Female Reproductive System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chapter 24 Primary Sex Organs = Gonads Produce Gametes Secrete Hormones That Control Reproduction Secondary Sex Organs = Accessory Structures
Anatomy Lecture Notes Chapter 24 primary sex organs = gonads produce gametes secrete hormones that control reproduction secondary sex organs = accessory structures Development and Differentiation A. gonads develop from mesoderm starting at week 5 gonadal ridges medial to kidneys germ cells migrate to gonadal ridges from yolk sac at week 7, if an XY embryo secretes SRY protein, the gonadal ridges begin developing into testes with seminiferous tubules the testes secrete androgens, which cause the mesonephric ducts to develop the testes secrete a hormone that causes the paramesonephric ducts to regress by week 8, in any fetus (XX or XY), if SRY protein has not been produced, the gondal ridges begin to develop into ovaries with ovarian follicles the lack of androgens causes the paramesonephric ducts to develop and the mesonephric ducts to regress B. accessory organs develop from embryonic duct systems mesonephric ducts / Wolffian ducts eventually become male accessory organs: epididymis, ductus deferens, ejaculatory duct paramesonephric ducts / Mullerian ducts eventually become female accessory organs: oviducts, uterus, superior vagina C. external genitalia are indeterminate until week 8 male female genital tubercle penis (glans, corpora cavernosa, clitoris (glans, corpora corpus spongiosum) cavernosa), vestibular bulb) urethral folds fuse to form penile urethra labia minora labioscrotal swellings fuse to form scrotum labia majora urogenital sinus urinary bladder, urethra, prostate, urinary bladder, urethra, seminal vesicles, bulbourethral inferior vagina, vestibular glands glands Strong/Fall 2008 Anatomy Lecture Notes Chapter 24 Male A. gonads = testes (singular = testis) located in scrotum 1. outer coverings a. tunica vaginalis =double layer of serous membrane that partially surrounds each testis; (figure 24.29) b. -
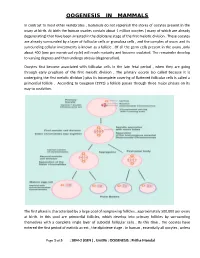
Oogenesis in Mammals
OOGENESIS IN MAMMALS In contrast to most other vertebrates , mammals do not replenish the stores of oocytes present in the ovary at birth. At birth the human ovaries contain about 1 million oocytes ( many of which are already degenerating) that have been arrested in the diplotene stage of the first meiotic division . These oocytes are already surrounded by a layer of follicular cells or granulosa cells , and the complex of ovum and its surrounding cellular investments is known as a follicle . Of all the germ cells present in the ovary ,only about 400 (one per menstrual cycle) will reach maturity and become ovulated. The remainder develop to varying degrees and then undergo atresia (degeneration). Oocytes first become associated with follicular cells in the late fetal period , when they are going through early prophase of the first meiotic division . The primary oocyte (so called because it is undergoing the first meiotic division ) plus its incomplete covering of flattened follicular cells is called a primordial follicle . According to Gougeon (1993) a follicle passes through three major phases on its way to ovulation. The first phase is characterized by a large pool of nongrowing follicles , approximately 500,000 per ovary at birth. In this pool are primordial follicles, which develop into primary follicles by surrounding themselves with a complete single layer of cuboidal follicular cells . By this time , the oocytes have entered the first period of meiotic arrest , the diplotene stage . In human , essentially all oocytes , unless Page 1 of 5 : SEM-2 (GEN ) , Unit#6 : OOGENESIS : Pritha Mondal they degenerate ,remain arrested in the diplotene stage until puberty ; some will not progress past the diplotene stage until the woman’s last reproductive cycle (age 45 to 55 years). -

