Upfront Dexrazoxane for the Reduction of Anthracycline-Induced
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thames Valley Chemotherapy Regimens Sarcoma
Thames Valley Thames Valley Chemotherapy Regimens Sarcoma Chemotherapy Regimens– Sarcoma 1 of 98 Thames Valley Notes from the editor All chemotherapy regimens, and associated guidelines eg antiemetics and dose bands are available on the Network website www.tvscn.nhs.uk/networks/cancer-topics/chemotherapy/ Any correspondence about the regimens should be addressed to: Sally Coutts, Cancer Pharmacist, Thames Valley email: [email protected] Acknowledgements These regimens have been compiled by the Network Pharmacy Group in collaboration with key contribution from Prof Bass Hassan, Medical Oncologist, OUH Dr Sally Trent, Clinical Oncologist, OUH Dr James Gildersleve, Clinical Oncologist, RBFT Dr Sarah Pratap, Medical Oncologist, OUH Dr Shaun Wilson, TYA - Paediatric Oncologist, OUH Catherine Chaytor, Cancer Pharmacist, OUH Varsha Ormerod, Cancer Pharmacist, OUH Kristen Moorhouse, Cancer Pharmacist, OUH © Thames Valley Cancer Network. All rights reserved. Not to be reproduced in whole or in part without the permission of the copyright owner. Chemotherapy Regimens– Sarcoma 2 of 98 Thames Valley Thames Valley Chemotherapy Regimens Sarcoma Network Chemotherapy Regimens used in the management of Sarcoma Date published: January 2019 Date of review: June 2022 Chemotherapy Regimens Name of regimen Indication Page List of amendments to this version 5 Imatinib GIST 6 Sunitinib GIST 9 Regorafenib GIST 11 Paclitaxel weekly (Taxol) Angiosarcoma 13 AC Osteosarcoma 15 Cisplatin Imatinib – if local Trust funding agreed Chordoma 18 Doxorubicin Sarcoma 21 -

Deferasirox (Exjade, Jadenu) Reference Number: CP.PHAR.145 Effective Date: 11.15 Last Review Date: 11.17 Line of Business: Medicaid Revision Log
Clinical Policy: Deferasirox (Exjade, Jadenu) Reference Number: CP.PHAR.145 Effective Date: 11.15 Last Review Date: 11.17 Line of Business: Medicaid Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Deferasirox (Exjade®, Jadenu®) is an iron chelator. FDA Approved Indication(s) Exjade and Jadenu are indicated: For the treatment of chronic iron overload due to blood transfusions (transfusional hemosiderosis) in patients 2 years of age and older. For the treatment of chronic iron overload in patients 10 years of age and older with non- transfusion-dependent thalassemia syndromes and with a liver iron concentration (LIC) of at least 5 milligrams of iron per gram of liver dry weight (mg Fe/g dw) and a serum ferritin greater than 300 mcg/L. Limitation of use: Controlled clinical trials of Exjade/Jadenu with myelodysplastic syndromes and chronic iron overload due to blood transfusions have not been performed. The safety and efficacy of Exjade/Jadenu when administered with other iron chelation therapy have not been established. Policy/Criteria Provider must submit documentation (including office chart notes and lab results) supporting that member has met all approval criteria It is the policy of health plans affiliated with Centene Corporation® that Exjade and Jadenu are medically necessary when the following criteria are met: I. Initial Approval Criteria A. Chronic Iron Overload Due to Blood Transfusions (must meet all): 1. Diagnosis of chronic iron overload due to blood transfusions as may occur in the treatment of chronic anemia, including thalassemia; 2. Age ≥ 2 years old; 3. -

