7-Renal Drugs FINAL
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Science of Medicine. the Art of Healing. Going Lecture Free for Genz
The science of medicine. The art of healing. Going Lecture Free for GenZ Brenda J.B. Roman, M.D. Associate Dean for Medical Education Irina Overman, M.D. Director of Foundations Curriculum Mary Jo Trout, Pharm.D. Director of Therapeutics Curriculum Image obtained from: https://visual.ly/community/infographic/other/generation-z Gen Z Learning Preferences ▪ “Hands on” learning opportunities ▪ Application to “real Life” ▪ Desire community engagement ▪ “Observers” first ▪ Value independent learning ▪ Differs from Millennials (teamwork-oriented approach) ▪ View peers and instructors as valuable resources No attendance problems What we did… Science of Learning Research… What doesn’t work Cognitive illusions ▪ Ineffective strategies that produce massive overconfidence Popular ineffective strategies ▪ Passive repetitive reading ▪ Highlighting and underlining ▪ Summarization ▪ Keyword mnemonics ▪ Imagery for text Science of Learning Research… What does work ▪ Interleaved practice ▪ Elaborative interrogation ▪ Self-explanation ▪ Distributed practice ▪ Practice testing ▪ Retrieval-based learning Foster a Growth Mindset ➢ Willingness to learn ➢ Get comfortable with from reading less than full mastery of material before the session Peer Multiple-Choice Instruction Questions Team-Based WrightQ Learning WrightCurriculum DISTRIBUTED PRACTICE INTERLEAVING READING Peer Instruction Students answer problem sets individually with ARS, then peer instruct and re-answer individually Retrieval-based learning Elaborative interrogation Self-explanation Practice -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

Conivaptan (Vaprisol )
January 3, 2007 Conivaptan (Vaprisol ®) DESCRIPTION WHAT YOU MAY NOT BE TOLD Conivaptan (Vaprisol ®) is an inhibitor of arginine Conivaptan is currently approved for euvolemic vasopressin that prevents its binding to V1a and V2 hyponatremia, but the only peer-reviewed published receptors located within the vasculature and renal data is in acute exacerbations of heart failure. It is tubules, respectively. Conivaptan was approved likely that the drug manufacturer will pursue this December 30, 2005, and is a first-in-class agent indication in the future. Conivaptan is also a potent approved for euvolemic hyponatremia. Conivaptan is inhibitor of CYP 3A4 and, as an oral formulation, available in 20 mg/5mL glass ampules. increases the area under the curve of midazolam 2- to 3-fold, simvastatin 3-fold, and amlodipine 2-fold. This WHAT THE PHARMACIST SHOULD KNOW level of interaction is what prevented the oral Euvolemic hyponatremia is most commonly associated formulation from being pursued for FDA approval. with the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Causes of this syndrome WHAT THE PATIENT SHOULD KNOW include pulmonary disease (e.g., pneumonia, Conivaptan is used to treat euvolemic hyponatremia, tuberculosis, pleural effusion) and CNS disease (e.g., manifested when a patient has too little sodium in the tumor, subarachnoid hemorrhage, meningitis). SIADH bloodstream but a normal amount of fluid in the body. also occurs with malignancies (e.g., small cell Conivaptan should not be used at this time for heart carcinoma of the lung) and can be caused by drugs failure. Conivaptan has relatively few adverse effects (e.g., chlorpropamide, carbamazepine, narcotic and is well tolerated. -

Lithium Carbonate
Right to Know Hazardous Substance Fact Sheet Common Name: LITHIUM CARBONATE Synonyms: Dilithium Carbonate; Carbolith CAS Number: 554-13-2 Chemical Name: Carbonic Acid, Dilithium Salt RTK Substance Number: 1124 Date: September 1998 Revision: January 2008 DOT Number: None Description and Use EMERGENCY RESPONDERS >>>> SEE BACK PAGE Lithium Carbonate is a white, light, odorless powder. It is Hazard Summary used in the production of glazes on ceramics and porcelain, in Hazard Rating NJDOH NFPA varnishes and dyes, as a coating on arc welding electrodes, HEALTH 1 - and in lubricating greases. It is also used as medication to FLAMMABILITY 0 - treat certain types of mental illness. REACTIVITY 0 - TERATOGEN POISONOUS GASES ARE PRODUCED IN FIRE Hazard Rating Key: 0=minimal; 1=slight; 2=moderate; 3=serious; 4=severe Reasons for Citation f Lithium Carbonate is on the Right to Know Hazardous f Lithium Carbonate can affect you when inhaled. Substance List because it is cited by DEP and EPA. f Lithium Carbonate may be a TERATOGEN. HANDLE f This chemical is on the Special Health Hazard Substance List. WITH EXTREME CAUTION. f Contact can irritate the skin and eyes. f Inhaling Lithium Carbonate can irritate the nose and throat. f Lithium Carbonate can cause nausea, vomiting, diarrhea and abdominal pain. f Inhaling Lithium Carbonate can irritate the lungs. Higher exposures may cause a build-up of fluid in the lungs SEE GLOSSARY ON PAGE 5. (pulmonary edema), a medical emergency. f Lithium Carbonate can cause headache, muscle FIRST AID weakness, confusion, seizures and coma. Eye Contact f Lithium Carbonate may cause a skin allergy. -

