of tables: 0 Number of figures: 5 Diabetes Publish Ahead of Print, published online June 26, 2014 Diabetes Page 2 of 288 2 ABSTRACT We previously demonstrated that micro-RNAs 132 and 212 are differentially upregulated in response to obesity in two mouse strains that differ in their susceptibility to obesity-induced diabetes. Here we show the overexpression of micro-RNAs 132 and 212 enhances insulin secretion (IS) in response to glucose and other secretagogues including non-fuel stimuli. We determined that carnitine acyl-carnitine translocase (CACT, Slc25a20) is a direct target of these miRNAs. -

By IL-4 in Memory CD8 T Cells Negative Regulation of NKG2D
Negative Regulation of NKG2D Expression by IL-4 in Memory CD8 T Cells Erwan Ventre, Lilia Brinza, Stephane Schicklin, Julien Mafille, Charles-Antoine Coupet, Antoine Marçais, Sophia This information is current as Djebali, Virginie Jubin, Thierry Walzer and Jacqueline of October 2, 2021. Marvel J Immunol published online 31 August 2012 http://www.jimmunol.org/content/early/2012/08/31/jimmun ol.1102954 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2012/09/04/jimmunol.110295 Material 4.DC1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on October 2, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2012 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Published August 31, 2012, doi:10.4049/jimmunol.1102954 The Journal of Immunology Negative Regulation of NKG2D Expression by IL-4 in Memory CD8 T Cells Erwan Ventre, Lilia Brinza,1 Stephane Schicklin,1 Julien Mafille, Charles-Antoine Coupet, Antoine Marc¸ais, Sophia Djebali, Virginie Jubin, Thierry Walzer, and Jacqueline Marvel IL-4 is one of the main cytokines produced during Th2-inducing pathologies. -

Transforming Growth Factor ß1-Mediated Functional Inhibition Of
Myelodysplastic Syndromes SUPPLEMENTARY APPENDIX Transforming growth factor 1- mediated functional inhibition of mesenchymal stromal celβls in myelodysplastic syndromes and acute myeloid leukemia Stefanie Geyh, 1* Manuel Rodríguez-Paredes, 1,2 * Paul Jäger, 1 Annemarie Koch, 1 Felix Bormann, 2 Julian Gutekunst, 2 Christoph Zilkens, 3 Ulrich Germing, 1 Guido Kobbe, 1 Frank Lyko, 2 Rainer Haas 1 and Thomas Schroeder 1 1Department of Hematology, Oncology and Clinical Immunology, University of Duesseldorf, Medical Faculty; 2Division of Epigenetics, DKFZ- ZMBH Alliance, German Cancer Research Center, Heidelberg and 3Department of Orthopedic Surgery, University of Duesseldorf, Medical Faculty, Germany *SG and MR-P contributed equally to this work. ©2018 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol. 2017.186734 Received: December 19, 2017. Accepted: May 14, 2018. Pre-published: May 17, 2018. Correspondence: [email protected] Figure S1 Downregulated genes Downregulated genes Upregulated Figure S1. Heatmaps showing the 50 most upregulated and downregulated genes between the 3 healthy MSC controls and the 9 RCMD-, RAEB- and AML-derived MSC samples. Color scale depicts the rlog-transformed FPKM values for each gene and every sample. Figure S2 Downregulated genes Downregulated genes Upregulated Figure S2. Heatmaps showing the 50 most upregulated and downregulated genes between the 3 