Chelation Therapy
Corporate Medical Policy Chelation Therapy File Name: chelation_therapy Origination: 12/1995 Last CAP Review: 2/2021 Next CAP Review: 2/2022 Last Review: 2/2021 Description of Procedure or Service Chelation therapy is an established treatment for the removal of metal toxins by converting them to a chemically inert form that can be excreted in the urine. Chelation therapy comprises intravenous or oral administration of chelating agents that remove metal ions such as lead, aluminum, mercury, arsenic, zinc, iron, copper, and calcium from the body. Specific chelating agents are used for particular heavy metal toxicities. For example, desferroxamine (not Food and Drug Administration [FDA] approved) is used for patients with iron toxicity, and calcium-ethylenediaminetetraacetic acid (EDTA) is used for patients with lead poisoning. Note that disodium-EDTA is not recommended for acute lead poisoning due to the increased risk of death from hypocalcemia. Another class of chelating agents, called metal protein attenuating compounds (MPACs), is under investigation for the treatment of Alzheimer’s disease, which is associated with the disequilibrium of cerebral metals. Unlike traditional systemic chelators that bind and remove metals from tissues systemically, MPACs have subtle effects on metal homeostasis and abnormal metal interactions. In animal models of Alzheimer’s disease, they promote the solubilization and clearance of β-amyloid protein by binding to its metal-ion complex and also inhibit redox reactions that generate neurotoxic free radicals. MPACs therefore interrupt two putative pathogenic processes of Alzheimer’s disease. However, no MPACs have received FDA approval for treating Alzheimer’s disease. Chelation therapy has also been investigated as a treatment for other indications including atherosclerosis and autism spectrum disorder. -

Cardiotoxicity of Doxorubicin Is Mediated Through Mitochondrial Iron Accumulation
Cardiotoxicity of doxorubicin is mediated through mitochondrial iron accumulation Yoshihiko Ichikawa, … , Tejaswitha Jairaj Naik, Hossein Ardehali J Clin Invest. 2014;124(2):617-630. https://doi.org/10.1172/JCI72931. Research Article Cardiology Doxorubicin is an effective anticancer drug with known cardiotoxic side effects. It has been hypothesized that doxorubicin- dependent cardiotoxicity occurs through ROS production and possibly cellular iron accumulation. Here, we found that cardiotoxicity develops through the preferential accumulation of iron inside the mitochondria following doxorubicin treatment. In isolated cardiomyocytes, doxorubicin became concentrated in the mitochondria and increased both mitochondrial iron and cellular ROS levels. Overexpression of ABCB8, a mitochondrial protein that facilitates iron export, in vitro and in the hearts of transgenic mice decreased mitochondrial iron and cellular ROS and protected against doxorubicin-induced cardiomyopathy. Dexrazoxane, a drug that attenuates doxorubicin-induced cardiotoxicity, decreased mitochondrial iron levels and reversed doxorubicin-induced cardiac damage. Finally, hearts from patients with doxorubicin-induced cardiomyopathy had markedly higher mitochondrial iron levels than hearts from patients with other types of cardiomyopathies or normal cardiac function. These results suggest that the cardiotoxic effects of doxorubicin develop from mitochondrial iron accumulation and that reducing mitochondrial iron levels protects against doxorubicin- induced cardiomyopathy. Find the latest version: https://jci.me/72931/pdf Research article Cardiotoxicity of doxorubicin is mediated through mitochondrial iron accumulation Yoshihiko Ichikawa,1 Mohsen Ghanefar,1 Marina Bayeva,1 Rongxue Wu,1 Arineh Khechaduri,1 Sathyamangla V. Naga Prasad,2 R. Kannan Mutharasan,1 Tejaswitha Jairaj Naik,1 and Hossein Ardehali1 1Feinberg Cardiovascular Institute, Northwestern University School of Medicine, Chicago, Illinois, USA. -

