Composition, Taxonomy and Functional Diversity of the Oropharynx Microbiome in Individuals with Schizophrenia and Controls Eduardo Castro-Nallar1,6 , Matthew L
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thesis Final
THESIS/DISSERTATION APPROVED BY 4-24-2020 Barbara J. O’Kane Date Barbara J. O’Kane, MS, Ph.D, Chair Margaret Jergenson Margret A. Jergenson, DDS Neil Norton Neil S. Norton, BA, Ph.D. Gail M. Jensen, Ph.D., Dean i COMPARISON OF PERIODONTIUM AMONG SUBJECTS TREATED WITH CLEAR ALIGNERS AND CONVENTIONAL ORTHODONTICS By: Mark S. Jones A THESIS Presented to the Faculty of The Graduate College at Creighton University In Partial Fulfillment of Requirements For the Degree of Master of Science in the Department of Oral Biology Under the Supervision of Dr. Marcelo Mattos Advising from: Dr. Margaret Jergenson, Dr. Neil S. Norton, and Dr. Barbara O’Kane Omaha, Nebraska 2020 i iii Abstract INTRODUCTION: With the wider therapeutic use of clear aligners the need to investigate the periodontal health status and microbiome of clear aligners’ patients in comparison with users of fixed orthodontic has arisen and is the objective of this thesis. METHODS: A clinical periodontal evaluation was performed, followed by professional oral hygiene treatment on a patient under clear aligner treatment, another under fixed orthodontics and two controls that never received any orthodontic therapy. One week after, supragingival plaque, swabs from the orthodontic devices, and saliva samples were collected from each volunteer for further 16s sequencing and microbiome analysis. RESULTS: All participants have overall good oral hygiene. However, our results showed increases in supragingival plaque, higher number of probing depths greater than 3mm, higher number of bleeding sites on probing, and a higher amount of gingival recession in the subject treated with fixed orthodontics. A lower bacterial count was observed colonizing the clear aligners, with less diversity than the other samples analyzed. -

Rothia Dentocariosa Endophthalmitis Following Intravitreal Injection—A Case Report R
Hayes et al. Journal of Ophthalmic Inflammation and Infection (2017) 7:24 Journal of Ophthalmic DOI 10.1186/s12348-017-0142-3 Inflammation and Infection LETTERTOTHEEDITOR Open Access Rothia dentocariosa endophthalmitis following intravitreal injection—a case report R. A. Hayes1,2* , H. Y. Bennett1,2 and S. O’Hagan2,3 Abstract Purpose: This report describes the first recognised case of Rothia dentocariosa endophthalmitis following intravitreal injection. Case report: A 57-year-old indigenous Australian diabetic female developed pain, redness and decreased vision 3 days after intravitreal aflibercept injection to the right eye—administered for diabetic vitreous haemorrhage with suspected macular oedema and proliferative diabetic retinopathy. Examination revealed best corrected visual acuity (BCVA) of hand movements, ocular hypertension and marked anterior chamber inflammation. The left eye was unaffected but had a BCVA of 6/24 due to pre-existing diabetic retinopathy. Vitreous culture isolated Rothia dentocariosa as the organism responsible for the endophthalmitis. The following treatment with intraocular cephazolin, vancomycin and ceftazidime, topical ciprofloxacin and gentamicin and systemic ciprofloxacin, the patient underwent vitrectomy. Nine weeks after onset, the patient’s BCVA had improved to 6/36, and fundal examination revealed extensive retinal necrosis. Conclusion: Rothia dentocariosa is presented as a rare cause of endophthalmitis following intravitreal injection and reports the appearance of ‘pink hypopyon’ previously observed with other organisms. Its identification also demonstrates the risk of oral bacterial contamination during intraocular injections. Vigilance with strategies to minimise bacterial contamination in the peri-injection period are important. Further research to identify additional techniques to prevent contamination with oral bacteria would be beneficial, including whether a role exists for patients wearing surgical masks during intravitreal injections. -