FEMALE REPRODUCTIVE SYSTEM Female Reproduc�Ve System
Human Anatomy Unit 3 FEMALE REPRODUCTIVE SYSTEM Female Reproducve System • Gonads = ovaries – almond shaped – flank the uterus on either side – aached to the uterus and body wall by ligaments • Gametes = oocytes – released from the ovary during ovulaon – Develop within ovarian follicles Ligaments • Broad ligament – Aaches to walls and floor of pelvic cavity – Connuous with parietal peritoneum • Round ligament – Perpendicular to broad ligament • Ovarian ligament – Lateral surface of uterus ‐ ‐> medial surface of ovary • Suspensory ligament – Lateral surface of ovary ‐ ‐> pelvic wall Ovarian Follicles • Layers of epithelial cells surrounding ova • Primordial follicle – most immature of follicles • Primary follicle – single layer of follicular (granulosa) cells • Secondary – more than one layer and growing cavies • Graafian – Fluid filled antrum – ovum supported by many layers of follicular cells – Ovum surrounded by corona radiata Ovarian Follicles Corpus Luteum • Ovulaon releases the oocyte with the corona radiata • Leaves behind the rest of the Graafian follicle • Follicle becomes corpus luteum • Connues to secrete hormones to support possible pregnancy unl placenta becomes secretory or no implantaon • Becomes corpus albicans when no longer funconal Corpus Luteum and Corpus Albicans Uterine (Fallopian) Tubes • Ciliated tubes – Passage of the ovum to the uterus and – Passage of sperm toward the ovum • Fimbriae – finger like projecons that cover the ovary and sway, drawing the ovum inside aer ovulaon The Uterus • Muscular, hollow organ – supports -

A Case of Non-Communicating Uterine Horn Containing Functional Endometrium
logy & Ob o st ec e tr n i y c s G Rani et al., Gynecol Obstet (Sunnyvale) 2015, 5:9 Gynecology & Obstetrics DOI: 10.4172/2161-0932.1000320 ISSN: 2161-0932 Case Report Open Access A Case of Non-Communicating Uterine Horn Containing Functional Endometrium Anjali Rani*, Madhu Kumari and Shipra Department of Obstetrics and Gynaecology, Institute Of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India Abstract Uterine anoamalies are very rare. They can present with complains of amebnorrhoea, dysmenorrhoea, bad obstetrical outcome and infertility etc. Unicornuate uterus with rudimentary horn is very rare. The incidence of this is 1/100,000. Normally rudimentary horns are non- functional and non-communicating. But if they have functional endometrium they can develop hematometra. We are presenting a case of hematometra and pain in a patient with rudimentary non communicating horn with functional endometrium. Rudimentary horn should be kept as a differential diagnosis in pelvic pain. Keywords: Unicornuate uterus; Rudimentary horn; Dysmenorrhea were found in the pelvis. Exploratory laparotomy was decided and the rudimentary horn was excised by applying clamps (Figure 2). Histo- Introduction pathological examination of the specimen was reported as uterine Uterine anomalies are very rarely seen. Unicornuate uterus is a very udimentary horn with functional endometrium with haematometra. rare uterine anomaly. The incidence of congenital uterine anomalies The patient was discharged on the fifth postoperative day. She came in in fertile population is 1/200 to 1/600. The incidence of rudimentary follow up her nomal menses after 6 weeks. horn is very very rare (1:100,000). -

Ovarian Cancer Stroma: Pathophysiology and the Roles in Cancer Development
Cancers 2012, 4, 701-724; doi:10.3390/cancers4030701 OPEN ACCESS cancers ISSN 2072-6694 www.mdpi.com/journal/cancers Review Ovarian Cancer Stroma: Pathophysiology and the Roles in Cancer Development Mitsuko Furuya Department of Pathology, Yokohama City University Graduate School of Medicine, Yokohama 236-0004, Japan; E-Mail: [email protected]; Tel.: +81-45-787-2587; Fax: +81-45-786-0191 Received: 17 May 2012; in revised form: 29 June 2012 / Accepted: 12 July 2012 / Published: 18 July 2012 Abstract: Ovarian cancer represents one of the cancers with the worst prognostic in adult women. More than half of the patients who present with clinical signs such as abdominal bloating and a feeling of fullness already show advanced stages. The majority of ovarian cancers grow as cystic masses, and cancer cells easily spread into the pelvic cavity once the cysts rupture or leak. When the ovarian cancer cells disseminate into the peritoneal cavity, metastatic nests may grow in the cul-de-sac, and in more advanced stages, the peritoneal surfaces of the upper abdomen become the next largest soil for cancer progression. Ascites is also produced frequently in ovarian cancers, which facilitates distant metastasis. Clinicopathologic, epidemiologic and molecular studies on ovarian cancers have improved our understanding and therapeutic approaches, but still further efforts are required to reduce the risks in the patients who are predisposed to this lethal disease and the mortality of the patients in advanced stages. Among various molecules involved in ovarian carcinogenesis, special genes such as TP53, BRCA1 and BRCA2 have been well investigated. These genes are widely accepted as the predisposing factors that trigger malignant transformation of the epithelial cells of the ovary. -