Targeted EDTA Chelation Therapy with Albumin Nanoparticles To
Clemson University TigerPrints All Dissertations Dissertations 8-2019 Targeted EDTA Chelation Therapy with Albumin Nanoparticles to Reverse Arterial Calcification and Restore Vascular Health in Chronic Kidney Disease Saketh Ram Karamched Clemson University, [email protected] Follow this and additional works at: https://tigerprints.clemson.edu/all_dissertations Recommended Citation Karamched, Saketh Ram, "Targeted EDTA Chelation Therapy with Albumin Nanoparticles to Reverse Arterial Calcification and Restore Vascular Health in Chronic Kidney Disease" (2019). All Dissertations. 2479. https://tigerprints.clemson.edu/all_dissertations/2479 This Dissertation is brought to you for free and open access by the Dissertations at TigerPrints. It has been accepted for inclusion in All Dissertations by an authorized administrator of TigerPrints. For more information, please contact [email protected]. TARGETED EDTA CHELATION THERAPY WITH ALBUMIN NANOPARTICLES TO REVERSE ARTERIAL CALCIFICATION AND RESTORE VASCULAR HEALTH IN CHRONIC KIDNEY DISEASE A Dissertation Presented to the Graduate School of Clemson University In Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy Bioengineering by Saketh Ram Karamched August 2019 Accepted by: Dr. Narendra Vyavahare, Ph.D., Committee Chair Dr. Agneta Simionescu, Ph.D. Dr. Alexey Vertegel, Ph.D. Dr. Christopher G. Carsten, III, M.D. ABSTRACT Cardiovascular diseases (CVDs) are the leading cause of death globally. An estimated 17.9 million people died from CVDs in 2016, with ~840,000 of them in the United States alone. Traditional risk factors, such as smoking, hypertension, and diabetes, are well discussed. In recent years, chronic kidney disease (CKD) has emerged as a risk factor of equal importance. Patients with mild-to-moderate CKD are much more likely to develop and die from CVDs than progress to end-stage renal failure. -

ZINECARD® (Dexrazoxane) for Injection Regimens
HIGHLIGHTS OF PRESCRIBING INFORMATION ----------------------DOSAGE FORMS AND STRENGTHS------------- These highlights do not include all the information needed to use 250 mg or 500 mg single dose vials as sterile, pyrogen-free lyophilizates. (3) ZINECARD safely and effectively. See full prescribing information for ZINECARD. -------------------------------CONTRAINDICATIONS------------------------------ ZINECARD should not be used with non-anthracycline chemotherapy ZINECARD® (dexrazoxane) for injection regimens. (4) Initial U.S. Approval: 1995 -----------------------WARNINGS AND PRECAUTIONS------------------------ ---------------------------INDICATIONS AND USAGE----------------------- Myelosuppression: ZINECARD may increase the myelosuppresive ZINECARD is a cytoprotective agent indicated for reducing the incidence and effects of chemotherapeutic agents. Perform hematological monitoring. severity of cardiomyopathy associated with doxorubicin administration in (5.1) women with metastatic breast cancer who have received a cumulative Embryo-Fetal Toxicity: Can cause fetal harm. Advise female patients of doxorubicin dose of 300 mg/m2 and who will continue to receive doxorubicin reproductive potential of the potential hazard to the fetus. (5.5, 8.1) therapy to maintain tumor control. Do not use ZINECARD with doxorubicin initiation. (1) ------------------------------ADVERSE REACTIONS------------------------------- In clinical studies, ZINECARD was administered to patients also receiving -----------------------DOSAGE AND ADMINISTRATION---------------------- chemotherapeutic agents for cancer. Pain on injection was observed more Reconstitute vial contents and dilute before use. (2.3) frequently in patients receiving ZINECARD versus placebo. (6.1) Administer ZINECARD by intravenous infusion over 15 minutes. DO NOT ADMINISTER VIA AN INTRAVENOUS PUSH. (2.1, 2.3) To report SUSPECTED ADVERSE REACTIONS, contact Pfizer, Inc. at The recommended dosage ratio of ZINECARD to doxorubicin is 10:1 1-800-438-1985 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. -
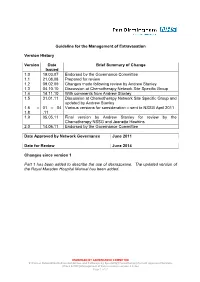
Guideline for the Management of Extravasation
Guideline for the Management of Extravasation Version History Version Date Brief Summary of Change Issued 1.0 19.03.07 Endorsed by the Governance Committee 1.1 21.08.08 Prepared for review 1.2 09.02.09 Changes made following review by Andrew Stanley 1.3 04.10.10 Discussion at Chemotherapy Network Site Specific Group 1.4 14.11.10 With comments from Andrew Stanley 1.5 31.01.11 Discussion at Chemotherapy Network Site Specific Group and updated by Andrew Stanley 1.6 – 01 – 04 Various versions for consideration – sent to NSSG April 2011 1.8 .11 1.9 05.05.11 Final version by Andrew Stanley for review by the Chemotherapy NSSG and Jeanette Hawkins 2.0 14.06.11 Endorsed by the Governance Committee Date Approved by Network Governance June 2011 Date for Review June 2014 Changes since version 1 Part 1 has been added to describe the use of dexrazoxane. The updated version of the Royal Marsden Hospital Manual has been added. ENDORSED BY GOVERNANCE COMMITTEE S:\Cancer Network\Guidelines\Guidelines and Pathways by Speciality\Chemotherapy\Current Approved Versions (Word & PDF)\Management of Extravasation version 2.0.doc Page 1 of 21 1 Scope of the Guideline This guidance has been produced to support the following: The prevention of the extravasation of intravenous anti-cancer drugs. The early detection of the extravasation of intravenous anti-cancer drugs. The treatment of the extravasation of intravenous anti-cancer drugs. 2 Guideline Statement Statement 2 The Network Site Specific Group has agreed to adopt the Royal Marsden Hospital Manual of Clinical Nursing Procedures 7th Edition; Blackwell Publishing (2008), chapter on extravasation, with the addition of a section on dexrazoxane. -