healthy MSC controls and the 3 RCMD, RAEB and AML MSC samples, respectively. Color scales depict the rlog-transformed FPKM values for each gene and every sample. Figure S3 A. B. 0.0015 *** ** <-3 -2 0.0010 RCMD RAEB AML -1 0 1 0.0005 Log2FC LTF 2 CCL26/GAPDH INHBB >3 0.0000 TGFB2 y S h D ML M A ealt ll LTF H a EGF 0.003 *** ** INHBB TGFB2 0.002 INHBB IGFBP7 0.001 GDF11 LIF/GAPDH BMP1 0.000 y L th M TNFSF12 l A FGF13 ea ll MDS H a FGF13 0.0015 * TNFSF10 TNFSF10 0.0010 0.0005 SPP1/GAPDH 0.0000 y th l AML ea H all MDS Figure S3. -

Oxidized Phospholipids Regulate Amino Acid Metabolism Through MTHFD2 to Facilitate Nucleotide Release in Endothelial Cells
ARTICLE DOI: 10.1038/s41467-018-04602-0 OPEN Oxidized phospholipids regulate amino acid metabolism through MTHFD2 to facilitate nucleotide release in endothelial cells Juliane Hitzel1,2, Eunjee Lee3,4, Yi Zhang 3,5,Sofia Iris Bibli2,6, Xiaogang Li7, Sven Zukunft 2,6, Beatrice Pflüger1,2, Jiong Hu2,6, Christoph Schürmann1,2, Andrea Estefania Vasconez1,2, James A. Oo1,2, Adelheid Kratzer8,9, Sandeep Kumar 10, Flávia Rezende1,2, Ivana Josipovic1,2, Dominique Thomas11, Hector Giral8,9, Yannick Schreiber12, Gerd Geisslinger11,12, Christian Fork1,2, Xia Yang13, Fragiska Sigala14, Casey E. Romanoski15, Jens Kroll7, Hanjoong Jo 10, Ulf Landmesser8,9,16, Aldons J. Lusis17, 1234567890():,; Dmitry Namgaladze18, Ingrid Fleming2,6, Matthias S. Leisegang1,2, Jun Zhu 3,4 & Ralf P. Brandes1,2 Oxidized phospholipids (oxPAPC) induce endothelial dysfunction and atherosclerosis. Here we show that oxPAPC induce a gene network regulating serine-glycine metabolism with the mitochondrial methylenetetrahydrofolate dehydrogenase/cyclohydrolase (MTHFD2) as a cau- sal regulator using integrative network modeling and Bayesian network analysis in human aortic endothelial cells. The cluster is activated in human plaque material and by atherogenic lipo- proteins isolated from plasma of patients with coronary artery disease (CAD). Single nucleotide polymorphisms (SNPs) within the MTHFD2-controlled cluster associate with CAD. The MTHFD2-controlled cluster redirects metabolism to glycine synthesis to replenish purine nucleotides. Since endothelial cells secrete purines in response to oxPAPC, the MTHFD2- controlled response maintains endothelial ATP. Accordingly, MTHFD2-dependent glycine synthesis is a prerequisite for angiogenesis. Thus, we propose that endothelial cells undergo MTHFD2-mediated reprogramming toward serine-glycine and mitochondrial one-carbon metabolism to compensate for the loss of ATP in response to oxPAPC during atherosclerosis. -

The Extracellular Bone Marrow Microenvironment—A Proteomic Comparison of Constitutive Protein Release by in Vitro Cultured Osteoblasts and Mesenchymal Stem Cells
