LITHIUM PRESCRIBING GUIDELINES Lithium for The
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Report of the Advisory Group to Recommend Priorities for the IARC Monographs During 2020–2024
IARC Monographs on the Identification of Carcinogenic Hazards to Humans Report of the Advisory Group to Recommend Priorities for the IARC Monographs during 2020–2024 Report of the Advisory Group to Recommend Priorities for the IARC Monographs during 2020–2024 CONTENTS Introduction ................................................................................................................................... 1 Acetaldehyde (CAS No. 75-07-0) ................................................................................................. 3 Acrolein (CAS No. 107-02-8) ....................................................................................................... 4 Acrylamide (CAS No. 79-06-1) .................................................................................................... 5 Acrylonitrile (CAS No. 107-13-1) ................................................................................................ 6 Aflatoxins (CAS No. 1402-68-2) .................................................................................................. 8 Air pollutants and underlying mechanisms for breast cancer ....................................................... 9 Airborne gram-negative bacterial endotoxins ............................................................................. 10 Alachlor (chloroacetanilide herbicide) (CAS No. 15972-60-8) .................................................. 10 Aluminium (CAS No. 7429-90-5) .............................................................................................. 11 -

Lithium Carbonate
Right to Know Hazardous Substance Fact Sheet Common Name: LITHIUM CARBONATE Synonyms: Dilithium Carbonate; Carbolith CAS Number: 554-13-2 Chemical Name: Carbonic Acid, Dilithium Salt RTK Substance Number: 1124 Date: September 1998 Revision: January 2008 DOT Number: None Description and Use EMERGENCY RESPONDERS >>>> SEE BACK PAGE Lithium Carbonate is a white, light, odorless powder. It is Hazard Summary used in the production of glazes on ceramics and porcelain, in Hazard Rating NJDOH NFPA varnishes and dyes, as a coating on arc welding electrodes, HEALTH 1 - and in lubricating greases. It is also used as medication to FLAMMABILITY 0 - treat certain types of mental illness. REACTIVITY 0 - TERATOGEN POISONOUS GASES ARE PRODUCED IN FIRE Hazard Rating Key: 0=minimal; 1=slight; 2=moderate; 3=serious; 4=severe Reasons for Citation f Lithium Carbonate is on the Right to Know Hazardous f Lithium Carbonate can affect you when inhaled. Substance List because it is cited by DEP and EPA. f Lithium Carbonate may be a TERATOGEN. HANDLE f This chemical is on the Special Health Hazard Substance List. WITH EXTREME CAUTION. f Contact can irritate the skin and eyes. f Inhaling Lithium Carbonate can irritate the nose and throat. f Lithium Carbonate can cause nausea, vomiting, diarrhea and abdominal pain. f Inhaling Lithium Carbonate can irritate the lungs. Higher exposures may cause a build-up of fluid in the lungs SEE GLOSSARY ON PAGE 5. (pulmonary edema), a medical emergency. f Lithium Carbonate can cause headache, muscle FIRST AID weakness, confusion, seizures and coma. Eye Contact f Lithium Carbonate may cause a skin allergy. -

Lithium Carbonate