Review of Oral Iron Chelators (Deferiprone and Deferasirox) for the Treatment of Iron Overload in Pediatric Patients
Review of Oral Iron Chelators (Deferiprone and Deferasirox) for the Treatment of Iron Overload in Pediatric Patients D. Adam Algren, MD Assistant Professor of Pediatrics and Emergency Medicine Division of Pediatric Pharmacology and Medical Toxicology Departments of Pediatrics and Emergency Medicine Children’s Mercy Hospitals and Clinics/Truman Medical Center University of Missouri-Kansas City School of Medicine 1 PROPOSAL The World Health Organization Model List of Essential Medicines and Model Formulary 2010 list deferoxamine (DFO) as the treatment of choice for both acute and chronic iron poisoning. The Model Formulary currently does not designate any orally administered agents for the chelation of iron. It is proposed that deferasirox be considered the oral chelator of choice in the treatment of chronic iron overload. Deferasirox is widely available recent evidence support that it is both safe and efficacious. INTRODUCTION Acute iron poisoning and chronic iron overload result in significant morbidity and mortality worldwide. Treatment of acute iron poisoning and chronic iron overload can be challenging and care providers are often confronted with management dilemmas. Oral iron supplements are commonly prescribed for patients with iron deficiency anemia. The wide availability of iron supplements and iron-containing multivitamins provide easy accessibility for both adults and children. The approach to treatment of acute iron toxicity involves providing adequate supportive care, optimizing hemodynamic status and antidotal therapy with IV deferoxamine, when indicated.1 Early following an acute ingestion gastrointestinal (GI) decontamination can be potentially beneficial. Multiple options exist including: syrup of ipecac, gastric lavage, and whole bowel irrigation (WBI). Although definitive evidence that GI decontamination decreases morbidity and mortality is lacking it is often considered to be beneficial. -

Iron Chelating Agents
Pharmacy Benefit Coverage Criteria Effective Date ............................................ 1/1/2021 Next Review Date… ..................................... 1/1/2022 Coverage Policy Number ................................ P0090 Iron Chelating Agents Table of Contents Related Coverage Resources Medical Necessity Criteria ................................... 1 Dimercaprol and Edetate Calcium Disodium FDA Approved Indications ................................... 3 Penicillamine and trientene hydrochloride Recommended Dosing ........................................ 4 Background .......................................................... 8 References ........................................................ 11 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies are based. For example, a customer’s benefit plan document may -

