Treatment of Hyponatremia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Specifications of Approved Drug Compound Library
Annexure-I : Specifications of Approved drug compound library The compounds should be structurally diverse, medicinally active, and cell permeable Compounds should have rich documentation with structure, Target, Activity and IC50 should be known Compounds which are supplied should have been validated by NMR and HPLC to ensure high purity Each compound should be supplied as 10mM solution in DMSO and at least 100µl of each compound should be supplied. Compounds should be supplied in screw capped vial arranged as 96 well plate format. -

Lithium Carbonate
Right to Know Hazardous Substance Fact Sheet Common Name: LITHIUM CARBONATE Synonyms: Dilithium Carbonate; Carbolith CAS Number: 554-13-2 Chemical Name: Carbonic Acid, Dilithium Salt RTK Substance Number: 1124 Date: September 1998 Revision: January 2008 DOT Number: None Description and Use EMERGENCY RESPONDERS >>>> SEE BACK PAGE Lithium Carbonate is a white, light, odorless powder. It is Hazard Summary used in the production of glazes on ceramics and porcelain, in Hazard Rating NJDOH NFPA varnishes and dyes, as a coating on arc welding electrodes, HEALTH 1 - and in lubricating greases. It is also used as medication to FLAMMABILITY 0 - treat certain types of mental illness. REACTIVITY 0 - TERATOGEN POISONOUS GASES ARE PRODUCED IN FIRE Hazard Rating Key: 0=minimal; 1=slight; 2=moderate; 3=serious; 4=severe Reasons for Citation f Lithium Carbonate is on the Right to Know Hazardous f Lithium Carbonate can affect you when inhaled. Substance List because it is cited by DEP and EPA. f Lithium Carbonate may be a TERATOGEN. HANDLE f This chemical is on the Special Health Hazard Substance List. WITH EXTREME CAUTION. f Contact can irritate the skin and eyes. f Inhaling Lithium Carbonate can irritate the nose and throat. f Lithium Carbonate can cause nausea, vomiting, diarrhea and abdominal pain. f Inhaling Lithium Carbonate can irritate the lungs. Higher exposures may cause a build-up of fluid in the lungs SEE GLOSSARY ON PAGE 5. (pulmonary edema), a medical emergency. f Lithium Carbonate can cause headache, muscle FIRST AID weakness, confusion, seizures and coma. Eye Contact f Lithium Carbonate may cause a skin allergy. -

Lithium Carbonate
SAFETY DATA SHEET Creation Date 26-Sep-2009 Revision Date 18-Jan-2018 Revision Number 3 1. Identification Product Name Lithium Carbonate Cat No. : L119-500 CAS-No 554-13-2 Synonyms carbonic acid lithium salt; Carbonic Acid Dilithium Salt Recommended Use Laboratory chemicals. Uses advised against Not for food, drug, pesticide or biocidal product use Details of the supplier of the safety data sheet Company Fisher Scientific One Reagent Lane Fair Lawn, NJ 07410 Tel: (201) 796-7100 Emergency Telephone Number CHEMTRECÒ, Inside the USA: 800-424-9300 CHEMTRECÒ, Outside the USA: 001-703-527-3887 2. Hazard(s) identification Classification This chemical is considered hazardous by the 2012 OSHA Hazard Communication Standard (29 CFR 1910.1200) Acute oral toxicity Category 4 Skin Corrosion/irritation Category 2 Serious Eye Damage/Eye Irritation Category 1 Specific target organ toxicity (single exposure) Category 3 Target Organs - Respiratory system, Central nervous system (CNS). Label Elements Signal Word Danger Hazard Statements Harmful if swallowed Causes skin irritation Causes serious eye damage May cause respiratory irritation ______________________________________________________________________________________________ Page 1 / 7 Lithium Carbonate Revision Date 18-Jan-2018 ______________________________________________________________________________________________ Precautionary Statements Prevention Wash face, hands and any exposed skin thoroughly after handling Do not eat, drink or smoke when using this product Wear protective gloves/protective clothing/eye protection/face protection Avoid breathing dust/fume/gas/mist/vapors/spray Use only outdoors or in a well-ventilated area Inhalation IF INHALED: Remove victim to fresh air and keep at rest in a position comfortable for breathing Call a POISON CENTER or doctor/physician if you feel unwell Skin IF ON SKIN: Wash with plenty of soap and water If skin irritation occurs: Get medical advice/attention Take off contaminated clothing and wash before reuse Eyes IF IN EYES: Rinse cautiously with water for several minutes. -
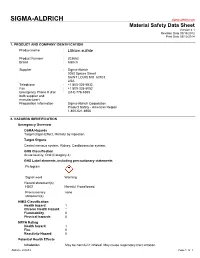
Lithium Sulfate
SIGMA-ALDRICH sigma-aldrich.com Material Safety Data Sheet Version 4.1 Revision Date 09/14/2012 Print Date 03/12/2014 1. PRODUCT AND COMPANY IDENTIFICATION Product name : Lithium sulfate Product Number : 203653 Brand : Aldrich Supplier : Sigma-Aldrich 3050 Spruce Street SAINT LOUIS MO 63103 USA Telephone : +1 800-325-5832 Fax : +1 800-325-5052 Emergency Phone # (For : (314) 776-6555 both supplier and manufacturer) Preparation Information : Sigma-Aldrich Corporation Product Safety - Americas Region 1-800-521-8956 2. HAZARDS IDENTIFICATION Emergency Overview OSHA Hazards Target Organ Effect, Harmful by ingestion. Target Organs Central nervous system, Kidney, Cardiovascular system. GHS Classification Acute toxicity, Oral (Category 4) GHS Label elements, including precautionary statements Pictogram Signal word Warning Hazard statement(s) H302 Harmful if swallowed. Precautionary none statement(s) HMIS Classification Health hazard: 1 Chronic Health Hazard: * Flammability: 0 Physical hazards: 0 NFPA Rating Health hazard: 1 Fire: 0 Reactivity Hazard: 0 Potential Health Effects Inhalation May be harmful if inhaled. May cause respiratory tract irritation. Aldrich - 203653 Page 1 of 7 Skin Harmful if absorbed through skin. May cause skin irritation. Eyes May cause eye irritation. Ingestion Harmful if swallowed. 3. COMPOSITION/INFORMATION ON INGREDIENTS Formula : Li2O4S Molecular Weight : 109.94 g/mol Component Concentration Lithium sulphate CAS-No. 10377-48-7 - EC-No. 233-820-4 4. FIRST AID MEASURES General advice Move out of dangerous area.Consult a physician. Show this safety data sheet to the doctor in attendance. If inhaled If breathed in, move person into fresh air. If not breathing, give artificial respiration. Consult a physician. -

Therapeutic Potential of Vasopressin-Receptor Antagonists in Heart Failure
J Pharmacol Sci 124, 1 – 6 (2014) Journal of Pharmacological Sciences © The Japanese Pharmacological Society Current Perspective Therapeutic Potential of Vasopressin-Receptor Antagonists in Heart Failure Yasukatsu Izumi1,*, Katsuyuki Miura2, and Hiroshi Iwao1 1Department of Pharmacology, 2Applied Pharmacology and Therapeutics, Osaka City University Medical School, Osaka 545-8585, Japan Received October 2, 2013; Accepted November 17, 2013 Abstract. Arginine vasopressin (AVP) is a 9-amino acid peptide that is secreted from the posterior pituitary in response to high plasma osmolality and hypotension. AVP has important roles in circulatory and water homoeostasis, which are mediated by oxytocin receptors and by AVP receptor subtypes: V1a (mainly vascular), V1b (pituitary), and V2 (renal). Vaptans are orally and intravenously active nonpeptide vasopressin-receptor antagonists. Recently, subtype-selective