cancers Article The Extracellular Bone Marrow Microenvironment—A Proteomic Comparison of Constitutive Protein Release by In Vitro Cultured Osteoblasts and Mesenchymal Stem Cells Elise Aasebø 1 , Even Birkeland 2, Frode Selheim 2, Frode Berven 2, Annette K. Brenner 1 and Øystein Bruserud 1,3,* 1 Department of Clinical Science, University of Bergen, N-5021 Bergen, Norway; [email protected] (E.A.); [email protected] (A.K.B.) 2 The Proteomics Facility of the University of Bergen (PROBE), University of Bergen, N-5021 Bergen, Norway; [email protected] (E.B.); [email protected] (F.S.); [email protected] (F.B.) 3 Department of Medicine, Haukeland University Hospital, N-5021 Bergen, Norway * Correspondence: [email protected] or [email protected]; Tel.: +47-5597-2997 Simple Summary: Normal blood cells are formed in the bone marrow by a process called hematopoiesis. This process is supported by a network of non-hematopoietic cells including connective tissue cells, blood vessel cells and bone-forming cells. However, these cells can also support the growth of cancer cells, i.e., hematological malignancies (e.g., leukemias) and cancers that arise in another organ and spread to the bone marrow. Two of these cancer-supporting normal cells are bone-forming osteoblasts and a subset of connective tissue cells called mesenchymal stem cells. One mechanism for their cancer support is the release of proteins that support cancer cell proliferation and progression of the cancer disease. Our present study shows that both these normal cells release a wide range of proteins that support cancer cells, and inhibition of this protein-mediated cancer support may become a new strategy for cancer treatment. -

Gene List HTG Edgeseq Oncology Biomarker Panel
Gene List HTG EdgeSeq Oncology Biomarker Panel For Research Use Only. Not for use in diagnostic procedures. A2M ADRA2B APH1B BAG1 BRCA2 CARM1 CCNH CDC25A CHI3L1 COX7B CXCL16 DESI1 ABCA2 ADRA2C APOC2 BAG2 BRIP1 CASP1 CCNO CDC25B CHI3L2 CP CXCL2 DFFA ABCA3 AFF1 APOC4 BAG3 BTC CASP10 CCNT1 CDC25C CHMP4B CPT1A CXCL3 DHCR24 ABCA4 AGER APOL3 BAG4 BTG1 CASP12 CCR1 CDC34 CHPT1 CPT1B CXCL5 DHH ABCA5 AGFG1 APP BAG5 BTG2 CASP14 CCR10 CDC42 CHRNA1 CPT1C CXCL6 DHX58 ABCA9 AGGF1 APPBP2 BAI1 BTG3 CASP2 CCR2 CDC42BPA CHRNB1 CPT2 CXCL8 DIABLO ABCB11 AGT AQP1 BAIAP3 BTK CASP3 CCR3 CDC6 CHSY1 CRADD CXCL9 DIAPH3 ABCB4 AHNAK AQP2 BAK1 BTRC CASP4 CCR4 CDC7 CHUK CREB1 CXCR1 DICER1 ABCB5 AHNAK2 AQP4 BAMBI BUB1 CASP5 CCR5 CDCA7 CIC CREB3L1 CXCR2 DISP1 ABCB6 AHR AQP7 BAP1 BUB1B CASP6 CCR6 CDH1 CIDEA CREB3L3 CXCR3 DISP2 ABCC1 AHRR AQP9 BATF C17orf53 CASP7 CCR7 CDH13 CIDEB CREB3L4 CXCR4 DKC1 ABCC10 AICDA AR BAX C19orf40 CASP8 CCR8 CDH15 CIRBP CREB5 CXCR5 DKK1 ABCC11 AIFM1 ARAF BBC3 C1orf106 CASP8AP2 CCR9 CDH2 CITED2 CREBBP CXCR6 DKK2 ABCC12 AIMP2 AREG BBS4 C1orf159 CASP9 CCRL2 CDH3 CKB CRK CXXC4 DKK3 ABCC2 AK1 ARHGAP44 BCAR1 C1orf86 CAV1 CCS CDH5 CKLF CRLF2 CXXC5 DKK4 ABCC3 AK2 ARHGEF16 BCAT1 C1QA CAV2 CCT2 CDK1 CKMT1A CRLS1 CYBA DLC1 ABCC4 AK3 ARID1A BCCIP C1S CBL CCT3 CDK16 CKMT2 CRP CYBB DLGAP5 ABCC5 AKAP1 ARID1B BCL10 C3 CBLC CCT4 CDK2 CKS1B CRTAC1 CYCS DLK1 ABCC6 AKR1B1 ARID2 BCL2 C3AR1 CBX3 CCT5 CDK4 CKS2 CRTC2 CYLD DLL1 ABCD1 AKR1C3 ARMC1 BCL2A1 C5 CBX5 CCT6A CDK5 CLCA2 CRY1 CYP19A1 DLL3 ABCD3 AKT1 ARNT BCL2L1 C5AR1 CCBL2 CCT6B CDK5R1 CLCF1 CRYAA CYP1A1 DLL4 -

Table S1. 103 Ferroptosis-Related Genes Retrieved from the Genecards