Genus Contributing to the Top 70% of Significant Dissimilarity of Bacteria Between Day 7 and 18 Age Groups As Determined by SIMPER
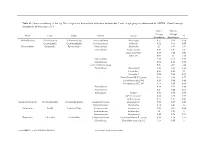
Table S1: Genus contributing to the top 70% of significant dissimilarity of bacteria between day 7 and 18 age groups as determined by SIMPER. Overall average dissimilarity between ages is 51%. Day 7 Day 18 Average Average Phyla Class Order Family Genus % Abundance Abundance Actinobacteria Actinobacteria Actinomycetales Actinomycetaceae Actinomyces 0.57 0.24 0.74 Coriobacteriia Coriobacteriales Coriobacteriaceae Collinsella 0.51 0.61 0.57 Bacteroidetes Bacteroidia Bacteroidales Bacteroidaceae Bacteroides 2.1 1.63 1.03 Marinifilaceae Butyricimonas 0.82 0.81 0.9 Sanguibacteroides 0.08 0.42 0.59 CAG-873 0.01 1.1 1.68 Marinifilaceae 0.38 0.78 0.91 Marinifilaceae 0.78 1.04 0.97 p-2534-18B5 gut group 0.06 0.7 1.04 Prevotellaceae Alloprevotella 0.46 0.83 0.89 Prevotella 2 0.95 1.11 1.3 Prevotella 7 0.22 0.42 0.56 Prevotellaceae NK3B31 group 0.62 0.68 0.77 Prevotellaceae UCG-003 0.26 0.64 0.89 Prevotellaceae UCG-004 0.11 0.48 0.68 Prevotellaceae 0.64 0.52 0.89 Prevotellaceae 0.27 0.42 0.55 Rikenellaceae Alistipes 0.39 0.62 0.77 dgA-11 gut group 0.04 0.38 0.56 RC9 gut group 0.79 1.17 0.95 Epsilonbacteraeota Campylobacteria Campylobacterales Campylobacteraceae Campylobacter 0.58 0.83 0.97 Helicobacteraceae Helicobacter 0.12 0.41 0.6 Firmicutes Bacilli Lactobacillales Enterococcaceae Enterococcus 0.36 0.31 0.64 Lactobacillaceae Lactobacillus 1.4 1.24 1 Streptococcaceae Streptococcus 0.82 0.58 0.53 Firmicutes Clostridia Clostridiales Christensenellaceae Christensenellaceae R-7 group 0.38 1.36 1.56 Clostridiaceae Clostridium sensu stricto 1 1.16 0.58 -

INFECTIOUS DISEASES NEWSLETTER May 2017 T. Herchline, Editor LOCAL NEWS ID Fellows Our New Fellow Starting in July Is Dr. Najmus
INFECTIOUS DISEASES NEWSLETTER May 2017 T. Herchline, Editor LOCAL NEWS ID Fellows Our new fellow starting in July is Dr. Najmus Sahar. Dr. Sahar graduated from Dow Medical College in Pakistan in 2009. She works in Dayton, OH and completed residency training from the Wright State University Internal Medicine Residency Program in 2016. She is married to Dr. Asghar Ali, a hospitalist in MVH and mother of 3 children Fawad, Ebaad and Hammad. She spends most of her spare time with family in outdoor activities. Dr Alpa Desai will be at Miami Valley Hospital in May and June, and at the VA Medical Center in July. Dr Luke Onuorah will be at the VA Medical Center in May and June, and at Miami Valley Hospital in July. Dr. Najmus Sahar will be at MVH in July. Raccoon Rabies Immune Barrier Breach, Stark County Two raccoons collected this year in Stark County have been confirmed by the Centers of Disease Control and Prevention to be infected with the raccoon rabies variant virus. These raccoons were collected outside the Oral Rabies Vaccination (ORV) zone and represent the first breach of the ORV zone since a 2004 breach in Lake County. In 1997, a new strain of rabies in wild raccoons was introduced into northeastern Ohio from Pennsylvania. The Ohio Department of Health and other partner agencies implemented a program to immunize wild raccoons for rabies using an oral rabies vaccine. This effort created a barrier of immune animals that reduced animal cases and prevented the spread of raccoon rabies into the rest of Ohio. -

A New Symbiotic Lineage Related to Neisseria and Snodgrassella Arises from the Dynamic and Diverse Microbiomes in Sucking Lice
