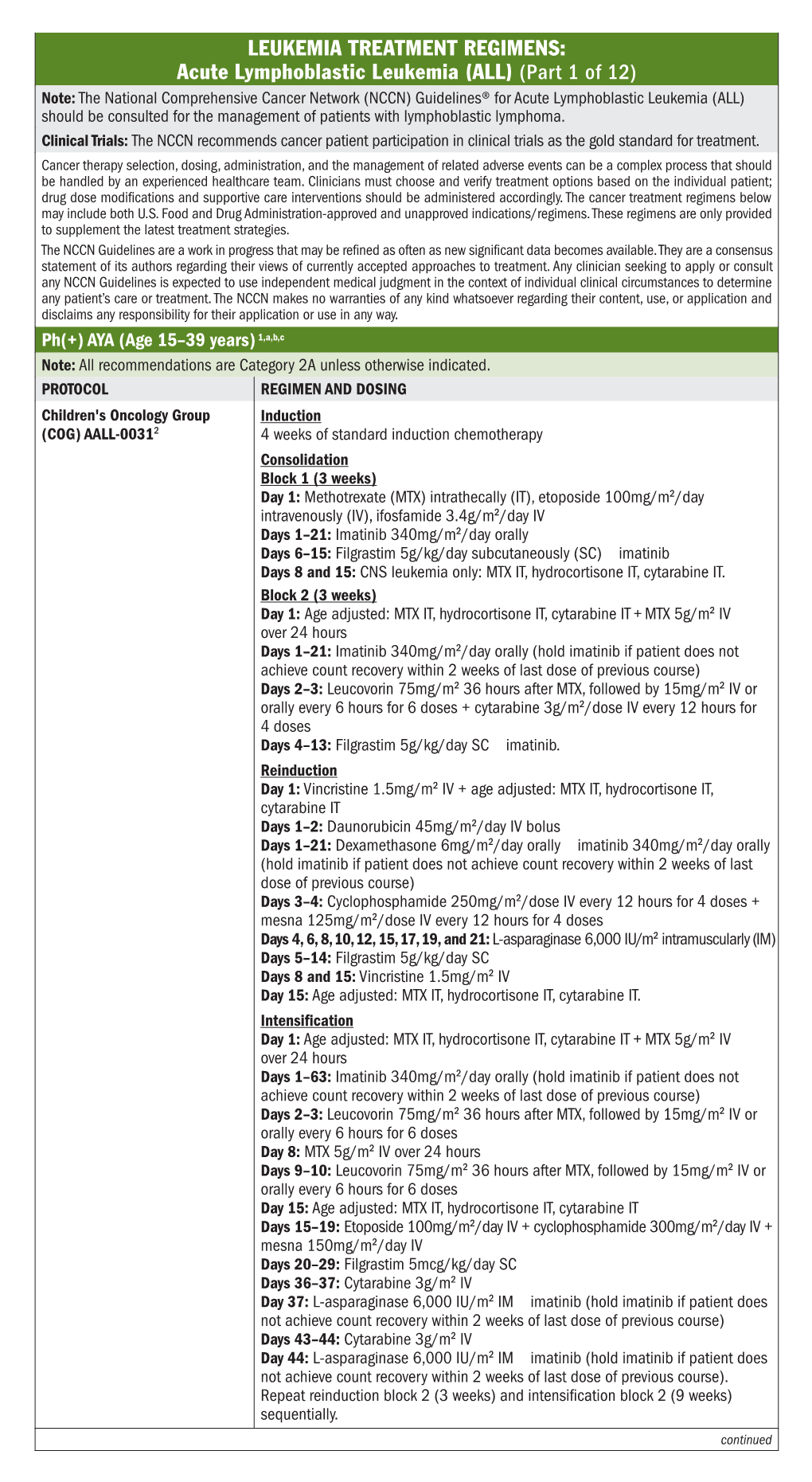
Acute Lymphoblastic Leukemia (ALL) (Part 1 Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Treatment of Localized Extranodal NK/T Cell Lymphoma, Nasal Type: a Systematic Review Seok Jin Kim†, Sang Eun Yoon† and Won Seog Kim*
Kim et al. Journal of Hematology & Oncology (2018) 11:140 https://doi.org/10.1186/s13045-018-0687-0 REVIEW Open Access Treatment of localized extranodal NK/T cell lymphoma, nasal type: a systematic review Seok Jin Kim†, Sang Eun Yoon† and Won Seog Kim* Abstract Extranodal natural killer/T cell lymphoma (ENKTL), nasal type, presents predominantly as a localized disease involving the nasal cavity and adjacent sites, and the treatment of localized nasal ENKTL is a major issue. However, given its rarity, there is no standard therapy based on randomized controlled trials and therefore a lack of consensus on the treatment of localized nasal ENKTL. Currently recommended treatments are based mainly on the results of phase II studies and retrospective analyses. Because the previous outcomes of anthracycline-containing chemotherapy were poor, non- anthracycline-based chemotherapy regimens, including etoposide and L-asparaginase, have been used mainly for patients with localized nasal ENKTL. Radiotherapy also has been used as a main component of treatment because it can produce a rapid response. Accordingly, the combined approach of non-anthracycline-based chemotherapy with radiotherapy is currently recommended as a first-line treatment for localized nasal ENKTL. This review summarizes the different approaches for the use of non-anthracycline-based chemotherapy with radiotherapy including concurrent, sequential, and sandwich chemoradiotherapy, which have been proposed as a first-line treatment for newly diagnosed patients with localized nasal ENKTL. Keywords: Extranodal NK/T cell lymphoma, Chemoradiotherapy, Localized disease Background Treatment for newly diagnosed patients with localized Extranodal natural killer/T cell lymphoma (ENKTL), nasal nasal ENKTL type, is a rare subtype of non-Hodgkin lymphoma [1]. -

A Pilot Trial of Clofarabine Added to Standard Busulfan and Fludarabine for Conditioning Prior to Allogeneic Hematopoietic Cell Transplantation
NCT# 01596699 A Pilot Trial of Clofarabine Added to Standard Busulfan and Fludarabine for Conditioning Prior to Allogeneic Hematopoietic Cell Transplantation Protocol Number: CC #110819 Version Number: 7.0 Version Date: June 6, 2013 Study Drug: Clofarabine Principal Investigator (Sponsor-Investigator) Christopher C. Dvorak, MD Co-Investigators Janel Long-Boyle, PharmD, PhD Morton Cowan, MD Biljana Horn, MD James Huang, MD Robert Goldsby, MD Kristin Ammon, MD Justin Wahlstrom, MD Statistician Stephen Shiboski, PhD Clinical Research Coordinator Revision History Version #1.0 9/19/11 Version #2.0 11/8/11 Version #3.1 02/23/12 Version #4.0 04/10/12 Version #5.0 04/30/12 Version #6.0 08/09/12 Version #7.0 06/07/13 Clofarabine Version 4.0, 04/10/12 Page 1 of 33 1.0 Hypothesis and Specific Aims: 1.1 Hypothesis: The addition of Clofarabine to standard Busulfan and Fludarabine prior to allogeneic hematopoietic cell transplant (HCT) will be safe and will improve engraftment rates of children with non-malignant diseases or decrease relapse rates of patients with high-risk myeloid malignancies. 1.2 Specific Aims: 1.2.1 Primary Objective: To determine the toxicity of the addition of Clofarabine to a conditioning backbone of Busulfan plus Fludarabine in patients with myeloid malignancies and non-malignant diseases undergoing allogeneic HCT. 1.2.2 Secondary Objectives: a. To determine if the addition of Clofarabine to a conditioning backbone of Busulfan plus Fludarabine improves the engraftment rate of patients with non-malignant diseases (Stratum A) undergoing allogeneic HCT as compared to historic controls. -

