Sputum Smear-Positive Case
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Kanan of Myanmar Most of the Kanan People Live in Banmauk Township
People and Language Detail Profile Profile Year: 2011 Language Name: Kanan ISO Language Code: zkn The Kanan of Myanmar Most of the Kanan people live in Banmauk Township. The Kanan live along the Mu River, to the southwest of the Kadu area. A few Kanan also live in Pinlebu Township, but this area is not connected to the Kanan majority area. It is not known how many Kanan live in Pinlebu Township or how long they have lived there. Information gathered indicates that there are 1,730 Kanan households. Assuming an average of four to six people per household, a population estimate for the Kanan would be about 7,000 to 10,000 people. Kanan language varieties are reported to be similar to one another, with only slight differences in accent or speed. Nanza and Hoyaw va- rieties are reported to be Kanan prestige dialects. Kanan people frequently travel to other Kanan villages for busi- ness and visiting. There is also much intermarriage between geo- Primary Religion: graphically close Kanan villages. Christianity _______________________________________________________ The Kanan and Kadu report that they are similar in many ways, in Disciples (Matt 28:19): 0% their language, cultural traditions and everyday life. The traditional _______________________________________________________ skirt for Kanan women is completely black. Other differences include Churches: 0 housing and animistic beliefs and practices. However, the Kadu and _______________________________________________________ Kanan also express a sense of separate ethnolinguistic identity. -
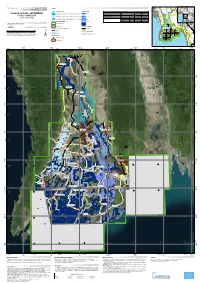
Damaged Health Facilities in the Flooded Areas Sagaing - (As of 18 August 2015)
Myanmar Information Management Unit Damaged Health Facilities in the Flooded Areas Sagaing - (As of 18 August 2015) 94° E 95° E 96° E N N ° ° 5 5 2 Nanyun Lay Shi 2 Lahe India Hkamti Homalin Lay Shi KACHIN Homalin Banmauk Homalin IndawKatha TamuPaungbyin PinlebuWuntho Tigyaing Mawlaik Kawlin India Kyunhla Kalewa Kanbalu Kale Taze Mingin Ye-U Khin-U TabayinShwebo Kani AyadawWetlet Yinmabin Pale MyinmuSagaing SalingyiMyaung Banmauk Banmauk Indaw Paungbyin Tamu Indaw Tamu Katha Paungbyin Ah Hlaw Pinlebu Katha Put Thar N Wuntho N ° ° 4 4 2 Pinlebu 2 Min Tha Mee Wuntho SAGAING Tigyaing Kawlin Myaung Gyi CHIN Kawlin Tigyaing Mawlaik Gway Tauk Taw Mawlaik Kyunhla Kale Kalewa Kyunhla In Daing Gyi Kyi Kone Kale Kalewa Kanbalu Zin Ka Le U Yin SHAN Kanbalu Kin Pun Chon (Kin Mun Chon) Taze Hto Mar Pauk Taw N N Inn Din ° ° 3 3 2 2 Kone Yin Taze Mingin Na Nwin Chaung Ye-U Pauk Aing Legend Kin Ye-U Khin-U State/Region Capital Mingin Khin-U Main Town Ohn Ma Tabayin Tabayin Type of Health Facilities District/Tsp Hospital Shwebo Shwebo Kani Station Hospital