Biology of the Corpus Luteum
PERIODICUM BIOLOGORUM UDC 57:61 VOL. 113, No 1, 43–49, 2011 CODEN PDBIAD ISSN 0031-5362 Review Biology of the Corpus luteum Abstract JELENA TOMAC \UR\ICA CEKINOVI] Corpus luteum (CL) is a small, transient endocrine gland formed fol- JURICA ARAPOVI] lowing ovulation from the secretory cells of the ovarian follicles. The main function of CL is the production of progesterone, a hormone which regu- Department of Histology and Embryology lates various reproductive functions. Progesterone plays a key role in the reg- Medical Faculty, University of Rijeka B. Branchetta 20, Rijeka, Croatia ulation of the length of estrous cycle and in the implantation of the blastocysts. Preovulatory surge of luteinizing hormone (LH) is crucial for Correspondence: the luteinization of follicular cells and CL maintenance, but there are also Jelena Tomac other factors which support the CL development and its functioning. In the Department of Histology and Embryology Medical Faculty, University of Rijeka absence of pregnancy, CL will cease to produce progesterone and induce it- B. Branchetta 20, Rijeka, Croatia self degradation known as luteolysis. This review is designed to provide a E-mail: [email protected] short overview of the events during the life span of corpus luteum (CL) and to make an insight in the synthesis and secretion of its main product – pro- Key words: Ovary, Corpus Luteum, gesterone. The major biologic mechanisms involved in CL development, Progesterone, Luteinization, Luteolysis function, and regression will also be discussed. INTRODUCTION orpus luteum (CL) is a transient endocrine gland, established by Cresidual follicular wall cells (granulosa and theca cells) following ovulation. -

Vocabulario De Morfoloxía, Anatomía E Citoloxía Veterinaria
Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) Servizo de Normalización Lingüística Universidade de Santiago de Compostela COLECCIÓN VOCABULARIOS TEMÁTICOS N.º 4 SERVIZO DE NORMALIZACIÓN LINGÜÍSTICA Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) 2008 UNIVERSIDADE DE SANTIAGO DE COMPOSTELA VOCABULARIO de morfoloxía, anatomía e citoloxía veterinaria : (galego-español- inglés) / coordinador Xusto A. Rodríguez Río, Servizo de Normalización Lingüística ; autores Matilde Lombardero Fernández ... [et al.]. – Santiago de Compostela : Universidade de Santiago de Compostela, Servizo de Publicacións e Intercambio Científico, 2008. – 369 p. ; 21 cm. – (Vocabularios temáticos ; 4). - D.L. C 2458-2008. – ISBN 978-84-9887-018-3 1.Medicina �������������������������������������������������������������������������veterinaria-Diccionarios�������������������������������������������������. 2.Galego (Lingua)-Glosarios, vocabularios, etc. políglotas. I.Lombardero Fernández, Matilde. II.Rodríguez Rio, Xusto A. coord. III. Universidade de Santiago de Compostela. Servizo de Normalización Lingüística, coord. IV.Universidade de Santiago de Compostela. Servizo de Publicacións e Intercambio Científico, ed. V.Serie. 591.4(038)=699=60=20 Coordinador Xusto A. Rodríguez Río (Área de Terminoloxía. Servizo de Normalización Lingüística. Universidade de Santiago de Compostela) Autoras/res Matilde Lombardero Fernández (doutora en Veterinaria e profesora do Departamento de Anatomía e Produción Animal. -