nonpeptide vasopressin-receptor agonists have been developed. A selective V1a-receptor antago- nist, relcovaptan, has shown initial positive results in the treatment of Raynaud’s disease, dysmen- orrhea, and tocolysis. A selective V1b-receptor antagonist, nelivaptan, has beneficial effects in the treatment of psychiatric disorders. Selective V2-receptor antagonists including mozavaptan, lixivaptan, satavaptan, and tolvaptan induce highly hypotonic diuresis without substantially affecting the excretion of electrolytes. A nonselective V1a/V2-receptor antagonist, conivaptan, is used in the treatment for euvolaemic or hypervolemic hyponatremia. Recent basic and clinical studies have shown that AVP-receptor antagonists, especially V2-receptor antagonists, may have therapeutic potential for heart failure. This review presents current information about AVP and its antagonists. Keywords: arginine vasopressin, diuretic, heart failure, vasopressin receptor antagonist 1. Introduction receptor blockers, diuretics, b-adrenoceptor blockers, digitalis glycosides, and inotropic agents (4). -

Management and Treatment of Lithium-Induced Nephrogenic Diabetes Insipidus
REVIEW Management and treatment of lithium- induced nephrogenic diabetes insipidus Christopher K Finch†, Lithium carbonate is a well documented cause of nephrogenic diabetes insipidus, with as Tyson WA Brooks, many as 10 to 15% of patients taking lithium developing this condition. Clinicians have Peggy Yam & Kristi W Kelley been well aware of lithium toxicity for many years; however, the treatment of this drug- induced condition has generally been remedied by discontinuation of the medication or a †Author for correspondence Methodist University reduction in dose. For those patients unresponsive to traditional treatment measures, Hospital, Department several pharmacotherapeutic regimens have been documented as being effective for the of Pharmacy, University of management of lithium-induced diabetes insipidus including hydrochlorothiazide, Tennessee, College of Pharmacy, 1265 Union Ave., amiloride, indomethacin, desmopressin and correction of serum lithium levels. Memphis, TN 38104, USA Tel.: +1 901 516 2954 Fax: +1 901 516 8178 [email protected] Lithium carbonate is well known for its wide use associated with a mutation(s) of vasopressin in bipolar disorders due to its mood stabilizing receptors. Acquired causes are tubulointerstitial properties. It is also employed in aggression dis- disease (e.g., sickle cell disease, amyloidosis, orders, post-traumatic stress disorders, conduct obstructive uropathy), electrolyte disorders (e.g., disorders and even as adjunctive therapy in hypokalemia and hypercalcemia), pregnancy, or depression. Lithium has many well documented conditions induced by a drug (e.g., lithium, adverse effects as well as a relatively narrow ther- demeclocycline, amphotericin B and apeutic range of 0.4 to 0.8 mmol/l. Clinically vincristine) [3,4]. Lithium is the most common significant adverse effects include polyuria, mus- cause of drug-induced nephrogenic DI [5]. -

Patent Application Publication ( 10 ) Pub . No . : US 2019 / 0192440 A1