SAFETY DATA SHEET Creation Date 26-Sep-2009 Revision Date 18-Jan-2018 Revision Number 3 1. Identification Product Name Lithium Carbonate Cat No. : L119-500 CAS-No 554-13-2 Synonyms carbonic acid lithium salt; Carbonic Acid Dilithium Salt Recommended Use Laboratory chemicals. Uses advised against Not for food, drug, pesticide or biocidal product use Details of the supplier of the safety data sheet Company Fisher Scientific One Reagent Lane Fair Lawn, NJ 07410 Tel: (201) 796-7100 Emergency Telephone Number CHEMTRECÒ, Inside the USA: 800-424-9300 CHEMTRECÒ, Outside the USA: 001-703-527-3887 2. Hazard(s) identification Classification This chemical is considered hazardous by the 2012 OSHA Hazard Communication Standard (29 CFR 1910.1200) Acute oral toxicity Category 4 Skin Corrosion/irritation Category 2 Serious Eye Damage/Eye Irritation Category 1 Specific target organ toxicity (single exposure) Category 3 Target Organs - Respiratory system, Central nervous system (CNS). Label Elements Signal Word Danger Hazard Statements Harmful if swallowed Causes skin irritation Causes serious eye damage May cause respiratory irritation ______________________________________________________________________________________________ Page 1 / 7 Lithium Carbonate Revision Date 18-Jan-2018 ______________________________________________________________________________________________ Precautionary Statements Prevention Wash face, hands and any exposed skin thoroughly after handling Do not eat, drink or smoke when using this product Wear protective gloves/protective clothing/eye protection/face protection Avoid breathing dust/fume/gas/mist/vapors/spray Use only outdoors or in a well-ventilated area Inhalation IF INHALED: Remove victim to fresh air and keep at rest in a position comfortable for breathing Call a POISON CENTER or doctor/physician if you feel unwell Skin IF ON SKIN: Wash with plenty of soap and water If skin irritation occurs: Get medical advice/attention Take off contaminated clothing and wash before reuse Eyes IF IN EYES: Rinse cautiously with water for several minutes. -

BNSSG Shared Care Guidance Please Complete All Sections
NHS Bristol North Bristol NHS Trust NHS North Somerset University Hospitals Bristol NHS Foundation Trust NHS South Gloucestershire Weston Area Health NHS Trust BNSSG Shared Care Guidance Please complete all sections AMBER 3 month Section 1: Heading Avon & Wiltshire Mental Health Partnership NHS Trust Trust(s) Speciality / Department Mental Health Agreement for Lithium Drug (please prescribe by brand name and specify formulation: Priadel, Camcolit®, Liskonum®, Li-Liquid® ) 1. The management of acute manic or hypomanic episodes. 2. The management of episodes of recurrent depressive disorders where treatment with other antidepressants has Indication been unsuccessful. 3. The prophylaxis against bipolar affective disorders. 4. Control of aggressive behaviour or intentional self harm. Section 2: Treatment Schedule Dosage is adjusted based on serum-lithium concentration. Lithium levels must be taken 12 hours post dose, otherwise clinical value is lost. Lithium has a narrow therapeutic range necessitating blood levels between 0.4-1.2mmol/L. The lower end of this range is used for elderly and infirmed patients and the upper end for younger patients, particularly those being treated for an episode of mania. Clinicians should aim for levels of 0.6-0.8 mmol/L, with higher levels possibly being of benefit for patients with predominantly manic symptoms. Usual dose and frequency of Rarely 1.2mmol/L may be used. administration The starting dose is usually 400mg at night (200mg in the elderly), adjusted to achieve the desired serum-lithium concentration. Bloods should be taken 12 hours post dose. For tablet preparations dose is usually given as a single dose at night; for liquid preparations, the dose may be spilt to twice a day. -