bioRxiv preprint doi: https://doi.org/10.1101/867275; this version posted December 6, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. A new symbiotic lineage related to Neisseria and Snodgrassella arises from the dynamic and diverse microbiomes in sucking lice Jana Říhová1, Giampiero Batani1, Sonia M. Rodríguez-Ruano1, Jana Martinů1,2, Eva Nováková1,2 and Václav Hypša1,2 1 Department of Parasitology, Faculty of Science, University of South Bohemia, České Budějovice, Czech Republic 2 Institute of Parasitology, Biology Centre, ASCR, v.v.i., České Budějovice, Czech Republic Author for correspondence: Václav Hypša, Department of Parasitology, University of South Bohemia, České Budějovice, Czech Republic, +42 387 776 276, [email protected] Abstract Phylogenetic diversity of symbiotic bacteria in sucking lice suggests that lice have experienced a complex history of symbiont acquisition, loss, and replacement during their evolution. By combining metagenomics and amplicon screening across several populations of two louse genera (Polyplax and Hoplopleura) we describe a novel louse symbiont lineage related to Neisseria and Snodgrassella, and show its' independent origin within dynamic lice microbiomes. While the genomes of these symbionts are highly similar in both lice genera, their respective distributions and status within lice microbiomes indicate that they have different functions and history. In Hoplopleura acanthopus, the Neisseria-related bacterium is a dominant obligate symbiont universally present across several host’s populations, and seems to be replacing a presumably older and more degenerated obligate symbiont. -

Case Report Prosthetic Hip Joint Infection Caused by Rothia Dentocariosa
Int J Clin Exp Med 2015;8(7):11628-11631 www.ijcem.com /ISSN:1940-5901/IJCEM0010162 Case Report Prosthetic hip joint infection caused by Rothia dentocariosa Fırat Ozan1, Eyyüp Sabri Öncel1, Fuat Duygulu1, İlhami Çelik2, Taşkın Altay3 ¹Department of Orthopedics and Traumatology, Kayseri Training and Research Hospital, Kayseri, Turkey; ²Department of Clinical Microbiology and Infectious Diseases, Kayseri Training and Research Hospital, Kayseri, Turkey; ³Department of Orthopedics and Traumatology, İzmir Bozyaka Training and Research Hospital, İzmir, Turkey Received May 12, 2015; Accepted June 26, 2015; Epub July 15, 2015; Published July 30, 2015 Abstract: Rothia dentocariosa is an aerobic, pleomorphic, catalase-positive, non-motile, gram-positive bacteria that is a part of the normal flora in the oral cavity and respiratory tract. Although it is a rare cause of systemic infection, it may be observed in immunosuppressed individuals. Here we report the case of an 85-year old man who developed prosthetic joint infection that was caused by R. dentocariosa after hemiarthroplasty. This is the first case report of a prosthetic hip joint infection caused by R. dentocariosa in the literature. Keywords: Hip arthroplasty, infection, Rothia dentocariosa, joint, prosthetic, treatment Introduction resulting from a fall. Swelling in the right lower extremity, pain during rest, erythema at the inci- Rothia dentocariosa is an aerobic, pleomorph- sion site and drainage developed 2 weeks after ic, catalase-positive, non-motile, gram positive surgery. The laboratory evaluations revealed bacteria that is a part of the normal flora in the the following results: C-reactive protein (CRP), oral cavity and respiratory tract [1, 2]. The 178 mg/L; erythrocyte sedimentation rate organism resembles Nocardia and Actinomyces (ESR), 90 mm/h; white blood cell (WBC), 7.79 × species but it differs in terms of the cell wall 103/µL. -
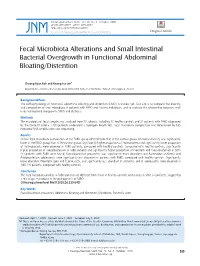
Fecal Microbiota Alterations and Small Intestinal Bacterial Overgrowth in Functional Abdominal Bloating/Distention