RMHCANDALAY Budalin Kani SRHC Budalin Wetlet Aing Taung Wetlet Type of Damage Ayadaw Fully Damaged Partially Damaged DAatyaa Sdaouwrces: Ministry of Health Base Map: MIMU Monywa Equipment Needs Yinmabin Boundaries: WFP/MIMU Monywa Township Damaged Place names: Ministry of Home Affairs Yinmabin Health Facilities (GAD) translated by MIMU Sagaing MAGWAY Township Boundary N N ° Map IDM: MyiInMmUu1326v01 ° 2 2 2 Pale Mandalay City 2 Salingyi Production Date: 10 September 2015, A3 State/Region Boundary Chaung-U Salingyi Pale Projection/Datum: MGyeinogmruaphic/WGS84 Chaung-U International Boundary Kilometers [email protected] Sagaing 0 10 20 40 www.themimu.info River and Stream Myaung 94° E 95° E Myaung 96° E Disclaimer: The names shown and the boundaries used on this map do not imply official endorsement or acceptance by the United Nations.. -

Usg Humanitarian Assistance to Burma
USG HUMANITARIAN ASSISTANCE TO BURMA RANGOON CITY AREA AFFECTED AREAS Affected Townships (as reported by the Government of Burma) American Red Cross aI SOURCE: MIMU ASEAN B Implementing NGO aD BAGO DIVISION IOM B Kyangin OCHA B (WEST) UNHCR I UNICEF DG JF Myanaung WFP E Seikgyikanaunglo WHO D UNICEF a WFP Ingapu DOD E RAKHINE b AYEYARWADY Dala STATE DIVISION UNICEF a Henzada WC AC INFORMA Lemyethna IC TI Hinthada PH O A N Rangoon R U G N O I T E G AYEYARWADY DIVISION ACF a U Zalun S A Taikkyi A D ID F MENTOR CARE a /DCHA/O D SC a Bago Yegyi Kyonpyaw Danubyu Hlegu Pathein Thabaung Maubin Twantay SC RANGOON a CWS/IDE AC CWS/IDE AC Hmawbi See Inset WC AC Htantabin Kyaunggon DIVISION Myaungmya Kyaiklat Nyaungdon Kayan Pathein Einme Rangoon SC/US JCa CWS/IDE AC Mayangone ! Pathein WC AC Î (Yangon) Thongwa Thanlyin Mawlamyinegyun Maubin Kyauktan Kangyidaunt Twantay CWS/IDE AC Myaungmya Wakema CWS/IDE Kyauktan AC PACT CIJ Myaungmya Kawhmu SC a Ngapudaw Kyaiklat Mawlamyinegyun Kungyangon UNDP/PACT C Kungyangon Mawlamyinegyun UNICEF Bogale Pyapon CARE a a Kawhmu Dedaye CWS/IDE AC Set San Pyapon Ngapudaw Labutta CWS/IDE AC UNICEF a CARE a IRC JEDa UNICEF a WC Set San AC SC a Ngapudaw Labutta Bogale KEY SC/US JCa USAID/OFDA USAID/FFP DOD Pyinkhayine Island Bogale A Agriculture and Food Security SC JC a Air Transport ACTED AC b Coordination and Information Management Labutta ACF a Pyapon B Economy and Market Systems CARE C !Thimphu ACTED a CARE Î AC a Emergency Food Assistance ADRA CWS/IDE AC CWS/IDE aIJ AC Emergency Relief Supplies Dhaka IOM a Î! CWS/IDE AC a UNICEF a D Health BURMA MERLIN PACT CJI DJ E Logistics PACT ICJ SC a Dedaye Vientiane F Nutrition Î! UNDP/PACT Rangoon SC C ! a Î ACTED AC G Protection UNDP/PACT C UNICEF a Bangkok CARE a IShelter and Settlements Î! UNICEF a WC AC J Water, Sanitation, and Hygiene WC WV GCJI AC 12/19/08 The boundaries and names used on this map do not imply official endorsement or acceptance by the U.S. -
Village Tract of Mandalay Region !
!. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. !. Myanmar Information Management Unit !. !. !. Village Tract of Mandalay Region !. !. !. !. 95° E 96° E Tigyaing !. !. !. / !. !. Inn Net Maing Daing Ta Gaung Taung Takaung Reserved Forest !. Reserved Forest Kyauk Aing Mabein !. !. !. !. Ma Gyi Kone Reserved !. Forest Thabeikkyin !. !. Reserved Forest !. Let Pan Kyunhla Kone !. Se Zin Kone !. Kyar Hnyat !. !. Kanbalu War Yon Kone !. !. !. Pauk Ta Pin Twin Nge Mongmit Kyauk Hpyu !. !. !. Kyauk Hpyar Yae Nyar U !. Kyauk Gyi Kyet Na !. Reserved Hpa Sa Bai Na Go Forest Bar Nat Li Shaw Kyauk Pon 23° N 23° Kyauk War N 23° Kyauk Gyi Li Shaw Ohn Dan Lel U !. Chaung Gyi !. Pein Pyit !. Kin Tha Dut !. Gway Pin Hmaw Kyauk Sin Sho !. Taze !. !. Than Lwin Taung Dun Taung Ah Shey Bawt Lone Gyi Pyaung Pyin !. Mogoke Kyauk Ka Paing Ka Thea Urban !. Hle Bee Shwe Ho Weik Win Ka Bar Nyaung Mogoke Ba Mun !. Pin Thabeikkyin Kyat Pyin !. War Yae Aye !. Hpyu Taung Hpyu Yaung Nyaung Nyaung Urban Htauk Kyauk Pin Ta Lone Pin Thar Tha Ohn Zone Laung Zin Pyay Lwe Ngin Monglon !. Ye-U Khin-U !. !. !. !. !. Reserved Forest Shwe Kyin !. !. Tabayin !. !. !. !. Shauk !. Pin Yoe Reserved !. Kyauk Myaung Nga Forest SAGAING !. Pyin Inn War Nat Taung Shwebo Yon !. Khu Lel Kone Mar Le REGION Singu Let Pan Hla !. Urban !. Koke Ko Singu Shwe Hlay Min !. Kyaung !. Seik Khet Thin Ngwe Taung MANDALAY Se Gyi !. Se Thei Nyaung Wun Taung Let Pan Kyar U Yin REGION Yae Taw Inn Kani Kone Thar !. !. Yar Shwe Pyi Wa Di Shwe Done !. Mya Sein Sin Htone Thay Gyi Shwe SHAN Budalin Hin Gon Taing Kha Tet !. Thar Nyaung Pin Chin Hpo Zee Pin Lel Wetlet Kyun Inn !. -

Lower Chindwin District Volume A
BURMA GAZETTEER LOWER CHINDWIN DISTRICT UPPER BURMA RANGOON OFFICE OF THE SUPERINTENDENT, GOVERNMENT PRINTING, BURMA TABLE OF CONTENTS. PAGE PART A. THE DISTRICT 1-211 Chapter I. Physical Description 1-20 Boundaries 1 The culturable portion 2 Rivers: the Chindwin; the Mu 3 The Alaungdaw gorge 4 Lakes ib. Diversity of the district ib. Area 5: Surveys ib. Geology 6 Petroliferous areas ib. Black-soil areas; red soils ib. Volcanic rocks 7 Explosion craters ib. Artesian wells 8 Saline efflorescence ib. Rainfall and climate 9 Fauna: quadrupeds; reptiles and lizards; game birds; predatory birds 9-15 Hunting: indigenous methods 16 Game fish 17 Hunting superstitions 18 Chapter II, History and Archæology 20-28 Early history 20 History after the Annexation of 1885 (a) east of the Chindwin; (b) west of the Chindwin: the southern portion; (c) the northern portion; (d) along the Chindwin 21-24 Archæology 24-28 The Register of Taya 25 CONTENTS. PAGE The Alaungdaw Katthapa shrine 25 The Powindaung caves 26 Pagodas ib. Inscriptions 27 Folk-lore: the Bodawgyi legend ib. Chapter III. The People 28-63 The main stock 28 Traces of admixture of other races ib. Population by census: densities; preponderance of females 29-32 Towns and large villages 32 Social and religious life: Buddhism and sects 33-35 The English Wesleyan Mission; Roman Catholics 35 Animism: the Alôn and Zidaw festivals 36 Caste 37 Standard of living: average agricultural income; the food of the people; the house; clothing; expenditure on works of public utility; agricultural stock 38-42 Agricultural indebtedness 42 Land values: sale and mortgage 48 Alienations to non-agriculturists 50 Indigence 51 Wages ib. -

TRENDS in MANDALAY Photo Credits
Local Governance Mapping THE STATE OF LOCAL GOVERNANCE: TRENDS IN MANDALAY Photo credits Paul van Hoof Mithulina Chatterjee Myanmar Survey Research The views expressed in this publication are those of the author, and do not necessarily represent the views of UNDP. Local Governance Mapping THE STATE OF LOCAL GOVERNANCE: TRENDS IN MANDALAY UNDP MYANMAR Table of Contents Acknowledgements II Acronyms III Executive Summary 1 1. Introduction 11 2. Methodology 14 2.1 Objectives 15 2.2 Research tools 15 3. Introduction to Mandalay region and participating townships 18 3.1 Socio-economic context 20 3.2 Demographics 22 3.3 Historical context 23 3.4 Governance institutions 26 3.5 Introduction to the three townships participating in the mapping 33 4. Governance at the frontline: Participation in planning, responsiveness for local service provision and accountability 38 4.1 Recent developments in Mandalay region from a citizen’s perspective 39 4.1.1 Citizens views on improvements in their village tract or ward 39 4.1.2 Citizens views on challenges in their village tract or ward 40 4.1.3 Perceptions on safety and security in Mandalay Region 43 4.2 Development planning and citizen participation 46 4.2.1 Planning, implementation and monitoring of development fund projects 48 4.2.2 Participation of citizens in decision-making regarding the utilisation of the development funds 52 4.3 Access to services 58 4.3.1 Basic healthcare service 62 4.3.2 Primary education 74 4.3.3 Drinking water 83 4.4 Information, transparency and accountability 94 4.4.1 Aspects of institutional and social accountability 95 4.4.2 Transparency and access to information 102 4.4.3 Civil society’s role in enhancing transparency and accountability 106 5. -

Mandalay Region Census Report Volume 3 – L
THE REPUBLIC OF THE UNION OF MYANMAR The 2014 Myanmar Population and Housing Census Mandalay Region Census Report Volume 3 – l Department of Population Ministry of Immigration and Population May 2015 The 2014 Myanmar Population and Housing Census Mandalay Region Report Census Report Volume 3 – I For more information contact: Department of Population Ministry of Immigration and Population Office No. 48 Nay Pyi Taw Tel: +95 67 431 062 www.dop.gov.mm May, 2015 Figure 2: Map of Mandalay Region, Districts and Townships ii Census Report Volume 3–I (Mandalay) Foreword The 2014 Myanmar Population and Housing Census (2014 MPHC) was conducted from 29th March to 10th April 2014 on a de facto basis. The successful planning and implementation of the census activities, followed by the timely release of the provisional results in August 2014 and now the main results in May 2015, is a clear testimony of the Government’s resolve to publish all information collected from respondents in accordance with the Population and Housing Census Law No. 19 of 2013. It is now my hope that the main results both Union and each of the State and Region reports will be interpreted correctly and will effectively inform the planning and decision-making processes in our quest for national and sub-national development. The census structures put in place, including the Central Census Commission, Census Committees and officers at the State/Region, District and Township levels and the International Technical Advisory Board (ITAB), a group of 15 experts from different countries and institutions involved in censuses and statistics internationally, provided the requisite administrative and technical inputs for the implementation of the census. -

Archaeologicl Evidences from Makkhaya Old City Min Lwin
Yadanabon University Research Journal 2019, Vol-10, No.1 1 Archaeologicl Evidences from Makkhaya Old City Min Lwin Abstract Makkhaya is among the ancient site of Myanmar old cities and various types of evidences related to earliest societies were found. Early people lived in Makkhaya period by period. Their traces were found in this site with many evidences. They are stone and wooden images of the Buddha, city wall, religious monuments, structure remains, stone inscription, wall painting, wood carving, human figure marked brick and animal figure marked brick and pot and potsherd, etc. Recent archaeological investigations on this site reveal its cultural levels associated not only with historical context, but with Prehistoric context of even Neolithic cultural level, passing through Metal Age, followed by Pyu Culture. Keywords: Religious monuments, Neolithic cultural level, passing through Metal Age, Pyu Culture. Introduction In Makkhaya region Pyu, Mon, Shan and Myanmar lived. But culture advanced in this site period by period. It can be found that structure remain, surface finds religious building and other ancient monuments. In this site many sources have been collected mainly on the datas and evidences such as background history, location and its environment, topography, burial remain, stone inscription and Old Mon village. Makkhaya ancient site is situated in Kyaukse plain, known as cultural context to historical character of Bagan and Post Bagan periods. In fact, lying at the junction of Zawgyi and Myit Nge Rivers, this area is provided by variety of environmental features of water supply and other lowland and highland natural resources – which serves as to the favourable condition for the early settlements. -

Mimu875v01 120626 3W Livelihoods South East
Myanmar Information Management Unit 3W South East of Myanmar Livelihoods Border and Country Based Organizations Presence by Township Budalin Thantlang 94°23'EKani Wetlet 96°4'E Kyaukme 97°45'E 99°26'E 101°7'E Ayadaw Madaya Pangsang Hakha Nawnghkio Mongyai Yinmabin Hsipaw Tangyan Gangaw SAGAING Monywa Sagaing Mandalay Myinmu Pale .! Pyinoolwin Mongyang Madupi Salingyi .! Matman CHINA Ngazun Sagaing Tilin 1 Tada-U 1 1 2 Monghsu Mongkhet CHIN Myaing Yesagyo Kyaukse Myingyan 1 Mongkaung Kyethi Mongla Mindat Pauk Natogyi Lawksawk Kengtung Myittha Pakokku 1 1 Hopong Mongping Taungtha 1 2 Mongyawng Saw Wundwin Loilen Laihka Ü Nyaung-U Kunhing Seikphyu Mahlaing Ywangan Kanpetlet 1 21°6'N Paletwa 4 21°6'N MANDALAY 1 1 Monghpyak Kyaukpadaung Taunggyi Nansang Meiktila Thazi Pindaya SHAN (EAST) Chauk .! Salin 4 Mongnai Pyawbwe 2 Tachileik Minbya Sidoktaya Kalaw 2 Natmauk Yenangyaung 4 Taunggyi SHAN (SOUTH) Monghsat Yamethin Pwintbyu Nyaungshwe Magway Pinlaung 4 Mawkmai Myothit 1 Mongpan 3 .! Nay Pyi Hsihseng 1 Minbu Taw-Tatkon 3 Mongton Myebon Langkho Ngape Magway 3 Nay Pyi Taw LAOS Ann MAGWAY Taungdwingyi [(!Nay Pyi Taw- Loikaw Minhla Nay Pyi Pyinmana 3 .! 3 3 Sinbaungwe Taw-Lewe Shadaw Pekon 3 3 Loikaw 2 RAKHINE Thayet Demoso Mindon Aunglan 19°25'N Yedashe 1 KAYAH 19°25'N 4 Thandaunggyi Hpruso 2 Ramree Kamma 2 3 Toungup Paukkhaung Taungoo Bawlakhe Pyay Htantabin 2 Oktwin Hpasawng Paungde 1 Mese Padaung Thegon Nattalin BAGOPhyu (EAST) BAGO (WEST) 3 Zigon Thandwe Kyangin Kyaukkyi Okpho Kyauktaga Hpapun 1 Myanaung Shwegyin 5 Minhla Ingapu 3 Gwa Letpadan -
The Union Report the Union Report : Census Report Volume 2 Census Report Volume 2
THE REPUBLIC OF THE UNION OF MYANMAR The 2014 Myanmar Population and Housing Census The Union Report The Union Report : Census Report Volume 2 Volume Report : Census The Union Report Census Report Volume 2 Department of Population Ministry of Immigration and Population May 2015 The 2014 Myanmar Population and Housing Census The Union Report Census Report Volume 2 For more information contact: Department of Population Ministry of Immigration and Population Office No. 48 Nay Pyi Taw Tel: +95 67 431 062 www.dop.gov.mm May, 2015 Figure 1: Map of Myanmar by State, Region and District Census Report Volume 2 (Union) i Foreword The 2014 Myanmar Population and Housing Census (2014 MPHC) was conducted from 29th March to 10th April 2014 on a de facto basis. The successful planning and implementation of the census activities, followed by the timely release of the provisional results in August 2014 and now the main results in May 2015, is a clear testimony of the Government’s resolve to publish all information collected from respondents in accordance with the Population and Housing Census Law No. 19 of 2013. It is my hope that the main census results will be interpreted correctly and will effectively inform the planning and decision-making processes in our quest for national development. The census structures put in place, including the Central Census Commission, Census Committees and Offices at all administrative levels and the International Technical Advisory Board (ITAB), a group of 15 experts from different countries and institutions involved in censuses and statistics internationally, provided the requisite administrative and technical inputs for the implementation of the census. -

MAGWAY REGION, MAGWAY DISTRICT Natmauk Township Report
THE REPUBLIC OF THE UNION OF MYANMAR The 2014 Myanmar Population and Housing Census MAGWAY REGION, MAGWAY DISTRICT Natmauk Township Report Department of Population Ministry of Labour, Immigration and Population October 2017 The 2014 Myanmar Population and Housing Census Magway Region, Magway District Natmauk Township Report Department of Population Ministry of Labour, Immigration and Population Office No.48 Nay Pyi Taw Tel: +95 67 431062 www.dop.gov.mm October 2017 Figure 1 : Map of Magway Region, showing the townships Natmauk Township Figures at a Glance 1 Total Population 206,996 2 Population males 92,774 (44.8%) Population females 114,222 (55.2%) Percentage of urban population 7.1% Area (Km2) 2,309.2 3 Population density (per Km2) 89.6 persons Median age 29.3 years Number of wards 7 Number of village tracts 73 Number of private households 48,426 Percentage of female headed households 27.7% Mean household size 4.2 persons 4 Percentage of population by age group Children (0 – 14 years) 29.3% Economically productive (15 – 64 years) 62.6% Elderly population (65+ years) 8.1% Dependency ratios Total dependency ratio 59.8 Child dependency ratio 46.8 Old dependency ratio 13.0 Ageing index 27.8 Sex ratio (males per 100 females) 81 Literacy rate (persons aged 15 and over) 87.6% Male 96.1% Female 81.4% People with disability Number Per cent Any form of disability 8,968 4.3 Walking 3,974 1.9 Seeing 4,841 2.3 Hearing 2,693 1.3 Remembering 3,062 1.5 Type of Identity Card (persons aged 10 and over) Number Per cent Citizenship Scrutiny 132,226 78.7 -
Irrawaddy Delta - MYANMAR Flooded Area Delineation 11/08/2015 11:46 UTC River R
Nepal (!Loikaw GLIDE number: N/A Activation ID: EMSR130 I Legend r n r India China e Product N.: 16IRRAWADDYDELTA, v2, English Magway a Rakhine w Bangladesh e a w l d a Vietnam Crisis Information Hydrology Consequences within the AOI on 09, 10, 11/08/2015 d Myanmar S Affected Total in AOI y Nay Pyi Taw Irrawaddy Delta - MYANMAR Flooded Area delineation 11/08/2015 11:46 UTC River R ha 428922,1 i v Laos Flooded area e ^ r S Flood - 01/08/2015 Flooded Area delineation 10/08/2015 23:49 UTC Stream Estimated population Inhabitants 4252141 11935674 it Bay of ( to Settlements Built-up area ha 35491,8 75542,0 A 10 Bago n Bengal Thailand y g Delineation Map e Flooded Area delineation 09/08/2015 11:13 UTC Lake y P Transportation Railways km 26,0 567,6 a Cambodia r i w Primary roads km 33,0 402,1 Andam an n a Gulf of General Information d Sea g Reservoir Secondary roads km 57,2 1702,3 Thailand 09 y Area of Interest ) Andam an Cartographic Information River Sea Missing data Transportation Bay of Bengal 08 Bago Tak Full color ISO A1, low resolution (100 dpi) 07 1:600000 Ayeyarwady Yangon (! Administrative boundaries Railway Kayin 0 12,5 25 50 Region km Primary Road Pathein 06 04 11 12 (! Province Mawlamyine Grid: WGS 1984 UTM Zone 46N map coordinate system Secondary Road 13 (! Tick marks: WGS 84 geographical coordinate system ± Settlements 03 02 01 ! Populated Place 14 15 Built-Up Area Gulf of Martaban Andaman Sea 650000 700000 750000 800000 850000 900000 950000 94°10'0"E 94°35'0"E 95°0'0"E 95°25'0"E 95°50'0"E 96°15'0"E 96°40'0"E 97°5'0"E N " 0 ' 5