Table S1. 103 ferroptosis-related genes retrieved from the GeneCards. Gene Symbol Description Category GPX4 Glutathione Peroxidase 4 Protein Coding AIFM2 Apoptosis Inducing Factor Mitochondria Associated 2 Protein Coding TP53 Tumor Protein P53 Protein Coding ACSL4 Acyl-CoA Synthetase Long Chain Family Member 4 Protein Coding SLC7A11 Solute Carrier Family 7 Member 11 Protein Coding VDAC2 Voltage Dependent Anion Channel 2 Protein Coding VDAC3 Voltage Dependent Anion Channel 3 Protein Coding ATG5 Autophagy Related 5 Protein Coding ATG7 Autophagy Related 7 Protein Coding NCOA4 Nuclear Receptor Coactivator 4 Protein Coding HMOX1 Heme Oxygenase 1 Protein Coding SLC3A2 Solute Carrier Family 3 Member 2 Protein Coding ALOX15 Arachidonate 15-Lipoxygenase Protein Coding BECN1 Beclin 1 Protein Coding PRKAA1 Protein Kinase AMP-Activated Catalytic Subunit Alpha 1 Protein Coding SAT1 Spermidine/Spermine N1-Acetyltransferase 1 Protein Coding NF2 Neurofibromin 2 Protein Coding YAP1 Yes1 Associated Transcriptional Regulator Protein Coding FTH1 Ferritin Heavy Chain 1 Protein Coding TF Transferrin Protein Coding TFRC Transferrin Receptor Protein Coding FTL Ferritin Light Chain Protein Coding CYBB Cytochrome B-245 Beta Chain Protein Coding GSS Glutathione Synthetase Protein Coding CP Ceruloplasmin Protein Coding PRNP Prion Protein Protein Coding SLC11A2 Solute Carrier Family 11 Member 2 Protein Coding SLC40A1 Solute Carrier Family 40 Member 1 Protein Coding STEAP3 STEAP3 Metalloreductase Protein Coding ACSL1 Acyl-CoA Synthetase Long Chain Family Member 1 Protein -
Supplementary Table S1. List of All the Proteins Identified by Itraq Analysis
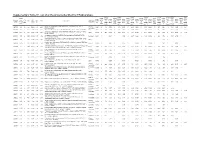
Supplementary Table S1. List of all the proteins identified by iTRAQ analysis. OVSA OVISE OVMA RMG- JHOS4 OVCA OVSA SKOV Seque OVISE OVMA RMG- JHOS4 OVCA OVSA HO/H SKOV # OVISE /HOSE OVMA NA/HO RMG- I/HOS JHOS4 /HOSE OVCA R3/HO HO/H SKOV 3/HOS Accession nce MW calc. Subcellular /HOSE NA/HO I/HOS /HOSE R3/HO HO/H OSE2 3/HOS Pept # AAs Score Protein name /HOSE 2C NA/HO SE2C I/HOS E2C /HOSE 2C R3/HO SE2C OSE2 3/HOS E2C number covera [kDa] pI localization 2C SE2C E2C 2C SE2C OSE2 C E2C ides 2C Variabi SE2C Variabi E2C Variabi 2C Variabi SE2C Variabi C E2C Variabi ge(%) Count Count Count Count Count C Variabi Count lity [%] lity [%] lity [%] lity [%] lity [%] Count lity [%] lity [%] Extended synaptotagmin-2 OS=Homo sapiens GN=ESYT2 PE=1 SV=1 - Plasma A0FGR8 13.9 10 921 102.29 9.26 421.7 1.043 12 19.8 0.758 9 15.3 0.969 11 43.5 1.080 11 27.3 0.800 10 34.7 3.281 12 74.1 1.430 9 38.6 [ESYT2_HUMAN] membrane A0MZ66 3.65 2 631 71.60 5.33 49.5 Shootin-1 OS=Homo sapiens GN=KIAA1598 PE=1 SV=4 - [SHOT1_HUMAN] Other 2.515 3 33.6 1.495 3 13.1 1.985 2 56.9 1.684 3 5.4 1.561 3 31.4 1.881 3 22.2 2.783 3 32.1 Acetolactate synthase-like protein OS=Homo sapiens GN=ILVBL PE=1 SV=2 - A1L0T0 10.13 5 632 67.82 8.15 231.2 Other 0.820 4 20.3 0.675 4 37.0 0.833 4 37.6 0.880 4 44.3 0.789 4 37.8 3.677 4 78.5 0.929 4 13.0 [ILVBL_HUMAN] Uncharacterized protein KIAA0564 OS=Homo sapiens GN=KIAA0564 PE=1 A3KMH1 1.15 2 1905 214.69 7.40 30.9 Secreted 0.934 1 0.661 1 1.650 2 28.7 1.928 2 18.0 0.949 2 38.8 1.748 2 10.7 2.450 1 SV=2 - [K0564_HUMAN] WD repeat-containing protein -

Analysis of the Expression and Single-Nucleotide Variant Frequencies of the Buyrophilin-Like 2 Gene in Patients with Uveal Melanoma
