(DSD)-Related Genes in Small for Gestational Age Children with Hypospadias
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

KIAA0556 Is a Novel Ciliary Basal Body Component Mutated in Joubert Syndrome Anna A
Sanders et al. Genome Biology (2015) 16:293 DOI 10.1186/s13059-015-0858-z RESEARCH Open Access KIAA0556 is a novel ciliary basal body component mutated in Joubert syndrome Anna A. W. M. Sanders1†, Erik de Vrieze2,3†, Anas M. Alazami4†, Fatema Alzahrani4, Erik B. Malarkey5, Nasrin Sorusch6, Lars Tebbe6, Stefanie Kuhns1, Teunis J. P. van Dam7, Amal Alhashem8, Brahim Tabarki8, Qianhao Lu9,10, Nils J. Lambacher1, Julie E. Kennedy1, Rachel V. Bowie1, Lisette Hetterschijt2,3, Sylvia van Beersum3,11, Jeroen van Reeuwijk3,11, Karsten Boldt12, Hannie Kremer2,3,11, Robert A. Kesterson13, Dorota Monies4, Mohamed Abouelhoda4, Ronald Roepman3,11, Martijn H. Huynen7, Marius Ueffing12, Rob B. Russell9,10, Uwe Wolfrum6, Bradley K. Yoder5, Erwin van Wijk2,3*, Fowzan S. Alkuraya4,14* and Oliver E. Blacque1* Abstract Background: Joubert syndrome (JBTS) and related disorders are defined by cerebellar malformation (molar tooth sign), together with neurological symptoms of variable expressivity. The ciliary basis of Joubert syndrome related disorders frequently extends the phenotype to tissues such as the eye, kidney, skeleton and craniofacial structures. Results: Using autozygome and exome analyses, we identified a null mutation in KIAA0556 in a multiplex consanguineous family with hallmark features of mild Joubert syndrome. Patient-derived fibroblasts displayed reduced ciliogenesis potential and abnormally elongated cilia. Investigation of disease pathophysiology revealed that Kiaa0556-/- null mice possess a Joubert syndrome-associated brain-restricted phenotype. Functional studies in Caenorhabditis elegans nematodes and cultured human cells support a conserved ciliary role for KIAA0556 linked to microtubule regulation. First, nematode KIAA0556 is expressed almost exclusively in ciliated cells, and the worm and human KIAA0556 proteins are enriched at the ciliary base. -

An E2-Ubiquitin Thioester-Driven Approach to Identify Substrates Modified with Ubiquitin and Ubiquitin-Like Molecules
ARTICLE DOI: 10.1038/s41467-018-07251-5 OPEN An E2-ubiquitin thioester-driven approach to identify substrates modified with ubiquitin and ubiquitin-like molecules Gábor Bakos1,LuYu2, Igor A. Gak1, Theodoros I. Roumeliotis2, Dimitris Liakopoulos3, Jyoti S. Choudhary2 & Jörg Mansfeld 1 fi 1234567890():,; Covalent modi cations of proteins with ubiquitin and ubiquitin-like molecules are instru- mental to many biological processes. However, identifying the E3 ligase responsible for these modifications remains a major bottleneck in ubiquitin research. Here, we present an E2-thioester-driven identification (E2~dID) method for the targeted identification of substrates of specific E2 and E3 enzyme pairs. E2~dID exploits the central position of E2-conjugating enzymes in the ubiquitination cascade and