US 20190192440A1 (19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2019 /0192440 A1 LI (43 ) Pub . Date : Jun . 27 , 2019 ( 54 ) ORAL DRUG DOSAGE FORM COMPRISING Publication Classification DRUG IN THE FORM OF NANOPARTICLES (51 ) Int . CI. A61K 9 / 20 (2006 .01 ) ( 71 ) Applicant: Triastek , Inc. , Nanjing ( CN ) A61K 9 /00 ( 2006 . 01) A61K 31/ 192 ( 2006 .01 ) (72 ) Inventor : Xiaoling LI , Dublin , CA (US ) A61K 9 / 24 ( 2006 .01 ) ( 52 ) U . S . CI. ( 21 ) Appl. No. : 16 /289 ,499 CPC . .. .. A61K 9 /2031 (2013 . 01 ) ; A61K 9 /0065 ( 22 ) Filed : Feb . 28 , 2019 (2013 .01 ) ; A61K 9 / 209 ( 2013 .01 ) ; A61K 9 /2027 ( 2013 .01 ) ; A61K 31/ 192 ( 2013. 01 ) ; Related U . S . Application Data A61K 9 /2072 ( 2013 .01 ) (63 ) Continuation of application No. 16 /028 ,305 , filed on Jul. 5 , 2018 , now Pat . No . 10 , 258 ,575 , which is a (57 ) ABSTRACT continuation of application No . 15 / 173 ,596 , filed on The present disclosure provides a stable solid pharmaceuti Jun . 3 , 2016 . cal dosage form for oral administration . The dosage form (60 ) Provisional application No . 62 /313 ,092 , filed on Mar. includes a substrate that forms at least one compartment and 24 , 2016 , provisional application No . 62 / 296 , 087 , a drug content loaded into the compartment. The dosage filed on Feb . 17 , 2016 , provisional application No . form is so designed that the active pharmaceutical ingredient 62 / 170, 645 , filed on Jun . 3 , 2015 . of the drug content is released in a controlled manner. Patent Application Publication Jun . 27 , 2019 Sheet 1 of 20 US 2019 /0192440 A1 FIG . -

New Approaches of the Hyponatremia Treatment in the Elderly – an Update
FARMACIA, 2020, Vol. 68, 3 https://doi.org/10.31925/farmacia.2020.3.5 REVIEW NEW APPROACHES OF THE HYPONATREMIA TREATMENT IN THE ELDERLY – AN UPDATE ALICE BĂLĂCEANU 1,2#, SECIL OMER 1,2, SILVIU ADRIAN MARINESCU 1,3*, SILVIU MIREL PIȚURU 1#, ȘERBAN DUMITRACHE 2#, DANIELA ELENA POPA 1, ANDREEA ANTONIA GHEORGHE 2, SIRAMONA POPESCU 3, CĂTĂLIN BEJINARIU 3, OCTAV GINGHINĂ 1,2, CARMEN GIUGLEA 1,2 1“Carol Davila” University of Medicine and Pharmacy, 37 Dionisie Lupu Street, 020021, Bucharest, Romania 2“Sf. Ioan” Clinical Emergency Hospital, 13 Vitan-Bârzești Road, 042122, Bucharest, Romania 3“Bagdasar Arseni” Clinical Emergency Hospital, 12 Berceni Road, 041915, Bucharest, Romania *corresponding author: [email protected] #Authors with equal contribution. Manuscript received: December 2019 Abstract Hyponatremia (hNa) is a frequently common imbalance in the elderly hospitalized patients. It is often correlated with elevated plasma quantities of arginine vasopressin (AVP, the antidiuretic hormone) and namely it depicts a water surplus in order to prevail sodium levels. It can conduct, in a comprehensive range, to detrimental changes that can affect the entire health status, especially the central nervous system, thus increasing the mortality and morbidity of hospitalized patients in care units. The inherent treatment of hNa, mainly of the chronic form, requires the correction of serum sodium concentrations at the appropriate rate, because, augmenting it at a warp speed, it can determine permanent or fatal neurologic sequelae. In this regard, the therapy for hNa may be enlightened by egressing therapies that include vasopressin V2 and V1a receptors antagonists, with the principal role of encouraging aquaresis and rise the serum sodium levels, alongside with the electrolyte- sparing discharge of free water. -

The Syndrome of Inappropriate Antidiuretic Hormone: Current and Future Management Options