The Reproductive System
27 The Reproductive System PowerPoint® Lecture Presentations prepared by Steven Bassett Southeast Community College Lincoln, Nebraska © 2012 Pearson Education, Inc. Introduction • The reproductive system is designed to perpetuate the species • The male produces gametes called sperm cells • The female produces gametes called ova • The joining of a sperm cell and an ovum is fertilization • Fertilization results in the formation of a zygote © 2012 Pearson Education, Inc. Anatomy of the Male Reproductive System • Overview of the Male Reproductive System • Testis • Epididymis • Ductus deferens • Ejaculatory duct • Spongy urethra (penile urethra) • Seminal gland • Prostate gland • Bulbo-urethral gland © 2012 Pearson Education, Inc. Figure 27.1 The Male Reproductive System, Part I Pubic symphysis Ureter Urinary bladder Prostatic urethra Seminal gland Membranous urethra Rectum Corpus cavernosum Prostate gland Corpus spongiosum Spongy urethra Ejaculatory duct Ductus deferens Penis Bulbo-urethral gland Epididymis Anus Testis External urethral orifice Scrotum Sigmoid colon (cut) Rectum Internal urethral orifice Rectus abdominis Prostatic urethra Urinary bladder Prostate gland Pubic symphysis Bristle within ejaculatory duct Membranous urethra Penis Spongy urethra Spongy urethra within corpus spongiosum Bulbospongiosus muscle Corpus cavernosum Ductus deferens Epididymis Scrotum Testis © 2012 Pearson Education, Inc. Anatomy of the Male Reproductive System • The Testes • Testes hang inside a pouch called the scrotum, which is on the outside of the body -

Luteal Phase Deficiency: What We Now Know
■ OBGMANAGEMENT BY LAWRENCE ENGMAN, MD, and ANTHONY A. LUCIANO, MD Luteal phase deficiency: What we now know Disagreement about the cause, true incidence, and diagnostic criteria of this condition makes evaluation and management difficult. Here, 2 physicians dissect the data and offer an algorithm of assessment and treatment. espite scanty and controversial sup- difficult to definitively diagnose the deficien- porting evidence, evaluation of cy or determine its incidence. Further, while Dpatients with infertility or recurrent reasonable consensus exists that endometrial pregnancy loss for possible luteal phase defi- biopsy is the most reliable diagnostic tool, ciency (LPD) is firmly established in clinical concerns remain about its timing, repetition, practice. In this article, we examine the data and interpretation. and offer our perspective on the role of LPD in assessing and managing couples with A defect of corpus luteum reproductive disorders (FIGURE 1). progesterone output? PD is defined as endometrial histology Many areas of controversy Linconsistent with the chronological date of lthough observational and retrospective the menstrual cycle, based on the woman’s Astudies have reported a higher incidence of LPD in women with infertility and recurrent KEY POINTS 1-4 pregnancy losses than in fertile controls, no ■ Luteal phase deficiency (LPD), defined as prospective study has confirmed these find- endometrial histology inconsistent with the ings. Furthermore, studies have failed to con- chronological date of the menstrual cycle, may be firm the superiority of any particular therapy. caused by deficient progesterone secretion from the corpus luteum or failure of the endometrium Once considered an important cause of to respond appropriately to ovarian steroids. -