Lithium Carbonate
SAFETY DATA SHEET Creation Date 26-Sep-2009 Revision Date 18-Jan-2018 Revision Number 3 1. Identification Product Name Lithium Carbonate Cat No. : L119-500 CAS-No 554-13-2 Synonyms carbonic acid lithium salt; Carbonic Acid Dilithium Salt Recommended Use Laboratory chemicals. Uses advised against Not for food, drug, pesticide or biocidal product use Details of the supplier of the safety data sheet Company Fisher Scientific One Reagent Lane Fair Lawn, NJ 07410 Tel: (201) 796-7100 Emergency Telephone Number CHEMTRECÒ, Inside the USA: 800-424-9300 CHEMTRECÒ, Outside the USA: 001-703-527-3887 2. Hazard(s) identification Classification This chemical is considered hazardous by the 2012 OSHA Hazard Communication Standard (29 CFR 1910.1200) Acute oral toxicity Category 4 Skin Corrosion/irritation Category 2 Serious Eye Damage/Eye Irritation Category 1 Specific target organ toxicity (single exposure) Category 3 Target Organs - Respiratory system, Central nervous system (CNS). Label Elements Signal Word Danger Hazard Statements Harmful if swallowed Causes skin irritation Causes serious eye damage May cause respiratory irritation ______________________________________________________________________________________________ Page 1 / 7 Lithium Carbonate Revision Date 18-Jan-2018 ______________________________________________________________________________________________ Precautionary Statements Prevention Wash face, hands and any exposed skin thoroughly after handling Do not eat, drink or smoke when using this product Wear protective gloves/protective clothing/eye protection/face protection Avoid breathing dust/fume/gas/mist/vapors/spray Use only outdoors or in a well-ventilated area Inhalation IF INHALED: Remove victim to fresh air and keep at rest in a position comfortable for breathing Call a POISON CENTER or doctor/physician if you feel unwell Skin IF ON SKIN: Wash with plenty of soap and water If skin irritation occurs: Get medical advice/attention Take off contaminated clothing and wash before reuse Eyes IF IN EYES: Rinse cautiously with water for several minutes. -