Iron and Chelation in Biochemistry and Medicine: New Approaches to Controlling Iron Metabolism and Treating Related Diseases
cells Review Iron and Chelation in Biochemistry and Medicine: New Approaches to Controlling Iron Metabolism and Treating Related Diseases George J. Kontoghiorghes * and Christina N. Kontoghiorghe Postgraduate Research Institute of Science, Technology, Environment and Medicine, CY-3021 Limassol, Cyprus * Correspondence: [email protected]; Tel./Fax: +357-2627-2076 Received: 7 May 2020; Accepted: 5 June 2020; Published: 12 June 2020 Abstract: Iron is essential for all living organisms. Many iron-containing proteins and metabolic pathways play a key role in almost all cellular and physiological functions. The diversity of the activity and function of iron and its associated pathologies is based on bond formation with adjacent ligands and the overall structure of the iron complex in proteins or with other biomolecules. The control of the metabolic pathways of iron absorption, utilization, recycling and excretion by iron-containing proteins ensures normal biologic and physiological activity. Abnormalities in iron-containing proteins, iron metabolic pathways and also other associated processes can lead to an array of diseases. These include iron deficiency, which affects more than a quarter of the world’s population; hemoglobinopathies, which are the most common of the genetic disorders and idiopathic hemochromatosis. Iron is the most common catalyst of free radical production and oxidative stress which are implicated in tissue damage in most pathologic conditions, cancer initiation and progression, neurodegeneration and many other diseases. The interaction of iron and iron-containing proteins with dietary and xenobiotic molecules, including drugs, may affect iron metabolic and disease processes. Deferiprone, deferoxamine, deferasirox and other chelating drugs can offer therapeutic solutions for most diseases associated with iron metabolism including iron overload and deficiency, neurodegeneration and cancer, the detoxification of xenobiotic metals and most diseases associated with free radical pathology. -

Effect of Chromium(VI) on Serum Iron and Removal of Its Toxicity by Combining Deferasirox and Deferiprone Chelators in Rats
American Journal of Pharmacology and Toxicology 8 (4): 164-169, 2013 ISSN: 1557-4962 ©2013 Science Publication doi:10.3844/ajptsp.2013.164.169 Published Online 8 (4) 2013 (http://www.thescipub.com/ajpt.toc) Effect of Chromium(VI) on Serum Iron and Removal of its Toxicity by Combining Deferasirox and Deferiprone Chelators in Rats 1S. Jamil A. Fatemi, 1Marzieh Iranmanesh and 2Faezeh Dahooee Balooch 1Department of Chemistry, Faculty of Sciences, Islamic Azad University, Kerman Branch, Kerman, Iran 2Department of Chemistry, Faculty of Sciences, Shahid Bahonar University of Kerman, Kerman, Iran Received 2013-09-26, Revised 2013-10-21; Accepted 2013-10-30 ABSTRACT The present research is aimed to characterize the potential efficiency of two chelators after chromium(VI) administration for 60 days following two doses of 15 and 30 mg kg −1 chromium(VI) per body weight daily to male rats. However, the hypothesis that the two chelators might be more efficient as combined therapy than as single therapy in removing chromium(VI) from bood serum was considered. In this way, two known chelators deferasirox and deferiprone were chosen and tested in the acute rat model. Two chelators were given orally as a single or combined therapy for a period of one week. Chromium(VI) and iron concentrations in blood were determined by flame atomic absorption spectroscopy method. Chromium is one of the most widely used industrial metals. Several million workers worldwide are estimated to be exposed to chromium compounds in an array of industries. Chromium(VI) is more readily absorbed by both inhalation and oral routes. Ingestion of large amounts of chromium(VI) can lead to severe respiratory, cardiovascular, gastrointestinal, hepatic and renal damage and potentially death. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole