Anthracycline Chemotherapy and Cardiotoxicity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CHEMDNER-Patents: Chemical Entity Annotation Manual
CHEMDNER-patents: Chemical Entity annotation manual Version 2.0 (May 2015) This document describes the annotation guidelines used for the construction of the annotations chemical mentions (CEM – Chemical Entity Mention) of the CHEMDNER-patents corpus. These annotation guidelines were generated based on the CHEMDNER 2013 task exclusively focused on chemical entities extracted from papers. Thus, annotation guidelines were adapted to mine patents with a stronger focus on identifying any wide definition of chemical terms rather than in obtaining highly refined chemical mentions that can be univoquely translated into a chemical structure. The reason for this subtle refinement resides in the fact that patents contain very wide, general chemical mentions to describe the different substituents of the general Markush formula. Discarding this kind of mentions would prevent future applications (e.g. deconvolution and interpretation of Markush formula) of the CHEMDNER-patents corpus. However, no attempt is made to establish Markush structure relation: establishing meaningful correlations between the Markush formula and substituents. Thus, two related CEMs that are clearly separated as different entities in the text will be annotated as two different CEMs; although the meaning of one of them can be linked to the other one. This guide provides the basic details of the CEM task and the conventions that should be followed during the corpus construction process. The annotation guidelines were refined after iterative cycles of annotations of sample documents based on direct suggestions made by the curators as well as through the observation of inconsistencies detected when comparing the results provided by different curators. Some participating teams provided feedback to improve the documentation after the release of the first sample set prepared for the CHEMDNER 2013 task. -

And Cisplatin-Resistant Ovarian Cancer
Vol. 2, 607–610, July 2003 Molecular Cancer Therapeutics 607 Alchemix: A Novel Alkylating Anthraquinone with Potent Activity against Anthracycline- and Cisplatin-resistant Ovarian Cancer Klaus Pors, Zennia Paniwnyk, mediated stabilization of the topo II-DNA-cleavable complex Paul Teesdale-Spittle,1 Jane A. Plumb, and resulting in inhibition of poststrand passage DNA religa- Elaine Willmore, Caroline A. Austin, and tion (1). This event is not lethal per se but initiates a cascade 2 Laurence H. Patterson of events leading to cell death (2). Anthraquinones, as ex- Department of Pharmaceutical and Biological Chemistry, The School of emplified by mitoxantrone, are topo II inhibitors with proven Pharmacy, University of London, London WC1N 1AX, United Kingdom [K. P., L. H. P.]; Department of Pharmacy, De Montfort University, success for the treatment of advanced breast cancer, non- Leicester LE1 9BH, United Kingdom [Z. P., P. T. S.]; Cancer Research Hodgkin’s lymphoma, and acute leukemia (3). Intercalation is UK Department of Medical Oncology, University of Glasgow, Glasgow a crucial part of topo II inhibition by cytotoxic anthraquinones G61 1BD, United Kingdom [J. A. P.]; and School of Cell and Molecular Biosciences, The Medical School, University of Newcastle upon Tyne, with high affinity for DNA (4). It is likely that the potent Newcastle upon Tyne NE2 4HH, United Kingdom [E. W., C. A. A.] cytotoxicity of anthraquinones is related to their slow rate of dissociation from DNA, the kinetics of which favors long- term trapping of the topo-DNA complexes (5). However, Abstract currently available DNA intercalators at best promote a tran- Chloroethylaminoanthraquinones are described with sient inhibition of topo II, because the topo-drug-DNA ter- intercalating and alkylating capacity that potentially nary complex is reversed by removal of the intracellular drug covalently cross-link topoisomerase II (topo II) to DNA. -

Comparative Study of Deferiprone Versus Deferiprone with Deferasirox
BANGLADESH J CHILD HEALTH 2019; VOL 43 (3) : 152-156 Comparative study of Deferiprone versus Deferiprone with Deferasirox as iron chelation therapy in Thalassemic children SYEDA JARKA JAHIR1, SAYEEDA ANWAR2, AKM AMIRUL MORSHED3, AFIQUL ISLAM4, KABIRUL ISLAM5 Abstract Background: Combination therapy of Deferiprone (DFP) with Deferasirox (DFX) is an efficacious and safe modality to reduce serum ferritin in multi-transfused children with thalassemia. Objectives: To compare the efficacy of Deferiprone versus Deferiprone with Deferasirox as iron chelation therapy of transfusion dependent thalassemia children. Materials and Methods: A non-randomized control clinical trial was done in department of Pediatric Hematology and Oncology, Dhaka Medical College Hospital and Bangladesh Thalassemia Hospital in Dhaka during the period of October 2016 to September 2017. Thirty children with transfusion dependent thalassemia major between 3 to 12 years of age were included in each group in this study. Children with thalassemia minor, after splenectomy, with comorbidities and on other iron chelation therapy were excluded from this study. Results: Among total enrolled 60 cases in this study, initial mean serum ferritin level was 3397.48 ± 774.48 ng/ml in DFP-monotherapy group and 3413.70 ± 1114.05ng/ ml in DFP-DFX combination group. Mean serum ferritin level at 6thmonth was found 2730.63 ± 839.91ng/ml in DFP-monotherapy group and 1654.20 ± 934.90 ng/ml in DFP-DFX-combination group which shows rapid reduction of serum ferritin level in DFP-DFX-combination group. 12 (40.0%) patients had arthralgia in DFP- monotherapy group and 5(16.7%) patients had vomiting in DFP-DFX-combination group. -

MEDICATION GUIDE FERRIPROX (Feh' Ri Prox) (Deferiprone) Oral
MEDICATION GUIDE FERRIPROX® (Feh’ ri prox) (deferiprone) oral solution What is the most important information I should know about FERRIPROX? FERRIPROX can cause serious side effects, including a very low white blood cell count in your blood. One type of white blood cell that is important for fighting infections is called a neutrophil. If your neutrophil count is low (neutropenia), you may be at risk of developing a serious infection that can lead to death. Neutropenia is common with FERRIPROX and can become severe in some people. Severe neutropenia is known as agranulocytosis. If you develop agranulocytosis, you will be at risk of developing serious infections that can lead to death. Your healthcare provider should do a blood test before you start FERRIPROX and weekly during treatment to check your neutrophil count. If you develop neutropenia, your healthcare provider should check your blood counts every day until your white blood cell count improves. Stop taking FERRIPROX and get medical help right away if you develop any of these symptoms of infection: •fever • sore throat or mouth sores • flu-like symptoms • chills and severe shaking. See “What are the possible side effects of FERRIPROX?” for more information about side effects. What is FERRIPROX? FERRIPROX is a prescription medicine used to treat people with thalassemia syndromes who have iron overload from blood transfusions, when current iron removal (chelation) therapy does not work well enough. It is not known if FERRIPROX is safe and effective: • to treat iron overload due to blood transfusions in people with any other type of anemia that is long lasting (chronic) • in children Who should not take FERRIPROX? Do not take FERRIPROX if you are allergic to deferiprone or any of the ingredients in FERRIPROX. -

5-Fluorouracil + Adriamycin + Cyclophosphamide) Combination in Differentiated H9c2 Cells
Article Doxorubicin Is Key for the Cardiotoxicity of FAC (5-Fluorouracil + Adriamycin + Cyclophosphamide) Combination in Differentiated H9c2 Cells Maria Pereira-Oliveira, Ana Reis-Mendes, Félix Carvalho, Fernando Remião, Maria de Lourdes Bastos and Vera Marisa Costa * UCIBIO, REQUIMTE, Laboratory of Toxicology, Faculty of Pharmacy, University of Porto, Rua de Jorge Viterbo Ferreira, 228, 4050-313 Porto, Portugal; [email protected] (M.P.-O.); [email protected] (A.R.-M.); [email protected] (F.C.); [email protected] (F.R.); [email protected] (M.L.B.) * Correspondence: [email protected] Received: 4 October 2018; Accepted: 3 January 2019; Published: 10 January 2019 Abstract: Currently, a common therapeutic approach in cancer treatment encompasses a drug combination to attain an overall better efficacy. Unfortunately, it leads to a higher incidence of severe side effects, namely cardiotoxicity. This work aimed to assess the cytotoxicity of doxorubicin (DOX, also known as Adriamycin), 5-fluorouracil (5-FU), cyclophosphamide (CYA), and their combination (5-Fluorouracil + Adriamycin + Cyclophosphamide, FAC) in H9c2 cardiac cells, for a better understanding of the contribution of each drug to FAC-induced cardiotoxicity. Differentiated H9c2 cells were exposed to pharmacological relevant concentrations of DOX (0.13–5 μM), 5-FU (0.13–5 μM), CYA (0.13–5 μM) for 24 or 48 h. Cells were also exposed to FAC mixtures (0.2, 1 or 5 μM of each drug and 50 μM 5-FU + 1 μM DOX + 50 μM CYA). DOX was the most cytotoxic drug, followed by 5-FU and lastly CYA in both cytotoxicity assays (reduction of 3-(4,5-dimethylthiazol-2- yl)-2,5-diphenyl tetrazolium bromide (MTT) and neutral red (NR) uptake). -

Thames Valley Chemotherapy Regimens Sarcoma
Thames Valley Thames Valley Chemotherapy Regimens Sarcoma Chemotherapy Regimens– Sarcoma 1 of 98 Thames Valley Notes from the editor All chemotherapy regimens, and associated guidelines eg antiemetics and dose bands are available on the Network website www.tvscn.nhs.uk/networks/cancer-topics/chemotherapy/ Any correspondence about the regimens should be addressed to: Sally Coutts, Cancer Pharmacist, Thames Valley email: [email protected] Acknowledgements These regimens have been compiled by the Network Pharmacy Group in collaboration with key contribution from Prof Bass Hassan, Medical Oncologist, OUH Dr Sally Trent, Clinical Oncologist, OUH Dr James Gildersleve, Clinical Oncologist, RBFT Dr Sarah Pratap, Medical Oncologist, OUH Dr Shaun Wilson, TYA - Paediatric Oncologist, OUH Catherine Chaytor, Cancer Pharmacist, OUH Varsha Ormerod, Cancer Pharmacist, OUH Kristen Moorhouse, Cancer Pharmacist, OUH © Thames Valley Cancer Network. All rights reserved. Not to be reproduced in whole or in part without the permission of the copyright owner. Chemotherapy Regimens– Sarcoma 2 of 98 Thames Valley Thames Valley Chemotherapy Regimens Sarcoma Network Chemotherapy Regimens used in the management of Sarcoma Date published: January 2019 Date of review: June 2022 Chemotherapy Regimens Name of regimen Indication Page List of amendments to this version 5 Imatinib GIST 6 Sunitinib GIST 9 Regorafenib GIST 11 Paclitaxel weekly (Taxol) Angiosarcoma 13 AC Osteosarcoma 15 Cisplatin Imatinib – if local Trust funding agreed Chordoma 18 Doxorubicin Sarcoma 21 -

Current Biomedical Use of Copper Chelation Therapy
International Journal of Molecular Sciences Review Current Biomedical Use of Copper Chelation Therapy Silvia Baldari 1,2, Giuliana Di Rocco 1 and Gabriele Toietta 1,* 1 Department of Research, Advanced Diagnostic, and Technological Innovation, IRCCS Regina Elena National Cancer Institute, via E. Chianesi 53, 00144 Rome, Italy; [email protected] (S.B.); [email protected] (G.D.R.) 2 Department of Medical Surgical Sciences and Biotechnologies, University of Rome “La Sapienza”, C.so della Repubblica 79, 04100 Latina, Italy * Correspondence: [email protected]; Tel.: +39-06-5266-2604 Received: 9 January 2020; Accepted: 4 February 2020; Published: 6 February 2020 Abstract: Copper is an essential microelement that plays an important role in a wide variety of biological processes. Copper concentration has to be finely regulated, as any imbalance in its homeostasis can induce abnormalities. In particular, excess copper plays an important role in the etiopathogenesis of the genetic disease Wilson’s syndrome, in neurological and neurodegenerative pathologies such as Alzheimer’s and Parkinson’s diseases, in idiopathic pulmonary fibrosis, in diabetes, and in several forms of cancer. Copper chelating agents are among the most promising tools to keep copper concentration at physiological levels. In this review, we focus on the most relevant compounds experimentally and clinically evaluated for their ability to counteract copper homeostasis deregulation. In particular, we provide a general overview of the main disorders characterized by a pathological increase in copper levels, summarizing the principal copper chelating therapies adopted in clinical trials. Keywords: copper; chelation therapy; therapeutic chelation; metal homeostasis; cancer; metalloproteins 1. -

Chelation Therapy
Corporate Medical Policy Chelation Therapy File Name: chelation_therapy Origination: 12/1995 Last CAP Review: 2/2021 Next CAP Review: 2/2022 Last Review: 2/2021 Description of Procedure or Service Chelation therapy is an established treatment for the removal of metal toxins by converting them to a chemically inert form that can be excreted in the urine. Chelation therapy comprises intravenous or oral administration of chelating agents that remove metal ions such as lead, aluminum, mercury, arsenic, zinc, iron, copper, and calcium from the body. Specific chelating agents are used for particular heavy metal toxicities. For example, desferroxamine (not Food and Drug Administration [FDA] approved) is used for patients with iron toxicity, and calcium-ethylenediaminetetraacetic acid (EDTA) is used for patients with lead poisoning. Note that disodium-EDTA is not recommended for acute lead poisoning due to the increased risk of death from hypocalcemia. Another class of chelating agents, called metal protein attenuating compounds (MPACs), is under investigation for the treatment of Alzheimer’s disease, which is associated with the disequilibrium of cerebral metals. Unlike traditional systemic chelators that bind and remove metals from tissues systemically, MPACs have subtle effects on metal homeostasis and abnormal metal interactions. In animal models of Alzheimer’s disease, they promote the solubilization and clearance of β-amyloid protein by binding to its metal-ion complex and also inhibit redox reactions that generate neurotoxic free radicals. MPACs therefore interrupt two putative pathogenic processes of Alzheimer’s disease. However, no MPACs have received FDA approval for treating Alzheimer’s disease. Chelation therapy has also been investigated as a treatment for other indications including atherosclerosis and autism spectrum disorder. -

Cardiotoxicity of Doxorubicin Is Mediated Through Mitochondrial Iron Accumulation
Cardiotoxicity of doxorubicin is mediated through mitochondrial iron accumulation Yoshihiko Ichikawa, … , Tejaswitha Jairaj Naik, Hossein Ardehali J Clin Invest. 2014;124(2):617-630. https://doi.org/10.1172/JCI72931. Research Article Cardiology Doxorubicin is an effective anticancer drug with known cardiotoxic side effects. It has been hypothesized that doxorubicin- dependent cardiotoxicity occurs through ROS production and possibly cellular iron accumulation. Here, we found that cardiotoxicity develops through the preferential accumulation of iron inside the mitochondria following doxorubicin treatment. In isolated cardiomyocytes, doxorubicin became concentrated in the mitochondria and increased both mitochondrial iron and cellular ROS levels. Overexpression of ABCB8, a mitochondrial protein that facilitates iron export, in vitro and in the hearts of transgenic mice decreased mitochondrial iron and cellular ROS and protected against doxorubicin-induced cardiomyopathy. Dexrazoxane, a drug that attenuates doxorubicin-induced cardiotoxicity, decreased mitochondrial iron levels and reversed doxorubicin-induced cardiac damage. Finally, hearts from patients with doxorubicin-induced cardiomyopathy had markedly higher mitochondrial iron levels than hearts from patients with other types of cardiomyopathies or normal cardiac function. These results suggest that the cardiotoxic effects of doxorubicin develop from mitochondrial iron accumulation and that reducing mitochondrial iron levels protects against doxorubicin- induced cardiomyopathy. Find the latest version: https://jci.me/72931/pdf Research article Cardiotoxicity of doxorubicin is mediated through mitochondrial iron accumulation Yoshihiko Ichikawa,1 Mohsen Ghanefar,1 Marina Bayeva,1 Rongxue Wu,1 Arineh Khechaduri,1 Sathyamangla V. Naga Prasad,2 R. Kannan Mutharasan,1 Tejaswitha Jairaj Naik,1 and Hossein Ardehali1 1Feinberg Cardiovascular Institute, Northwestern University School of Medicine, Chicago, Illinois, USA. -

ZINECARD® (Dexrazoxane) for Injection Regimens
HIGHLIGHTS OF PRESCRIBING INFORMATION ----------------------DOSAGE FORMS AND STRENGTHS------------- These highlights do not include all the information needed to use 250 mg or 500 mg single dose vials as sterile, pyrogen-free lyophilizates. (3) ZINECARD safely and effectively. See full prescribing information for ZINECARD. -------------------------------CONTRAINDICATIONS------------------------------ ZINECARD should not be used with non-anthracycline chemotherapy ZINECARD® (dexrazoxane) for injection regimens. (4) Initial U.S. Approval: 1995 -----------------------WARNINGS AND PRECAUTIONS------------------------ ---------------------------INDICATIONS AND USAGE----------------------- Myelosuppression: ZINECARD may increase the myelosuppresive ZINECARD is a cytoprotective agent indicated for reducing the incidence and effects of chemotherapeutic agents. Perform hematological monitoring. severity of cardiomyopathy associated with doxorubicin administration in (5.1) women with metastatic breast cancer who have received a cumulative Embryo-Fetal Toxicity: Can cause fetal harm. Advise female patients of doxorubicin dose of 300 mg/m2 and who will continue to receive doxorubicin reproductive potential of the potential hazard to the fetus. (5.5, 8.1) therapy to maintain tumor control. Do not use ZINECARD with doxorubicin initiation. (1) ------------------------------ADVERSE REACTIONS------------------------------- In clinical studies, ZINECARD was administered to patients also receiving -----------------------DOSAGE AND ADMINISTRATION---------------------- chemotherapeutic agents for cancer. Pain on injection was observed more Reconstitute vial contents and dilute before use. (2.3) frequently in patients receiving ZINECARD versus placebo. (6.1) Administer ZINECARD by intravenous infusion over 15 minutes. DO NOT ADMINISTER VIA AN INTRAVENOUS PUSH. (2.1, 2.3) To report SUSPECTED ADVERSE REACTIONS, contact Pfizer, Inc. at The recommended dosage ratio of ZINECARD to doxorubicin is 10:1 1-800-438-1985 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. -