(12) United States Patent (10) Patent No.: US 9,642,912 B2 Kisak Et Al
USOO9642912B2 (12) United States Patent (10) Patent No.: US 9,642,912 B2 Kisak et al. (45) Date of Patent: *May 9, 2017 (54) TOPICAL FORMULATIONS FOR TREATING (58) Field of Classification Search SKIN CONDITIONS CPC ...................................................... A61K 31f S7 (71) Applicant: Crescita Therapeutics Inc., USPC .......................................................... 514/171 Mississauga (CA) See application file for complete search history. (72) Inventors: Edward T. Kisak, San Diego, CA (56) References Cited (US); John M. Newsam, La Jolla, CA (US); Dominic King-Smith, San Diego, U.S. PATENT DOCUMENTS CA (US); Pankaj Karande, Troy, NY (US); Samir Mitragotri, Santa Barbara, 5,602,183 A 2f1997 Martin et al. CA (US); Wade A. Hull, Kaysville, UT 5,648,380 A 7, 1997 Martin 5,874.479 A 2, 1999 Martin (US); Ngoc Truc-ChiVo, Longueuil 6,328,979 B1 12/2001 Yamashita et al. (CA) 7,001,592 B1 2/2006 Traynor et al. 7,795,309 B2 9/2010 Kisak et al. (73) Assignee: Crescita Therapeutics Inc., 8,343,962 B2 1/2013 Kisak et al. Mississauga (CA) 8,513,304 B2 8, 2013 Kisak et al. 8,535,692 B2 9/2013 Pongpeerapat et al. (*) Notice: Subject to any disclaimer, the term of this 9,308,181 B2* 4/2016 Kisak ..................... A61K 47/12 patent is extended or adjusted under 35 2002fOOO6435 A1 1/2002 Samuels et al. 2002fOO64524 A1 5, 2002 Cevc U.S.C. 154(b) by 204 days. 2005, OO 14823 A1 1/2005 Soderlund et al. This patent is Subject to a terminal dis 2005.00754O7 A1 4/2005 Tamarkin et al. -
Lithium Sulfate
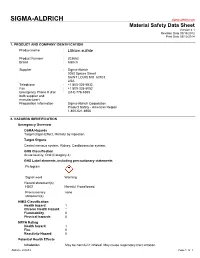
SIGMA-ALDRICH sigma-aldrich.com Material Safety Data Sheet Version 4.1 Revision Date 09/14/2012 Print Date 03/12/2014 1. PRODUCT AND COMPANY IDENTIFICATION Product name : Lithium sulfate Product Number : 203653 Brand : Aldrich Supplier : Sigma-Aldrich 3050 Spruce Street SAINT LOUIS MO 63103 USA Telephone : +1 800-325-5832 Fax : +1 800-325-5052 Emergency Phone # (For : (314) 776-6555 both supplier and manufacturer) Preparation Information : Sigma-Aldrich Corporation Product Safety - Americas Region 1-800-521-8956 2. HAZARDS IDENTIFICATION Emergency Overview OSHA Hazards Target Organ Effect, Harmful by ingestion. Target Organs Central nervous system, Kidney, Cardiovascular system. GHS Classification Acute toxicity, Oral (Category 4) GHS Label elements, including precautionary statements Pictogram Signal word Warning Hazard statement(s) H302 Harmful if swallowed. Precautionary none statement(s) HMIS Classification Health hazard: 1 Chronic Health Hazard: * Flammability: 0 Physical hazards: 0 NFPA Rating Health hazard: 1 Fire: 0 Reactivity Hazard: 0 Potential Health Effects Inhalation May be harmful if inhaled. May cause respiratory tract irritation. Aldrich - 203653 Page 1 of 7 Skin Harmful if absorbed through skin. May cause skin irritation. Eyes May cause eye irritation. Ingestion Harmful if swallowed. 3. COMPOSITION/INFORMATION ON INGREDIENTS Formula : Li2O4S Molecular Weight : 109.94 g/mol Component Concentration Lithium sulphate CAS-No. 10377-48-7 - EC-No. 233-820-4 4. FIRST AID MEASURES General advice Move out of dangerous area.Consult a physician. Show this safety data sheet to the doctor in attendance. If inhaled If breathed in, move person into fresh air. If not breathing, give artificial respiration. Consult a physician. -

Therapeutic Drug Monitoring Clinical Guide FOURTH EDITION