214120Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 214120Orig1s000 MULTI-DISCIPLINE REVIEW Summary Review Office Director Cross Discipline Team Leader Review Clinical Review Non-Clinical Review Statistical Review Clinical Pharmacology Review NDA Multidisciplinary Review and Evaluation Application Number NDA 214120 Application Type Type 3 Priority or Standard Priority Submit Date 3/3/2020 Received Date 3/3/2020 PDUFA Goal Date 9/3/2020 Office/Division OOD/DHM1 Review Completion Date 9/1/2020 Applicant Celgene Corporation Established Name Azacitidine (Proposed) Trade Name Onureg Pharmacologic Class Nucleoside metabolic inhibitor Formulations Tablet (200 mg, 300 mg) (b) (4) Applicant Proposed Indication/Population Recommendation on Regulatory Regular approval Action Recommended Indication/ For continued treatment of adult patients with acute Population myeloid leukemia who achieved first complete remission (CR) or complete remission with incomplete blood count recovery (CRi) following intensive induction chemotherapy and are not able to complete intensive curative therapy. SNOMED CT for the Recommended 91861009 Indication/Population Recommended Dosing Regimen 300 mg orally daily on Days 1 through 14 of each 28-day cycle Reference ID: 4664570 NDA Multidisciplinary Review and Evaluation NDA 214120 Onureg (azacitidine tablets) TABLE OF CONTENTS TABLE OF CONTENTS ................................................................................................................................... 2 TABLE OF TABLES ....................................................................................................................................... -

Clofarabine/Busulfan-Based Reduced Intensity
www.oncotarget.com Oncotarget, 2018, Vol. 9, (No. 93), pp: 36603-36612 Research Paper Clofarabine/busulfan-based reduced intensity conditioning regimens provides very good survivals in acute myeloid leukemia patients in complete remission at transplant: a retrospective study on behalf of the SFGM-TC Amandine Le Bourgeois1, Myriam Labopin2, Mathieu Leclerc3, Régis Peffault de Latour4, Jean-Henri Bourhis5, Patrice Ceballos6, Corentin Orvain7, Hélène Labussière Wallet8, Karin Bilger9, Didier Blaise10, Marie-Thérese Rubio11, Thierry Guillaume1, Mohamad Mohty2, Patrice Chevallier1 and on behalf of Société Francophone de Greffe de Moelle et de Thérapie Cellulaire 1Department of Hematology, CHU Hôtel Dieu, Nantes, France 2Department of Hematology, Hôpital Saint Antoine, Paris, France 3Department of Hematology, Hôpital Henri Mondor, Créteil, France 4Department of Hematology, Hôpital Saint Louis, Université Paris 7, Denis Diderot, Paris, France 5Department of Hematology, Hôpital Gustave Roussy, Paris, France 6Department of Hematology, CHU de Montpellier, Montpellier, France 7Department of Hematology, CHU d’Angers, Angers, France 8Department of Hematology, Centre Hospitalier Lyon Sud, Lyon, France 9Department of Hematology, CHU Strasbourg, Strasbourg, France 10Department of Hematology, Centre de Recherche en Cancérologie de Marseille, Institut Paoli Calmettes, Marseille, France 11Department of Hematology, CHU Nancy, Nancy, France Correspondence to: Amandine Le Bourgeois, email: [email protected] Patrice Chevallier, email: [email protected] Keywords: allogeneic stem cell transplantation; clofarabine; busulfan; reduced intensity conditioning regimen; acute myeloid leukemia Received: August 24, 2018 Accepted: November 01, 2018 Published: November 27, 2018 Copyright: Bourgeois et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License 3.0 (CC BY 3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. -