Regulation and Roles of the Hyaluronan System in Mammalian Reproduction
REPRODUCTIONREVIEW Regulation and roles of the hyaluronan system in mammalian reproduction Ali A Fouladi-Nashta1, Kabir A Raheem1,2, Waleed F Marei1,3, Fataneh Ghafari1 and Geraldine M Hartshorne4 1Royal Veterinary College, Reproduction Research Group, Hawkshead Campus, Hatfield, UK, 2Department of Veterinary Surgery and Theriogenology, Michael Okpara University of Agriculture, Umudike, Nigeria, 3Department of Theriogenology, Faculty of Veterinary Medicine, Cairo University, Giza, Egypt and 4Warwick Medical School, University of Warwick, Coventry, UK and Centre for Reproductive Medicine, University Hospitals Coventry and Warwickshire NHS Trust, Coventry, UK Correspondence should be addressed to A A Fouladi-Nashta; Email: [email protected] Abstract Hyaluronan (HA) is a non-sulphated glycosaminoglycan polymer naturally occurring in many tissues and fluids of mammals, including the reproductive system. Its biosynthesis by HA synthase (HAS1–3) and catabolism by hyaluronidases (HYALs) are affected by ovarian steroid hormones. Depending upon its molecular size, HA functions both as a structural component of tissues in the form of high-molecular-weight HA or as a signalling molecule in the form of small HA molecules or HA fragments with effects mediated through interaction with its specific cell-membrane receptors. HA is produced by oocytes and embryos and in various segments of the reproductive system. This review provides information about the expression and function of members of the HA system, including HAS, HYALs and HA receptors. We examine their role in various processes from folliculogenesis through oocyte maturation, fertilisation and early embryo development, to pregnancy and cervical dilation, as well as its application in assisted reproduction technologies. Particular emphasis has been placed upon the role of the HA system in pre-implantation embryo development and embryo implantation, for which we propose a hypothetical sequential model. -

Normal Imaging Findings of the Uterus 3
Normal Image Findings of the Uterus 37 Normal Imaging Findings of the Uterus 3 Claudia Klüner and Bernd Hamm CONTENTS the strong muscle coat forming the mass of the organ. The myometrium is mostly comprised of spindle- 3.1 Embryonic Development and shaped smooth muscle cells and additionally con- Normal Anatomy of the Uterus 37 tains reserve connective tissue cells, which give rise 3.2 Imaging Findings: Uterine Corpus 40 to additional myometrial cells in pregnancy through 3.3 Imaging Findings: Uterine Cervix 44 hyperplasia. The uterine cavity is only a thin cleft and References 47 is lined by endometrium (Fig. 3.2). Functionally, the endometrium consists of basal and functional layers. The isthmus of uterus (lower uterine segment), 3.1 together with the internal os, forms the junction be- Embryonic Development and tween the corpus and cervix. In nonpregnant wom- Normal Anatomy of the Uterus en the isthmus is only about 5 mm high and is less muscular than the corpus. Unlike the uterine cervix, During embryonal life, fusion of the two Müllerian the isthmus becomes overproportionally large in the ducts gives rise to the uterine corpus, isthmus, cervix, course of pregnancy and serves as a kind of reserve and the upper third of the vagina. The Müllerian ducts for fetal development in addition to the uterine cor- are of mesodermal origin and arise in the 4th week pus. The endometrium of the isthmus consists of a of gestation. They course on both sides lateral to the single layer of columnar epithelium and only under- ducts of the mesonephros (Wolffi an ducts). -

Clinical Pelvic Anatomy
SECTION ONE • Fundamentals 1 Clinical pelvic anatomy Introduction 1 Anatomical points for obstetric analgesia 3 Obstetric anatomy 1 Gynaecological anatomy 5 The pelvic organs during pregnancy 1 Anatomy of the lower urinary tract 13 the necks of the femora tends to compress the pelvis Introduction from the sides, reducing the transverse diameters of this part of the pelvis (Fig. 1.1). At an intermediate level, opposite A thorough understanding of pelvic anatomy is essential for the third segment of the sacrum, the canal retains a circular clinical practice. Not only does it facilitate an understanding cross-section. With this picture in mind, the ‘average’ of the process of labour, it also allows an appreciation of diameters of the pelvis at brim, cavity, and outlet levels can the mechanisms of sexual function and reproduction, and be readily understood (Table 1.1). establishes a background to the understanding of gynae- The distortions from a circular cross-section, however, cological pathology. Congenital abnormalities are discussed are very modest. If, in circumstances of malnutrition or in Chapter 3. metabolic bone disease, the consolidation of bone is impaired, more gross distortion of the pelvic shape is liable to occur, and labour is likely to involve mechanical difficulty. Obstetric anatomy This is termed cephalopelvic disproportion. The changing cross-sectional shape of the true pelvis at different levels The bony pelvis – transverse oval at the brim and anteroposterior oval at the outlet – usually determines a fundamental feature of The girdle of bones formed by the sacrum and the two labour, i.e. that the ovoid fetal head enters the brim with its innominate bones has several important functions (Fig.