J Neurogastroenterol Motil, Vol. 26 No. 4 October, 2020 pISSN: 2093-0879 eISSN: 2093-0887 https://doi.org/10.5056/jnm20080 JNM Journal of Neurogastroenterology and Motility Original Article Fecal Microbiota Alterations and Small Intestinal Bacterial Overgrowth in Functional Abdominal Bloating/Distention Choong-Kyun Noh and Kwang Jae Lee* Department of Gastroenterology, Ajou University School of Medicine, Suwon, Gyeonggi-do, Korea Background/Aims The pathophysiology of functional abdominal bloating and distention (FABD) is unclear yet. Our aim is to compare the diversity and composition of fecal microbiota in patients with FABD and healthy individuals, and to evaluate the relationship between small intestinal bacterial overgrowth (SIBO) and dysbiosis. Methods The microbiota of fecal samples was analyzed from 33 subjects, including 12 healthy controls and 21 patients with FABD diagnosed by the Rome IV criteria. FABD patients underwent a hydrogen breath test. Fecal microbiota composition was determined by 16S ribosomal RNA amplification and sequencing. Results Overall fecal microbiota composition of the FABD group differed from that of the control group. Microbial diversity was significantly lower in the FABD group than in the control group. Significantly higher proportion of Proteobacteria and significantly lower proportion of Actinobacteria were observed in FABD patients, compared with healthy controls. Compared with healthy controls, significantly higher proportion of Faecalibacterium in FABD patients and significantly higher proportion of Prevotella and Faecalibacterium in SIBO (+) patients with FABD were found. Faecalibacterium prausnitzii, was significantly more abundant, but Bacteroides uniformis and Bifidobacterium adolescentis were significantly less abundant in patients with FABD, compared with healthy controls. Significantly more abundant Prevotella copri and F. -

Bacterial Diversity and Functional Analysis of Severe Early Childhood
www.nature.com/scientificreports OPEN Bacterial diversity and functional analysis of severe early childhood caries and recurrence in India Balakrishnan Kalpana1,3, Puniethaa Prabhu3, Ashaq Hussain Bhat3, Arunsaikiran Senthilkumar3, Raj Pranap Arun1, Sharath Asokan4, Sachin S. Gunthe2 & Rama S. Verma1,5* Dental caries is the most prevalent oral disease afecting nearly 70% of children in India and elsewhere. Micro-ecological niche based acidifcation due to dysbiosis in oral microbiome are crucial for caries onset and progression. Here we report the tooth bacteriome diversity compared in Indian children with caries free (CF), severe early childhood caries (SC) and recurrent caries (RC). High quality V3–V4 amplicon sequencing revealed that SC exhibited high bacterial diversity with unique combination and interrelationship. Gracillibacteria_GN02 and TM7 were unique in CF and SC respectively, while Bacteroidetes, Fusobacteria were signifcantly high in RC. Interestingly, we found Streptococcus oralis subsp. tigurinus clade 071 in all groups with signifcant abundance in SC and RC. Positive correlation between low and high abundant bacteria as well as with TCS, PTS and ABC transporters were seen from co-occurrence network analysis. This could lead to persistence of SC niche resulting in RC. Comparative in vitro assessment of bioflm formation showed that the standard culture of S. oralis and its phylogenetically similar clinical isolates showed profound bioflm formation and augmented the growth and enhanced bioflm formation in S. mutans in both dual and multispecies cultures. Interaction among more than 700 species of microbiota under diferent micro-ecological niches of the human oral cavity1,2 acts as a primary defense against various pathogens. Tis has been observed to play a signifcant role in child’s oral and general health. -

Oral and Fecal Campylobacter Concisus Strains Perturb Barrier Function by Apoptosis Induction in HT-29/B6 Intestinal Epithelial Cells
Oral and Fecal Campylobacter concisus Strains Perturb Barrier Function by Apoptosis Induction in HT-29/B6 Intestinal Epithelial Cells Hans Linde Nielsen1, Henrik Nielsen1, Tove Ejlertsen2, Jørgen Engberg3, Dorothee Gu¨ nzel4, Martin Zeitz5, Nina A. Hering5, Michael Fromm4,Jo¨ rg-Dieter Schulzke5*, Roland Bu¨ cker5 1 Department of Infectious Diseases, Aalborg Hospital, Aarhus University Hospital, Aalborg, Denmark, 2 Department of Clinical Microbiology, Aalborg Hospital, Aarhus University Hospital, Aalborg, Denmark, 3 Department of Clinical Microbiology, Slagelse Hospital, Slagelse, Denmark, 4 Institute of Clinical Physiology, Charite´ Universita¨tsmedizin Berlin, Berlin, Germany, 5 Department of Gastroenterology, Infectious Diseases and Rheumatology, Division of General Medicine and Nutrition, Charite´ Universita¨tsmedizin Berlin, Berlin, Germany Abstract Campylobacter concisus infections of the gastrointestinal tract can be accompanied by diarrhea and inflammation, whereas colonization of the human oral cavity might have a commensal nature. We focus on the pathophysiology of C. concisus and the effects of different clinical oral and fecal C. concisus strains on human HT-29/B6 colon cells. Six oral and eight fecal strains of C. concisus were isolated. Mucus-producing HT-29/B6 epithelial monolayers were infected with the C. concisus strains. Transepithelial electrical resistance (Rt) and tracer fluxes of different molecule size were measured in Ussing chambers. Tight junction (TJ) protein expression was determined by Western blotting, and subcellular TJ distribution was analyzed by confocal laser-scanning microscopy. Apoptosis induction was examined by TUNEL-staining and Western blot of caspase-3 activation. All strains invaded confluent HT-29/B6 cells and impaired epithelial barrier function, characterized by a time- and dose-dependent decrease in Rt either after infection from the apical side but even more from the basolateral compartment. -

Bacteriophages As Potential New Mammalian Pathogens George V
www.nature.com/scientificreports OPEN Bacteriophages as potential new mammalian pathogens George V. Tetz 1, Kelly V. Ruggles2,3, Hua Zhou3, Adriana Heguy4,5,6, Aristotelis Tsirigos3,4,5 & Victor Tetz1 Received: 4 May 2017 Increased intestinal permeability and translocation of gut bacteria trigger various polyaetiological Accepted: 23 June 2017 diseases associated with chronic infammation and underlie a variety of poorly treatable pathologies. Published online: 1 August 2017 Previous studies have established a primary role of the microbiota composition and intestinal permeability in such pathologies. Using a rat model, we examined the efects of exposure to a bacteriophage cocktail on intestinal permeability and relative abundance of taxonomic units in the gut bacterial community. There was an increase in markers of impaired gut permeability, such as the lactulose/mannitol ratio, plasma endotoxin concentrations, and serum levels of infammation- related cytokines, following the bacteriophage challenge. We observed signifcant diferences in the alpha diversity of faecal bacterial species and found that richness and diversity index values increased following the bacteriophage challenge. There was a reduction in the abundance of Blautia, Catenibacterium, Lactobacillus, and Faecalibacterium species and an increase in Butyrivibrio, Oscillospira and Ruminococcus after bacteriophage administration. These fndings provide novel insights into the role of bacteriophages as potentially pathogenic for mammals and their possible implication in the development of diseases associated with increased intestinal permeability. Our knowledge of the intestinal microbiota has greatly expanded over the last decade, and growing evidence sug- gests that alterations of the intestinal microbiota are critical pathogenic factors that trigger various polyaetiologi- cal diseases associated with increased intestinal permeability and chronic infammation1–3. -