Long-Term Administration of Tolvaptan to Patients with Decompensated
Int. J. Med. Sci. 2020, Vol. 17 874 Ivyspring International Publisher International Journal of Medical Sciences 2020; 17(7): 874-880. doi: 10.7150/ijms.41454 Research Paper Long-term administration of Tolvaptan to patients with decompensated cirrhosis Kengo Kanayama1, Tetsuhiro Chiba1, Kazufumi Kobayashi1, Keisuke Koroki1, Susumu Maruta1, Hiroaki Kanzaki1, Yuko Kusakabe1, Tomoko Saito1, Soichiro Kiyono1, Masato Nakamura1, Sadahisa Ogasawara1, Eiichiro Suzuki1, Yoshihiko Ooka1, Shingo Nakamoto1, Shin Yasui1, Tatsuo Kanda2, Hitoshi Maruyama3, Jun Kato1, Naoya Kato1 1. Department of Gastroenterology, Graduate School of Medicine, Chiba University, 1-8-1 Inohana, Chuo-ku, Chiba 260-8670, Japan. 2. Department of Gastroenterology and Hepatology, Nihon University School of Medicine, 30-1 Oyaguchi-Kamicho, Itabashi-ku, Tokyo 173-8610, Japan. 3. Department of Gastroenterology, Juntendo University School of Medicine, 2-1-1 Hongo, Bunkyo-ku, Tokyo 113-8421, Japan. Corresponding author: Tetsuhiro Chiba, M.D., Ph.D. Department of Gastroenterology, Graduate School of Medicine, Chiba University, 1-8-1 Inohana, Chuo-ku, Chiba 260-8670, Japan. Telephone: +81-43-2262083, Fax: +81-43-2262088, E-mail: [email protected]. © The author(s). This is an open access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/). See http://ivyspring.com/terms for full terms and conditions. Received: 2019.10.24; Accepted: 2020.02.20; Published: 2020.03.15 Abstract Aim: Tolvaptan, an oral vasopressin-2 antagonist, sometimes improves hepatic edema including ascites in patients with decompensated cirrhosis. In this study, we examined the effectiveness and survival advantage in patients with the long-term administration of tolvaptan. -
Lithium Sulfate
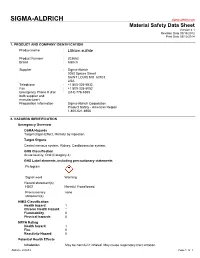
SIGMA-ALDRICH sigma-aldrich.com Material Safety Data Sheet Version 4.1 Revision Date 09/14/2012 Print Date 03/12/2014 1. PRODUCT AND COMPANY IDENTIFICATION Product name : Lithium sulfate Product Number : 203653 Brand : Aldrich Supplier : Sigma-Aldrich 3050 Spruce Street SAINT LOUIS MO 63103 USA Telephone : +1 800-325-5832 Fax : +1 800-325-5052 Emergency Phone # (For : (314) 776-6555 both supplier and manufacturer) Preparation Information : Sigma-Aldrich Corporation Product Safety - Americas Region 1-800-521-8956 2. HAZARDS IDENTIFICATION Emergency Overview OSHA Hazards Target Organ Effect, Harmful by ingestion. Target Organs Central nervous system, Kidney, Cardiovascular system. GHS Classification Acute toxicity, Oral (Category 4) GHS Label elements, including precautionary statements Pictogram Signal word Warning Hazard statement(s) H302 Harmful if swallowed. Precautionary none statement(s) HMIS Classification Health hazard: 1 Chronic Health Hazard: * Flammability: 0 Physical hazards: 0 NFPA Rating Health hazard: 1 Fire: 0 Reactivity Hazard: 0 Potential Health Effects Inhalation May be harmful if inhaled. May cause respiratory tract irritation. Aldrich - 203653 Page 1 of 7 Skin Harmful if absorbed through skin. May cause skin irritation. Eyes May cause eye irritation. Ingestion Harmful if swallowed. 3. COMPOSITION/INFORMATION ON INGREDIENTS Formula : Li2O4S Molecular Weight : 109.94 g/mol Component Concentration Lithium sulphate CAS-No. 10377-48-7 - EC-No. 233-820-4 4. FIRST AID MEASURES General advice Move out of dangerous area.Consult a physician. Show this safety data sheet to the doctor in attendance. If inhaled If breathed in, move person into fresh air. If not breathing, give artificial respiration. Consult a physician. -

Subject: Samsca (Tolvaptan) Original Effective Date: 07/27/15
Subject: Samsca (tolvaptan) Original Effective Date: 07/27/15 Policy Number: MCP-252 Revision Date(s): Review Date(s): 12/15/2016; 6/22/2017 DISCLAIMER This Medical Policy is intended to facilitate the Utilization Management process. It expresses Molina's determination as to whether certain services or supplies are medically necessary, experimental, investigational, or cosmetic for purposes of determining appropriateness of payment. The conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Molina) for a particular member. The member's benefit plan determines coverage. Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Members and their providers will need to consult the member's benefit plan to determine if there are any exclusion(s) or other benefit limitations applicable to this service or supply. If there is a discrepancy between this policy and a member's plan of benefits, the benefits plan will govern. In addition, coverage may be mandated by applicable legal requirements of a State, the Federal government or CMS for Medicare and Medicaid members. CMS's Coverage Database can be found on the CMS website. The coverage directive(s) and criteria from an existing National Coverage Determination (NCD) or Local Coverage Determination (LCD) will supersede the contents of this Molina Clinical Policy (MCP) document and provide the directive for all Medicare members. SUMMARY OF EVIDENCE/POSITION This policy addresses the coverage of Samsca (tolvaptan) for the treatment of clinically significant hypervolemic and euvolemic hyponatremia when appropriate criteria are met. -

Management and Treatment of Lithium-Induced Nephrogenic Diabetes Insipidus
REVIEW Management and treatment of lithium- induced nephrogenic diabetes insipidus Christopher K Finch†, Lithium carbonate is a well documented cause of nephrogenic diabetes insipidus, with as Tyson WA Brooks, many as 10 to 15% of patients taking lithium developing this condition. Clinicians have Peggy Yam & Kristi W Kelley been well aware of lithium toxicity for many years; however, the treatment of this drug- induced condition has generally been remedied by discontinuation of the medication or a †Author for correspondence Methodist University reduction in dose. For those patients unresponsive to traditional treatment measures, Hospital, Department several pharmacotherapeutic regimens have been documented as being effective for the of Pharmacy, University of management of lithium-induced diabetes insipidus including hydrochlorothiazide, Tennessee, College of Pharmacy, 1265 Union Ave., amiloride, indomethacin, desmopressin and correction of serum lithium levels. Memphis, TN 38104, USA Tel.: +1 901 516 2954 Fax: +1 901 516 8178 [email protected] Lithium carbonate is well known for its wide use associated with a mutation(s) of vasopressin in bipolar disorders due to its mood stabilizing receptors. Acquired causes are tubulointerstitial properties. It is also employed in aggression dis- disease (e.g., sickle cell disease, amyloidosis, orders, post-traumatic stress disorders, conduct obstructive uropathy), electrolyte disorders (e.g., disorders and even as adjunctive therapy in hypokalemia and hypercalcemia), pregnancy, or depression. Lithium has many well documented conditions induced by a drug (e.g., lithium, adverse effects as well as a relatively narrow ther- demeclocycline, amphotericin B and apeutic range of 0.4 to 0.8 mmol/l. Clinically vincristine) [3,4]. Lithium is the most common significant adverse effects include polyuria, mus- cause of drug-induced nephrogenic DI [5]. -