provides in vitro generated biotinylated E2~ubiquitin thioester conjugates as the sole source for ubiquitination in extracts. This enables purification and mass spectrometry-based identification of modified proteins under stringent conditions independently of the biological source of the extract. We demonstrate the sensitivity and specificity of E2-dID by identifying and validating substrates of APC/C in human cells. Finally, we perform E2~dID with SUMO in S. cerevisiae, showing that this approach can be easily adapted to other ubiquitin-like modifiers and experimental models. 1 Cell Cycle, Biotechnology Center, Technische Universität Dresden, 01307 Dresden, Germany. 2 Functional Proteomics Group, The Institute of Cancer Research, London SW3 6JB, UK. 3 Centre -

Universidade De São Paulo Faculdade De Zootecnia E Engenharia De Alimentos
UNIVERSIDADE DE SÃO PAULO FACULDADE DE ZOOTECNIA E ENGENHARIA DE ALIMENTOS LAÍS GRIGOLETTO Genomic studies in Montana Tropical Composite cattle Pirassununga 2020 LAIS GRIGOLETTO Genomic studies in Montana Tropical Composite cattle Versão Corrigida Thesis submitted to the College of Animal Science and Food Engineering, University of São Paulo in partial fulfillment of the requirements for the degree of Doctor in Science from the Animal Biosciences program. Concentration area: Genetics, Molecular and Cellular Biology Supervisor: Prof. Dr. José Bento Sterman Ferraz Co-supervisor: Prof. Dr. Fernando Baldi Pirassununga 2020 Ficha catalográfica elaborada pelo Serviço de Biblioteca e Informação, FZEA/USP, com os dados fornecidos pelo(a) autor(a) Grigoletto, Laís G857g Genomic studies in Montana Tropical Composite cattle / Laís Grigoletto ; orientador José Bento Sterman Ferraz ; coorientador Fernando Baldi. -- Pirassununga, 2020. 183 f. Tese (Doutorado - Programa de Pós-Graduação em Biociência Animal) -- Faculdade de Zootecnia e Engenharia de Alimentos, Universidade de São Paulo. 1. beef cattle. 2. composite. 3. genomics. 4. imputation. 5. genetic progress. I. Ferraz, José Bento Sterman, orient. II. Baldi, Fernando, coorient. III. Título. Permitida a cópia total ou parcial deste documento, desde que citada a fonte - o autor UNIVERSIDADE DE SÃO PAULO Faculdade de Zootecnia e Engenharia de Alimentos Comissão de Ética no Uso de Animais DISPENSA DE ANÁLISE ÉTICA Comunicamos que o projeto de pesquisa abaixo identificado está dispensado da análise ética por utilizar animais oriundos de coleções biológicas formadas anteriormente ao ano de 2008, ano da promulgação da Lei nº 11.794/2008 – lei que estabelece procedimentos para o uso científico de animais. Ressaltamos que atividades realizadas na vigência da referida lei, ou que resulte em incremento do acervo biológico, devem ser submetidas à análise desta CEUA conforme disposto pelo Conselho Nacional de Controle de Experimentação Animal (CONCEA). -
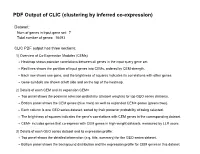
PDF Output of CLIC (Clustering by Inferred Co-Expression)