Cardioprotective Effects of Exercise Training on Doxorubicin-Induced
www.nature.com/scientificreports OPEN Cardioprotective efects of exercise training on doxorubicin‑induced cardiomyopathy: a systematic review with meta‑analysis of preclinical studies Paola Victória da Costa Ghignatti, Laura Jesuíno Nogueira, Alexandre Machado Lehnen & Natalia Motta Leguisamo* Doxorubicin (DOX)‑induced cardiotoxicity in chemotherapy is a major treatment drawback. Clinical trials on the cardioprotective efects of exercise in cancer patients have not yet been published. Thus, we conducted a systematic review and meta‑analysis of preclinical studies for to assess the efcacy of exercise training on DOX‑induced cardiomyopathy. We included studies with animal models of DOX‑induced cardiomyopathy and exercise training from PubMed, Web of Sciences and Scopus databases. The outcome was the mean diference (MD) in fractional shortening (FS, %) assessed by echocardiography between sedentary and trained DOX‑treated animals. Trained DOX‑treated animals improved 7.40% (95% CI 5.75–9.05, p < 0.001) in FS vs. sedentary animals. Subgroup analyses revealed a superior efect of exercise training execution prior to DOX exposure (MD = 8.20, 95% CI 6.27–10.13, p = 0.010). The assessment of cardiac function up to 10 days after DOX exposure and completion of exercise protocol was also associated with superior efect size in FS (MD = 7.89, 95% CI 6.11–9.67, p = 0.020) vs. an echocardiography after over 4 weeks. Modality and duration of exercise, gender and cumulative DOX dose did were not individually associated with changes on FS. Exercise training is a cardioprotective approach in rodent models of DOX‑induced cardiomyopathy. Exercise prior to DOX exposure exerts greater efect sizes on FS preservation. -
Guideline for the Management of Extravasation
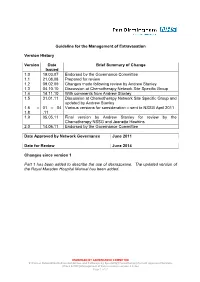
Guideline for the Management of Extravasation Version History Version Date Brief Summary of Change Issued 1.0 19.03.07 Endorsed by the Governance Committee 1.1 21.08.08 Prepared for review 1.2 09.02.09 Changes made following review by Andrew Stanley 1.3 04.10.10 Discussion at Chemotherapy Network Site Specific Group 1.4 14.11.10 With comments from Andrew Stanley 1.5 31.01.11 Discussion at Chemotherapy Network Site Specific Group and updated by Andrew Stanley 1.6 – 01 – 04 Various versions for consideration – sent to NSSG April 2011 1.8 .11 1.9 05.05.11 Final version by Andrew Stanley for review by the Chemotherapy NSSG and Jeanette Hawkins 2.0 14.06.11 Endorsed by the Governance Committee Date Approved by Network Governance June 2011 Date for Review June 2014 Changes since version 1 Part 1 has been added to describe the use of dexrazoxane. The updated version of the Royal Marsden Hospital Manual has been added. ENDORSED BY GOVERNANCE COMMITTEE S:\Cancer Network\Guidelines\Guidelines and Pathways by Speciality\Chemotherapy\Current Approved Versions (Word & PDF)\Management of Extravasation version 2.0.doc Page 1 of 21 1 Scope of the Guideline This guidance has been produced to support the following: The prevention of the extravasation of intravenous anti-cancer drugs. The early detection of the extravasation of intravenous anti-cancer drugs. The treatment of the extravasation of intravenous anti-cancer drugs. 2 Guideline Statement Statement 2 The Network Site Specific Group has agreed to adopt the Royal Marsden Hospital Manual of Clinical Nursing Procedures 7th Edition; Blackwell Publishing (2008), chapter on extravasation, with the addition of a section on dexrazoxane.