European Journal of Endocrinology (2010) 162 S13–S18 ISSN 0804-4643 The syndrome of inappropriate antidiuretic hormone: current and future management options Mark Sherlock and Chris J Thompson1 Centre for Endocrinology, Diabetes and Metabolism, School of Clinical and Experimental Medicine, University of Birmingham, Birmingham, B15 2TT, UK and 1Academic Department of Diabetes and Endocrinology, Beaumont Hospital and RCSI Medical School, Beaumont Road, Dublin 9, Ireland (Correspondence should be addressed to C J Thompson; Email: [email protected]) Abstract Hyponatraemia is the commonest electrolyte abnormality, and syndrome of inappropriate antidiuretic hormone (SIADH) is the most frequent underlying pathophysiology. Hyponatraemia is associated with significant morbidity and mortality, and as such appropriate treatment is essential. Treatment options for SIADH include fluid restriction, demeclocycline, urea, frusemide and saline infusion, all of which have their limitations. The introduction of the vasopressin-2 receptor antagonists has allowed clinicians to specifically target the underlying pathophysiology of SIADH. Initial studies have shown good efficacy and safety profiles in the treatment of mild to moderate hyponatraemia. However, studies assessing the efficacy and safety of these agents in acute severe symptomatic hyponatraemia are awaited. Furthermore, the cost of these agents at present may limit their use. European Journal of Endocrinology 162 S13–S18 Introduction diagnosis of SIADH and the differentiation from other causes of hyponatraemia is the first essential step in The previous article in this supplement established determining appropriate treatment. Diagnostic criteria that hyponatraemia due to syndrome of inappropriate for SIADH are included in Table 1 (10). In this article, antidiuretic hormone (SIADH) is associated with we review the existing treatments available for the significant morbidity (1), mortality (2–5) and increased management of SIADH and discuss the potential impact length of hospital stay (6). -

Endocrine Emergencies
Endocrine Emergencies • Neuroendocrine response to Critical illness • Thyroid storm/Myxedema Coma • Adrenal Crisis/Sepsis • Hyper/Hypocalcemia • Hypoglycemia • Hyper and Hyponatremia • Pheochromocytoma crises CASE 76 year old man presents with urosepsis and is Admitted to MICU. He has chronic renal insufficiency. During his hospital course, he is intubated and treated With dopamine. Thyroid studies are performed for Inability to wean from ventilator. What labs do you want? Assessment of Thyroid Function • Hormone Levels: Total T4, Total T3 • Binding proteins: TBG, (T3*) Resin uptake • Free Hormone Levels: TSH, F T4, F T3, Free Thyroid Index, F T4 by Eq Dialysis • Radioactive Iodine uptake (RAIU); primarily for DDx of hyperthyroidism • Thyroid antibodies; TPO, Anti-Thyroglobulin, Thyroid stimulating immunoglobulins, Th receptor antibodies Labs: T4 2.4 ug/dl (5-12) T3U 40% (25-35) FTI 1.0 (1.2-4.2) FT4 0.6 (0.8-1.8) TSH 0.2 uU/ml (.4-5.0) Non-thyroidal illness • Hypothesis: NTI vs 2° Hypothyroidism –RT3 ↑ in NTI and ↓ in Hypothyroidism • Hypothesis: NTI vs Hyperthyroidism – TT3 ↓ in NTI and in ↑ Hyperthyroidism • 75 year old woman with history of hypothyroidism is found unresponsive in her home during a cold spell in houston. No heat in the home. • Exam: T° 95, BP 100/60, P 50, RR 8 • Periorbital edema, neck scar, no rub or gallop, distant heart sounds, crackles at bases, peripheral edema • ECG: Decreased voltage, runs of Torsade de pointes • Labs? Imaging? • CXR: cardiomegaly • Glucose 50 • Na+ 120, K+ 4, Cl 80, HCO3¯ 30 • BUN 30 Creat 1.4 • ABG: pH 7.25, PCO2 75, PO2 80 • CK 600 • Thyroid studies pending • Management: Manifestations of Myxedema Coma • Precipitated by infection, iatrogenic (surgery, sedation, diuretics) • Low thyroid studies • Hypothermia • Altered mental status • Hyponatremia • ↑pCO2 • ↑CK • ↑Catecholamines with ↑vascular resistance • Cardiac: low voltage, Pericardial effusion, impaired relaxation with ↓C.O. -

I Regulations
23.2.2007 EN Official Journal of the European Union L 56/1 I (Acts adopted under the EC Treaty/Euratom Treaty whose publication is obligatory) REGULATIONS COUNCIL REGULATION (EC) No 129/2007 of 12 February 2007 providing for duty-free treatment for specified pharmaceutical active ingredients bearing an ‘international non-proprietary name’ (INN) from the World Health Organisation and specified products used for the manufacture of finished pharmaceuticals and amending Annex I to Regulation (EEC) No 2658/87 THE COUNCIL OF THE EUROPEAN UNION, (4) In the course of three such reviews it was concluded that a certain number of additional INNs and intermediates used for production and manufacture of finished pharmaceu- ticals should be granted duty-free treatment, that certain of Having regard to the Treaty establishing the European Commu- these intermediates should be transferred to the list of INNs, nity, and in particular Article 133 thereof, and that the list of specified prefixes and suffixes for salts, esters or hydrates of INNs should be expanded. Having regard to the proposal from the Commission, (5) Council Regulation (EEC) No 2658/87 of 23 July 1987 on the tariff and statistical nomenclature and on the Common Customs Tariff (1) established the Combined Nomenclature Whereas: (CN) and set out the conventional duty rates of the Common Customs Tariff. (1) In the course of the Uruguay Round negotiations, the Community and a number of countries agreed that duty- (6) Regulation (EEC) No 2658/87 should therefore be amended free treatment should be granted to pharmaceutical accordingly, products falling within the Harmonised System (HS) Chapter 30 and HS headings 2936, 2937, 2939 and 2941 as well as to designated pharmaceutical active HAS ADOPTED THIS REGULATION: ingredients bearing an ‘international non-proprietary name’ (INN) from the World Health Organisation, specified salts, esters or hydrates of such INNs, and designated inter- Article 1 mediates used for the production and manufacture of finished products. -
Eudract Number: 2018-000477-77 (Version: 2; Version Date: 31 Jul 2018)
Eudract Number: 2018-000477-77 (Version: 2; Version Date: 31 Jul 2018) CLINICAL NO PROFIT PROTOCOL EUDRACT NUMBER: 2018-000477-77 TITLE: Metformin versus Tolvaptan in adults with Autosomal Dominant Polycystic Kidney Disease (ADPKD): a phase 3a, independent, multi- centre, 2 parallel arms randomized controlled trial STUDY NAME: METROPOLIS VERSION: 2 VERSION DATE: 31 July 2018 Page 1 of 111 Eudract Number: 2018-000477-77 (Version: 2; Version Date: 31 Jul 2018) SPONSOR Name: Università degli Studi di Bari Dipartimento dell’Emergenza e dei Trapianti di organi (D.E.T.O.) Address: Piazza G.Cesare n.11-Policlinico- 70124 Bari Phone: +39 0805478627- Ufficio protocollo + 39080 5478614 E mail : [email protected] Signature ( per lo sponsor ) Prof. Loreto Gesualdo CHAIRMAN/STUDY Name: Prof. Loreto Gesualdo -Direttore U.O. COORDINATOR Nefrologia Universitaria – Azienda Policlinico di Bari Address: Piazza G.Cesare n.11 70124 Bari Phone: + 39 080 5594041 Fax: + 39 080 5478675 Email: [email protected] Prof. Loreto Gesualdo PRINCIPAL/COORDINATING Name: Prof. Loreto Gesualdo - Direttore U.O. INVESTIGATOR Nefrologia Universitaria – Azienda Policlinico di Bari Address: Piazza G. Cesare n.11 70124 Bari Phone: + 39 080 5594041 Fax: 39 080 5478675 Email: [email protected] Prof. Loreto Gesualdo MEDICAL WRITING Name: Prof. Loreto Gesualdo; Name: Dr. Giovanni Piscopo Page 2 of 111 Eudract Number: 2018-000477-77 (Version: 2; Version Date: 31 Jul 2018) TABLE OF CONTENTS A. LIST OF ABBREVIATIONS ....................................................................................