DIAGNOSTICS Therapeutic Drug Monitoring Clinical Guide FOURTH EDITION 1 Therapeutic Drug Monitoring Clinical Guide FOURTH EDITION Authors Mike Hallworth, MA, MSc, FRCPath Former Consultant Biochemist Royal Shrewsbury Hospital United Kingdom Ian Watson, MSc, PhD, FRCPath Former Consultant Biochemist and Toxicologist University Hospital Aintree Liverpool, United Kingdom Editors of the David Holt, DSc, PhD Third Edition Susan Tett, PhD, BPharm (Hons), MPS Steven H. Wong, PhD, DABCC (TC), FACB 2 CONTENTS THERAPEUTIC DRUG MONITORING . 5 RUFINAMIDE . 81 WHY IS TDM NECESSARY? . 6 TIAGABINE . 83 WHICH DRUGS SHOULD BE MONITORED? . 8 TOPIRAMATE . 85 PRACTICAL CONSIDERATIONS . 10 VALPROATE . 87 CALCULATION OF DOSAGE ADJUSTMENT . 15 VIGABATRIN . 89 OTHER APPROACHES TO OPTIMIZING THERAPY — ZONISAMIDE . 91 PHARMACOGENETICS AND BIOMARKERS . 17 ANTIFUNGALS . 94 EFFECTIVENESS OF TDM – DOES IT HELP PATIENTS? . 19 POSOCONAZOLE/VORICONAZOLE . 95 REFERENCES . 21 ANTINEOPLASTICS . 98 WEBSITES . 23 BUSULFAN . 99 DRUG DATA PROFILES . 24 METHOTREXATE . 101 PREFACE . 24 ANTIRETROVIRALS . 104 ADDICTION THERAPEUTICS . 28 ANTIRETROVIRALS . 105 BUPRENORPHINE . 29 BRONCHODILATOR, ANALEPTIC . 108 METHADONE . 31 THEOPHYLLINE . 109 ANALGESICS . 34 CAFFEINE . 111 ACETAMINOPHEN (PARACETAMOL) . 35 CARDIAC AGENTS . 114 ACETYLSALICYLIC ACID (ASPIRIN) . 37 ANTI-ARRHYTHMICS MORPHINE . 39 AMIODARONE . 115 ANTIBIOTICS . 42 DISOPYRAMIDE . 117 AMINOGLYCOSIDES FLECAINIDE . 119 AMIKACIN . 43 LIDOCAINE . 121 GENTAMICIN . 45 CARDIAC GLYCOSIDES TOBRAMYCIN . 47 DIGOXIN . 123 OTHER ANTIBIOTICS -

Management and Treatment of Lithium-Induced Nephrogenic Diabetes Insipidus
REVIEW Management and treatment of lithium- induced nephrogenic diabetes insipidus Christopher K Finch†, Lithium carbonate is a well documented cause of nephrogenic diabetes insipidus, with as Tyson WA Brooks, many as 10 to 15% of patients taking lithium developing this condition. Clinicians have Peggy Yam & Kristi W Kelley been well aware of lithium toxicity for many years; however, the treatment of this drug- induced condition has generally been remedied by discontinuation of the medication or a †Author for correspondence Methodist University reduction in dose. For those patients unresponsive to traditional treatment measures, Hospital, Department several pharmacotherapeutic regimens have been documented as being effective for the of Pharmacy, University of management of lithium-induced diabetes insipidus including hydrochlorothiazide, Tennessee, College of Pharmacy, 1265 Union Ave., amiloride, indomethacin, desmopressin and correction of serum lithium levels. Memphis, TN 38104, USA Tel.: +1 901 516 2954 Fax: +1 901 516 8178 [email protected] Lithium carbonate is well known for its wide use associated with a mutation(s) of vasopressin in bipolar disorders due to its mood stabilizing receptors. Acquired causes are tubulointerstitial properties. It is also employed in aggression dis- disease (e.g., sickle cell disease, amyloidosis, orders, post-traumatic stress disorders, conduct obstructive uropathy), electrolyte disorders (e.g., disorders and even as adjunctive therapy in hypokalemia and hypercalcemia), pregnancy, or depression. Lithium has many well documented conditions induced by a drug (e.g., lithium, adverse effects as well as a relatively narrow ther- demeclocycline, amphotericin B and apeutic range of 0.4 to 0.8 mmol/l. Clinically vincristine) [3,4]. Lithium is the most common significant adverse effects include polyuria, mus- cause of drug-induced nephrogenic DI [5]. -

Safety Data Sheet