Metatranscriptomic Analysis to Define the Secrebiome, and 16S Rrna
Gallardo‑Becerra et al. Microb Cell Fact (2020) 19:61 https://doi.org/10.1186/s12934‑020‑01319‑y Microbial Cell Factories RESEARCH Open Access Metatranscriptomic analysis to defne the Secrebiome, and 16S rRNA profling of the gut microbiome in obesity and metabolic syndrome of Mexican children Luigui Gallardo‑Becerra1†, Fernanda Cornejo‑Granados1†, Rodrigo García‑López1†, Alejandra Valdez‑Lara1, Shirley Bikel1, Samuel Canizales‑Quinteros2, Blanca E. López‑Contreras2, Alfredo Mendoza‑Vargas3, Henrik Nielsen4 and Adrián Ochoa‑Leyva1* Abstract Background: In the last decade, increasing evidence has shown that changes in human gut microbiota are asso‑ ciated with diseases, such as obesity. The excreted/secreted proteins (secretome) of the gut microbiota afect the microbial composition, altering its colonization and persistence. Furthermore, it infuences microbiota‑host interac‑ tions by triggering infammatory reactions and modulating the host’s immune response. The metatranscriptome is essential to elucidate which genes are expressed under diseases. In this regard, little is known about the expressed secretome in the microbiome. Here, we use a metatranscriptomic approach to delineate the secretome of the gut microbiome of Mexican children with normal weight (NW) obesity (O) and obesity with metabolic syndrome (OMS). Additionally, we performed the 16S rRNA profling of the gut microbiota. Results: Out of the 115,712 metatranscriptome genes that codifed for proteins, 30,024 (26%) were predicted to be secreted, constituting the Secrebiome of the -

A Genomic Approach to Bacterial Taxonomy: an Examination and Proposed Reclassification of Species Within the Genus Neisseria
Microbiology (2012), 158, 1570–1580 DOI 10.1099/mic.0.056077-0 A genomic approach to bacterial taxonomy: an examination and proposed reclassification of species within the genus Neisseria Julia S. Bennett,1 Keith A. Jolley,1 Sarah G. Earle,1 Craig Corton,2 Stephen D. Bentley,2 Julian Parkhill2 and Martin C. J. Maiden1 Correspondence 1Department of Zoology, University of Oxford, Oxford OX1 3PS, UK Julia S. Bennett 2The Wellcome Trust Sanger Institute, Wellcome Trust Genome Campus, Hinxton CB10 1SA, UK [email protected] In common with other bacterial taxa, members of the genus Neisseria are classified using a range of phenotypic and biochemical approaches, which are not entirely satisfactory in assigning isolates to species groups. Recently, there has been increasing interest in using nucleotide sequences for bacterial typing and taxonomy, but to date, no broadly accepted alternative to conventional methods is available. Here, the taxonomic relationships of 55 representative members of the genus Neisseria have been analysed using whole-genome sequence data. As genetic material belonging to the accessory genome is widely shared among different taxa but not present in all isolates, this analysis indexed nucleotide sequence variation within sets of genes, specifically protein-coding genes that were present and directly comparable in all isolates. Variation in these genes identified seven species groups, which were robust to the choice of genes and phylogenetic clustering methods used. The groupings were largely, but not completely, congruent with current species designations, with some minor changes in nomenclature and the reassignment of a few isolates necessary. In particular, these data showed that isolates classified as Neisseria polysaccharea are polyphyletic and probably include more than one taxonomically distinct organism.