Diuretics in Clinical Practice. Part I: Mechanisms of Action, Pharmacological Effects and 1
Review Diuretics in clinical practice. Part I: mechanisms of action, pharmacological effects and 1. Introduction clinical indications of diuretic 2. Principles of diuretic action and classification of diuretic compounds compounds † 3. Carbonic anhydrase inhibitors Pantelis A Sarafidis , Panagiotis I Georgianos & Anastasios N Lasaridis Aristotle University of Thessaloniki, AHEPA Hospital, Section of Nephrology and Hypertension, 4. Osmotic diuretics 1st Department of Medicine, Thessaloniki, St. Kiriakidi 1, 54636, Thessaloniki, Greece 5. Loop diuretics 6. Thiazides and thiazide-related Importance of the field: Diuretics are among the most important drugs of our diuretics therapeutic armamentarium and have been broadly used for > 50 years, 7. Potassium-retaining diuretics providing important help towards the treatment of several diseases. Although all diuretics act primarily by impairing sodium reabsorption in the renal 8. Conclusion tubules, they differ in their mechanism and site of action and, therefore, in 9. Expert opinion their specific pharmacological properties and clinical indications. Loop diure- tics are mainly used for oedematous disorders (i.e., cardiac failure, nephrotic syndrome) and for blood pressure and volume control in renal disease; thiazides and related agents are among the most prescribed drugs for hypertension treatment; aldosterone-blockers are traditionally used for primary or secondary aldosteronism; and other diuretic classes have more specific indications. Areas covered in this review: This article discusses the mechanisms of action, pharmacological effects and clinical indications of the various diuretic classes For personal use only. used in everyday clinical practice, with emphasis on recent knowledge sug- gesting beneficial effects of certain diuretics on clinical conditions distinct from the traditional indications of these drugs (i.e., heart protection for aldosterone blockers). -

Mineralocorticoid Receptor Antagonists for Heart Failure with Reduced Ejection Fraction: Integrating Evidence Into Clinical Practice
European Heart Journal Advance Access published August 31, 2012 European Heart Journal REVIEW doi:10.1093/eurheartj/ehs257 Novel Therapeutic Concepts Mineralocorticoid receptor antagonists for heart failure with reduced ejection fraction: integrating evidence into clinical practice Faiez Zannad1*, Wendy Gattis Stough2,PatrickRossignol1, Johann Bauersachs3, John J.V. McMurray4,KarlSwedberg5,AllanD.Struthers6, Adriaan A. Voors7, Luis M. Ruilope8,GeorgeL.Bakris9, Christopher M. O’Connor10, Mihai Gheorghiade11, Downloaded from Robert J. Mentz10, Alain Cohen-Solal12,AldoP.Maggioni13, Farzin Beygui14, Gerasimos S. Filippatos15,ZiadA.Massy16, Atul Pathak17, Ileana L. Pin˜a18, Hani N. Sabbah19, Domenic A. Sica20, Luigi Tavazzi21, and Bertram Pitt22 http://eurheartj.oxfordjournals.org/ 1INSERM, Centre d’Investigation Clinique 9501 and Unite´ 961, Centre Hospitalier Universitaire, and the Department of Cardiology, Nancy University, Universite´ de Lorraine, Nancy, France; 2Campbell University College of Pharmacy and Health Sciences, Buies Creek, NC, USA; 3Department of Cardiology and Angiology, Hannover Medical School, Hannover, Germany; 4Western Infirmary and the British Heart Foundation, Glasgow Cardiovascular Research Centre, University of Glasgow, Glasgow, UK; 5Department of Molecular and Clinical Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; 6University of Dundee, Ninewells Hospital and Medical School, Dundee, UK; 7University Medical Center Groningen, University of Groningen, Groningen, The Netherlands; 8Hypertension -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01