SAFETY DATA SHEET Creation Date 22-Sep-2009 Revision Date 27-Dec-2020 Revision Number 2 SECTION 1: IDENTIFICATION OF THE SUBSTANCE/MIXTURE AND OF THE COMPANY/UNDERTAKING 1.1. Product identifier Product Description: Lithium citrate tribasic tetrahydrate Cat No. : 47373 Synonyms Lithium citrate tetrahydrate Molecular Formula C6 H5 Li3 O7 . 4 H2 O 1.2. Relevant identified uses of the substance or mixture and uses advised against Recommended Use Laboratory chemicals. Uses advised against No Information available 1.3. Details of the supplier of the safety data sheet Company Thermo Fisher (Kandel) GmbH . Erlenbachweg 2 76870 Kandel Germany Tel: +49 (0) 721 84007 280 Fax: +49 (0) 721 84007 300 E-mail address [email protected] www.alfa.com Product safety Tel + +049 (0) 7275 988687-0 1.4. Emergency telephone number Carechem 24: +44 (0) 1235 239 670 (Multi-language emergency number) Poison Information Center Mainz www.giftinfo.uni-mainz.de Telephone: +49(0)6131/19240 Exclusively for customers in Austria: Poison Information Center (VIZ) Emergency call 0-24 clock: +43 1 406 43 43 Office hours: Monday to Friday, 8am to 4pm, tel: +43 1 406 68 98 SECTION 2: HAZARDS IDENTIFICATION 2.1. Classification of the substance or mixture CLP Classification - Regulation (EC) No 1272/2008 Physical hazards Based on available data, the classification criteria are not met ______________________________________________________________________________________________ ALFAA47373 Page 1 / 10 SAFETY DATA SHEET Lithium citrate tribasic tetrahydrate Revision Date 27-Dec-2020 ______________________________________________________________________________________________ Health hazards Based on available data, the classification criteria are not met Environmental hazards Based on available data, the classification criteria are not met Full text of Hazard Statements: see section 16 2.2. -

Subchronic Lithium Treatment Increases the Anxiolytic-Like Effect of Mirtazapine on the Expression of Contextual Title Conditioned Fear
Subchronic lithium treatment increases the anxiolytic-like effect of mirtazapine on the expression of contextual Title conditioned fear Author(s) An, Yan; Inoue, Takeshi; Kitaichi, Yuji; Nakagawa, Shin; Wang, Ce; Chen, Chong; Song, Ning; Kusumi, Ichiro European journal of pharmacology, 747, 13-17 Citation https://doi.org/10.1016/j.ejphar.2014.11.009 Issue Date 2015-01-15 Doc URL http://hdl.handle.net/2115/58243 Type article (author version) File Information AnManuscript.pdf Instructions for use Hokkaido University Collection of Scholarly and Academic Papers : HUSCAP Subchronic lithium treatment increases the anxiolytic-like effect of mirtazapine on the expression of contextual conditioned fear Yan Ana, Takeshi Inouea*, Yuji Kitaichia, Shin Nakagawaa, Ce Wangb, Chong Chena, Ning Songa, Ichiro Kusumia a Department of Psychiatry, Hokkaido University Graduate School of Medicine, North 15, West 7, Kita-ku, Sapporo 060-8638, Japan b Department of Neuropharmacology, Hokkaido University Graduate School of Medicine, North 15, West 7, Kita-ku, Sapporo 060-8638, Japan Number of figures: 3 Corresponding address: Takeshi Inoue, Department of Psychiatry, Hokkaido University Graduate School of Medicine, North 15, West 7, Kita-ku, Sapporo 060-8638, Japan Phone: +81(11)706-5160 Fax: +81(11)706-5081 E-mail: [email protected] 1 Abstract Lithium not only has a mood-stabilizing effect but also the augmentation effect of an antidepressant, the mechanism of which remains unclear. Although lithium may augment the effect of mirtazapine, this augmentation has not been confirmed. Using a contextual fear conditioning test in rats, an animal model of anxiety or fear, we examined the effect of subchronic lithium carbonate (in diet) in combination with systemic mirtazapine on the expression of contextual conditioned fear. -
Lithium Sulfate, Technical Grade, Min. 99.0 %
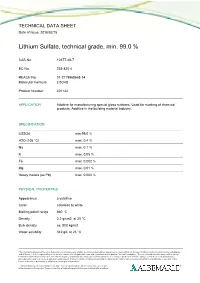