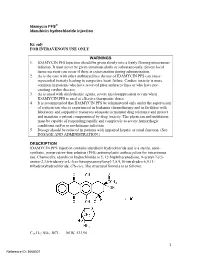
Idamycin PFS® Idarubicin Hydrochloride Injection
Idamycin PFS® idarubicin hydrochloride injection Rx only FOR INTRAVENOUS USE ONLY WARNINGS 1. IDAMYCIN PFS Injection should be given slowly into a freely flowing intravenous infusion. It must never be given intramuscularly or subcutaneously. Severe local tissue necrosis can occur if there is extravasation during administration. 2. As is the case with other anthracyclines the use of IDAMYCIN PFS can cause myocardial toxicity leading to congestive heart failure. Cardiac toxicity is more common in patients who have received prior anthracyclines or who have pre- existing cardiac disease. 3. As is usual with antileukemic agents, severe myelosuppression occurs when IDAMYCIN PFS is used at effective therapeutic doses. 4. It is recommended that IDAMYCIN PFS be administered only under the supervision of a physician who is experienced in leukemia chemotherapy and in facilities with laboratory and supportive resources adequate to monitor drug tolerance and protect and maintain a patient compromised by drug toxicity. The physician and institution must be capable of responding rapidly and completely to severe hemorrhagic conditions and/or overwhelming infection. 5. Dosage should be reduced in patients with impaired hepatic or renal function. (See DOSAGE AND ADMINISTRATION.) DESCRIPTION IDAMYCIN PFS Injection contains idarubicin hydrochloride and is a sterile, semi- synthetic, preservative-free solution (PFS) antineoplastic anthracycline for intravenous use. Chemically, idarubicin hydrochloride is 5, 12-Naphthacenedione, 9-acetyl-7-[(3- amino-2,3,6-trideoxy-α-L-lyxo-hexopyranosyl)oxy]-7,8,9,10-tetrahydro-6,9,11- trihydroxyhydrochloride, (7S-cis). The structural formula is as follows: C26 H27 NO9 .HCL M.W. 533.96 1 Reference ID: 3668307 IDAMYCIN PFS is a sterile, red-orange, isotonic parenteral preservative-free solution, available in 5 mL (5 mg), 10 mL (10 mg) and 20 mL (20 mg) single-use-only vials. -

SYN-40585 SYNRIBO Digital PI, Pil and IFU 5/2021 V3.Indd
SYN-40585 CONTRAINDICATIONS HIGHLIGHTS OF PRESCRIBING INFORMATION None. These highlights do not include all the information needed to use SYNRIBO safely and WARNINGS AND PRECAUTIONS effectively. See full prescribing information for SYNRIBO. • Myelosuppression: Severe and fatal thrombocytopenia, neutropenia and anemia. Monitor SYNRIBO® (omacetaxine mepesuccinate) for injection, for subcutaneous use hematologic parameters frequently (2.3, 5.1). Initial U.S. Approval: 2012 • Bleeding: Severe thrombocytopenia and increased risk of hemorrhage. Fatal cerebral hemorrhage and severe, non-fatal gastrointestinal hemorrhage (5.1, 5.2). INDICATIONS AND USAGE Hyperglycemia: Glucose intolerance and hyperglycemia including hyperosmolar non-ketotic SYNRIBO for Injection is indicated for the treatment of adult patients with chronic or accelerated • hyperglycemia (5.3). phase chronic myeloid leukemia (CML) with resistance and/or intolerance to two or more Embryo-Fetal Toxicity: Can cause fetal harm. Advise females of reproductive potential of the tyrosine kinase inhibitors (TKI) (1). • potential risk to a fetus and to use an effective method of contraception (5.4, 8.1, 8.3). DOSAGE AND ADMINISTRATION ADVERSE REACTIONS Induction Dose: 1.25 mg/m2 administered by subcutaneous injection twice daily for • Most common adverse reactions (frequency ≥ 20%): thrombocytopenia, anemia, neutropenia, 14 consecutive days of a 28-day cycle (2.1). diarrhea, nausea, fatigue, asthenia, injection site reaction, pyrexia, infection, and lymphopenia Maintenance Dose: 1.25 mg/m2 administered by subcutaneous injection twice daily for • (6.1). 7 consecutive days of a 28-day cycle (2.2). • Dose modifications are needed for toxicity (2.3). To report SUSPECTED ADVERSE REACTIONS, contact Teva Pharmaceuticals at 1-888-483-8279 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. -
Mitomycin C: Indications for Use and Safe Practice in Ophthalmology Published by American Society of Ophthalmic Registered Nurses
Mitomycin C: Indications for Use and Safe Practice in Ophthalmology Published by American Society of Ophthalmic Registered Nurses Editor Susan Clouser, RN, MSN, CRNO American Society of Ophthalmic Registered Nurses 655 Beach Street, San Francisco, CA 94109 1 This publication includes independent authors’ guidelines for the safe use and handling of mitomycin C in ophthalmic practices. Readers should use these guidelines as a resource only. These guidelines should never take precedence over manufacturers’ recommended practices, facilities policies and procedures, or compliance with federal regulations. Information in this publication may assist facilities in developing policies and procedures specifc to their needs and practice environment. American Society of Ophthalmic Registered Nurses For questions regarding content or association issues contact ASORN at [email protected] or 1.415.561.8513. Copyright © 2011 by American Society of Ophthalmic Registered Nurses American Society of Ophthalmic Registered Nurses has the exclusive rights to reproduce this work, to prepare derivative works from this work, to publicly distribute this work, to publicly perform this work and to publicly display this work. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior written permission of American Society of Ophthalmic Registered Nurses. Printed in the United States of America 10 9 8 7 6 5 4 3 2 1 ACKNOWLEDGMENTS The development of this educational resource would not have been possible without the knowledge and expertise of the ophthalmologists and ophthalmic registered nurses who wrote the content and the subsequent reviewers who provided valuable input. -

The New Therapeutic Strategies in Pediatric T-Cell Acute Lymphoblastic Leukemia
International Journal of Molecular Sciences Review The New Therapeutic Strategies in Pediatric T-Cell Acute Lymphoblastic Leukemia Marta Weronika Lato 1 , Anna Przysucha 1, Sylwia Grosman 1, Joanna Zawitkowska 2 and Monika Lejman 3,* 1 Student Scientific Society, Laboratory of Genetic Diagnostics, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] (M.W.L.); [email protected] (A.P.); [email protected] (S.G.) 2 Department of Pediatric Hematology, Oncology and Transplantology, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 3 Laboratory of Genetic Diagnostics, Medical University of Lublin, 20-093 Lublin, Poland * Correspondence: [email protected] Abstract: Childhood acute lymphoblastic leukemia is a genetically heterogeneous cancer that ac- counts for 10–15% of T-cell acute lymphoblastic leukemia (T-ALL) cases. The T-ALL event-free survival rate (EFS) is 85%. The evaluation of structural and numerical chromosomal changes is important for a comprehensive biological characterization of T-ALL, but there are currently no ge- netic prognostic markers. Despite chemotherapy regimens, steroids, and allogeneic transplantation, relapse is the main problem in children with T-ALL. Due to the development of high-throughput molecular methods, the ability to define subgroups of T-ALL has significantly improved in the last few years. The profiling of the gene expression of T-ALL has led to the identification of T-ALL subgroups, and it is important in determining prognostic factors and choosing an appropriate treatment. Novel therapies targeting molecular aberrations offer promise in achieving better first remission with the Citation: Lato, M.W.; Przysucha, A.; hope of preventing relapse. -

Ciera L. Patzke, Alison P. Duffy, Vu H. Duong, Firas El Chaer 4, James A
Journal of Clinical Medicine Article Comparison of High-Dose Cytarabine, Mitoxantrone, and Pegaspargase (HAM-pegA) to High-Dose Cytarabine, Mitoxantrone, Cladribine, and Filgrastim (CLAG-M) as First-Line Salvage Cytotoxic Chemotherapy for Relapsed/Refractory Acute Myeloid Leukemia Ciera L. Patzke 1, Alison P. Duffy 1,2, Vu H. Duong 1,3, Firas El Chaer 4, James A. Trovato 2, Maria R. Baer 1,3, Søren M. Bentzen 1,3 and Ashkan Emadi 1,3,* 1 Greenebaum Comprehensive Cancer Center, University of Maryland, Baltimore, MD 21201, USA; [email protected] (C.L.P.); aduff[email protected] (A.P.D.); [email protected] (V.H.D.); [email protected] (M.R.B.); [email protected] (S.M.B.) 2 School of Pharmacy, University of Maryland, Baltimore, MD 21201, USA; [email protected] 3 School of Medicine, University of Maryland, Baltimore, MD 21201, USA 4 School of Medicine, University of Virginia, Charlottesville, VA 22908, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-410-328-2596 Received: 10 January 2020; Accepted: 13 February 2020; Published: 16 February 2020 Abstract: Currently, no standard of care exists for the treatment of relapsed or refractory acute myeloid leukemia (AML). We present our institutional experience with using either CLAG-M or HAM-pegA, a novel regimen that includes pegaspargase. This is a retrospective comparison of 34 patients receiving CLAG-M and 10 receiving HAM-pegA as first salvage cytotoxic chemotherapy in the relapsed or refractory setting. Composite complete response rates were 47.1% for CLAG-M and 90% for HAM-pegA (p = 0.027). -

A Comparison of Early Intensive Methotrexate/Mercaptopurine With
Leukemia (2001) 15, 1038–1045 2001 Nature Publishing Group All rights reserved 0887-6924/01 $15.00 www.nature.com/leu A comparison of early intensive methotrexate/mercaptopurine with early intensive alternating combination chemotherapy for high-risk B-precursor acute lymphoblastic leukemia: a Pediatric Oncology Group phase III randomized trial SJ Lauer1, JJ Shuster2, DH Mahoney Jr3, N Winick4, S Toledano5, L Munoz5, G Kiefer6, JD Pullen7, CP Steuber3 and BM Camitta6 1Emory University School of Medicine, Atlanta, GA; 2Pediatric Oncology Group Statistical Office and Department of Statistics, University of Florida, Gainesville, FL; 3Texas Children’s Cancer Center, Baylor College of Medicine, Houston, TX; 4University of Texas Southwestern Medical Center, Dallas, TX; 5University Miami School of Medicine, Miami, FL; 6Midwest Children’s Cancer Center, Milwaukee, WI; and 7University of Mississippi Medical Center Children’s Hospital, Jackson, MS, USA A prospective, randomized multicenter study was performed to to their risk for relapse and treatment strategies designed to evaluate the relative efficacy of two different concepts for early improve event-free survival (EFS). intensive therapy in a randomized trial of children with B-pre- cursor acute lymphoblastic leukemia (ALL) at high risk (HR) for It is believed that the leading causes of relapse in children relapse. Four hundred and ninety eligible children with HR-ALL with higher risk ALL (HR-ALL) are inadequate cell kill and were randomized on the Pediatric Oncology Group (POG) 9006 emergence of drug-resistant clones. Clinical trials using early phase III trial between 7 January 1991 and 12 January 1994. intensive myelosuppressive combination chemotherapy as After prednisone (PDN), vincristine (VCR), asparaginase (ASP) post-induction consolidation were designed to maximize cell and daunorubicin (DNR) induction, 470 patients received either 2 kill and address drug resistance. -

Nelarabine) Injection • Severe Neurologic Reactions Have Been Reported
HIGHLIGHTS OF PRESCRIBING INFORMATION --------------------- DOSAGE FORMS AND STRENGTHS -------------- These highlights do not include all the information needed to use 250 mg/50 mL (5 mg/mL) vial (3) ARRANON safely and effectively. See full prescribing information for -------------------------------CONTRAINDICATIONS------------------------ ARRANON. None. ----------------------- WARNINGS AND PRECAUTIONS ---------------- ARRANON (nelarabine) Injection • Severe neurologic reactions have been reported. Monitor for signs and Initial U.S. Approval: 2005 symptoms of neurologic toxicity. (5.1) WARNING: NEUROLOGIC ADVERSE REACTIONS • Hematologic Reactions: Complete blood counts including platelets should See full prescribing information for complete boxed warning. be monitored regularly. (5.2) Severe neurologic adverse reactions have been reported with the use of • Fetal harm can occur if administered to a pregnant woman. Women should ARRANON. These adverse reactions have included altered mental states be advised not to become pregnant when taking ARRANON. (5.3) including severe somnolence, central nervous system effects including ------------------------------ ADVERSE REACTIONS ----------------------- convulsions, and peripheral neuropathy ranging from numbness and The most common (≥ 20%) adverse reactions were: paresthesias to motor weakness and paralysis. There have also been • Adult: anemia, thrombocytopenia, neutropenia, nausea, diarrhea, reports of adverse reactions associated with demyelination, and ascending vomiting, constipation, fatigue, -

Burkitt Lymphoma
NON-HODGKIN LYMPHOMA TREATMENT REGIMENS: Burkitt Lymphoma (Part 1 of 3) Clinical Trials: The National Comprehensive Cancer Network recommends cancer patient participation in clinical trials as the gold standard for treatment. Cancer therapy selection, dosing, administration, and the management of related adverse events can be a complex process that should be handled by an experienced health care team. Clinicians must choose and verify treatment options based on the individual patient; drug dose modifications and supportive care interventions should be administered accordingly. The cancer treatment regimens below may include both U.S. Food and Drug Administration-approved and unapproved indications/regimens. These regimens are provided only to supplement the latest treatment strategies. These Guidelines are a work in progress that may be refined as often as new significant data become available. The NCCN Guidelines® are a consensus statement of its authors regarding their views of currently accepted approaches to treatment. Any clinician seeking to apply or consult any NCCN Guidelines® is expected to use independent medical judgment in the context of individual clinical circumstances to determine any patient’s care or treatment. The NCCN makes no warranties of any kind whatsoever regarding their content, use, or application and disclaims any responsibility for their application or use in any way. Induction Therapy—Low Risk Combination Regimens1,a Note: All recommendations are Category 2A unless otherwise indicated. REGIMEN DOSING CODOX-M