Supplementary Online Content Amaro A, Parodi F, Diedrich K, et al. Analysis of the expression and single-nucleotide variant frequencies of the buyrophilin-like 2 gene in patients with uveal melanoma. JAMA Ophthalmol. Published online August 11, 2016. doi: 10.1001/jamaophthalmol.2016.2691. eTable 1. M1- and M2-poloarization genes eTable 2. M1- and M2-polarization genes that are associated with disease-free survival of patients with uveal melanoma This supplementary material has been provided by the authors to give readers additional information about their work. © 2016 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/30/2021 eTable 1. M1- and M2-poloarization genes 203308_x NM_000195 | HPS1 3257 Hs.40456 203308_x 10 GO:00070 - AI185798 Hermansky-Pudlak syndrome 1 chr10:100 1E+08 1E+08 -1.13131 6.095084 0.859709 0.14105 1.819564 205022_s NM_001085471 FOXN3 1112 Hs.43428 205022_s 14 GO:00000 - NM_0051 forkhead box N3 chr14:896 89622516 90085494 -0.83339 6.106332 1.983495 0.324826 3.850649 204226_a NM_001164380 STAU2 27067 Hs.56181 204226_a 8 GO:00068 - NM_0143 staufen, RNA binding protein, chr8:7446 74461843 74659943 -0.95841 6.106973 0.850648 0.139291 1.804766 208639_x NM_005742 | PDIA6 10130 Hs.21210 208639_x 2 GO:00064 - BC001312 protein disulfide isomerase chr2:1092 10923518 10952960 -0.37258 6.110976 1.043652 0.170783 2.061971 204295_a NA NA NA NA 204295_a NA NA NA NM_0031 NA chrNA:-1-- -1 -1 -0.94773 6.113623 0.686679 0.112319 1.613194 202609_a NM_004447 | EPS8 2059 Hs.59116 202609_a -

Clarke, Cassie J. (2015) an Investigation Into the Role of the Initiator Methionine Transfer RNA in Cell Migration and Tumour Growth
Clarke, Cassie J. (2015) An investigation into the role of the initiator methionine transfer RNA in cell migration and tumour growth. PhD thesis. http://theses.gla.ac.uk/6913/ Copyright and moral rights for this work are retained by the author A copy can be downloaded for personal non-commercial research or study, without prior permission or charge This work cannot be reproduced or quoted extensively from without first obtaining permission in writing from the author The content must not be changed in any way or sold commercially in any format or medium without the formal permission of the author When referring to this work, full bibliographic details including the author, title, awarding institution and date of the thesis must be given Enlighten:Theses http://theses.gla.ac.uk/ [email protected] An investigation into the role of the initiator methionine transfer RNA in cell migration and tumour growth Cassie J. Clarke M.Sci. Submitted in fulfilment of the requirements for the Degree of Doctor of Philosophy Institute of Cancer Sciences College of Medical, Veterinary and Life Sciences University of Glasgow September 2015 2 Abstract Control of cellular tRNA repertoires can drive specific programmes of translation Met to favour the maintenance of proliferative or differentiated phenotypes. tRNAi is the initiator methionine tRNA, responsible for recognising the start codon and Met initiating translation. We have investigated how increased expression of tRNAi can influence cell behaviour, using both immortalised cell lines in vitro and mouse models in vivo. Met Levels of tRNAi are increased in carcinoma-associated fibroblasts compared to Met normal fibroblasts.