TECHNICAL DATA SHEET Date of Issue: 2018/02/15 Lithium Sulfate, technical grade, min. 99.0 % CAS-No. 10377-48-7 EC-No. 233-820-4 REACH No. 01-2119968668-14 Molecular Formula Li2O4S Product Number 401142 APPLICATION Additive for manufacturing special glass mixtures. Used for marking of chemical products. Additive in the building material industry. SPECIFICATION Li2SO4 min 99.0 % H2O (105 °C) max. 0.4 % Na max. 0.1 % K max. 0.05 % Fe max. 0.002 % Mg max. 0.01 % Heavy metals (as Pb) max. 0.004 % PHYSICAL PROPERTIES Appearance crystalline Color colorless to white Melting point/ range 860 °C Density 2.2 g/cm3 at 20 °C Bulk density ca. 800 kg/m3 Water solubility 342 g/L at 25 °C The information presented herein is believed to be accurate and reliable, but is presented without guarantee or responsibility on the part of Albemarle Corporation and its subsidiaries and affiliates. It is the responsibility of the user to comply with all applicable laws and regulations and to provide for a safe workplace. The user should consider any health or safety hazards or information contained herein only as a guide, and should take those precautions which are necessary or prudent to instruct employees and to develop work practice procedures in order to promote a safe work environment. Further, nothing contained herein shall be taken as an inducement or recommendation to manufacture or use any of the herein materials or processes in violation of existing or future patent. Technical data sheets may change frequently. You can download the latest version from our website www.albemarle-lithium.com. -

A History of the Pharmacological Treatment of Bipolar Disorder
International Journal of Molecular Sciences Review A History of the Pharmacological Treatment of Bipolar Disorder Francisco López-Muñoz 1,2,3,4,* ID , Winston W. Shen 5, Pilar D’Ocon 6, Alejandro Romero 7 ID and Cecilio Álamo 8 1 Faculty of Health Sciences, University Camilo José Cela, C/Castillo de Alarcón 49, 28692 Villanueva de la Cañada, Madrid, Spain 2 Neuropsychopharmacology Unit, Hospital 12 de Octubre Research Institute (i+12), Avda. Córdoba, s/n, 28041 Madrid, Spain 3 Portucalense Institute of Neuropsychology and Cognitive and Behavioural Neurosciences (INPP), Portucalense University, R. Dr. António Bernardino de Almeida 541, 4200-072 Porto, Portugal 4 Thematic Network for Cooperative Health Research (RETICS), Addictive Disorders Network, Health Institute Carlos III, MICINN and FEDER, 28029 Madrid, Spain 5 Departments of Psychiatry, Wan Fang Medical Center and School of Medicine, Taipei Medical University, 111 Hsin Long Road Section 3, Taipei 116, Taiwan; [email protected] 6 Department of Pharmacology, Faculty of Pharmacy, University of Valencia, Avda. Vicente Andrés, s/n, 46100 Burjassot, Valencia, Spain; [email protected] 7 Department of Pharmacology and Toxicology, Faculty of Veterinary Medicine, Complutense University, Avda. Puerta de Hierro, s/n, 28040 Madrid, Spain; [email protected] 8 Department of Biomedical Sciences (Pharmacology Area), Faculty of Medicine and Health Sciences, University of Alcalá, Crta. de Madrid-Barcelona, Km. 33,600, 28871 Alcalá de Henares, Madrid, Spain; [email protected] * Correspondence: fl[email protected] or [email protected] Received: 4 June 2018; Accepted: 13 July 2018; Published: 23 July 2018 Abstract: In this paper, the authors review the history of the pharmacological treatment of bipolar disorder, from the first nonspecific sedative agents introduced in the 19th and early 20th century, such as solanaceae alkaloids, bromides and barbiturates, to John Cade’s experiments with lithium and the beginning of the so-called “Psychopharmacological Revolution” in the 1950s.