PDF Output of CLIC (clustering by inferred co-expression) Dataset: Num of genes in input gene set: 7 Total number of genes: 16493 CLIC PDF output has three sections: 1) Overview of Co-Expression Modules (CEMs) Heatmap shows pairwise correlations between all genes in the input query gene set. Red lines shows the partition of input genes into CEMs, ordered by CEM strength. Each row shows one gene, and the brightness of squares indicates its correlations with other genes. Gene symbols are shown at left side and on the top of the heatmap. 2) Details of each CEM and its expansion CEM+ Top panel shows the posterior selection probability (dataset weights) for top GEO series datasets. Bottom panel shows the CEM genes (blue rows) as well as expanded CEM+ genes (green rows). Each column is one GEO series dataset, sorted by their posterior probability of being selected. The brightness of squares indicates the gene's correlations with CEM genes in the corresponding dataset. CEM+ includes genes that co-express with CEM genes in high-weight datasets, measured by LLR score. 3) Details of each GEO series dataset and its expression profile: Top panel shows the detailed information (e.g. title, summary) for the GEO series dataset. Bottom panel shows the background distribution and the expression profile for CEM genes in this dataset. Overview of Co-Expression Modules (CEMs) with Dataset Weighting Scale of average Pearson correlations Num of Genes in Query Geneset: 7. Num of CEMs: 1. 0.0 0.2 0.4 0.6 0.8 1.0 Med14 Med21 Med6 Cdk8 Ccnc Med10 Med23 Med14 Med21 -

Agricultural University of Athens
ΓΕΩΠΟΝΙΚΟ ΠΑΝΕΠΙΣΤΗΜΙΟ ΑΘΗΝΩΝ ΣΧΟΛΗ ΕΠΙΣΤΗΜΩΝ ΤΩΝ ΖΩΩΝ ΤΜΗΜΑ ΕΠΙΣΤΗΜΗΣ ΖΩΙΚΗΣ ΠΑΡΑΓΩΓΗΣ ΕΡΓΑΣΤΗΡΙΟ ΓΕΝΙΚΗΣ ΚΑΙ ΕΙΔΙΚΗΣ ΖΩΟΤΕΧΝΙΑΣ ΔΙΔΑΚΤΟΡΙΚΗ ΔΙΑΤΡΙΒΗ Εντοπισμός γονιδιωματικών περιοχών και δικτύων γονιδίων που επηρεάζουν παραγωγικές και αναπαραγωγικές ιδιότητες σε πληθυσμούς κρεοπαραγωγικών ορνιθίων ΕΙΡΗΝΗ Κ. ΤΑΡΣΑΝΗ ΕΠΙΒΛΕΠΩΝ ΚΑΘΗΓΗΤΗΣ: ΑΝΤΩΝΙΟΣ ΚΟΜΙΝΑΚΗΣ ΑΘΗΝΑ 2020 ΔΙΔΑΚΤΟΡΙΚΗ ΔΙΑΤΡΙΒΗ Εντοπισμός γονιδιωματικών περιοχών και δικτύων γονιδίων που επηρεάζουν παραγωγικές και αναπαραγωγικές ιδιότητες σε πληθυσμούς κρεοπαραγωγικών ορνιθίων Genome-wide association analysis and gene network analysis for (re)production traits in commercial broilers ΕΙΡΗΝΗ Κ. ΤΑΡΣΑΝΗ ΕΠΙΒΛΕΠΩΝ ΚΑΘΗΓΗΤΗΣ: ΑΝΤΩΝΙΟΣ ΚΟΜΙΝΑΚΗΣ Τριμελής Επιτροπή: Aντώνιος Κομινάκης (Αν. Καθ. ΓΠΑ) Ανδρέας Κράνης (Eρευν. B, Παν. Εδιμβούργου) Αριάδνη Χάγερ (Επ. Καθ. ΓΠΑ) Επταμελής εξεταστική επιτροπή: Aντώνιος Κομινάκης (Αν. Καθ. ΓΠΑ) Ανδρέας Κράνης (Eρευν. B, Παν. Εδιμβούργου) Αριάδνη Χάγερ (Επ. Καθ. ΓΠΑ) Πηνελόπη Μπεμπέλη (Καθ. ΓΠΑ) Δημήτριος Βλαχάκης (Επ. Καθ. ΓΠΑ) Ευάγγελος Ζωίδης (Επ.Καθ. ΓΠΑ) Γεώργιος Θεοδώρου (Επ.Καθ. ΓΠΑ) 2 Εντοπισμός γονιδιωματικών περιοχών και δικτύων γονιδίων που επηρεάζουν παραγωγικές και αναπαραγωγικές ιδιότητες σε πληθυσμούς κρεοπαραγωγικών ορνιθίων Περίληψη Σκοπός της παρούσας διδακτορικής διατριβής ήταν ο εντοπισμός γενετικών δεικτών και υποψηφίων γονιδίων που εμπλέκονται στο γενετικό έλεγχο δύο τυπικών πολυγονιδιακών ιδιοτήτων σε κρεοπαραγωγικά ορνίθια. Μία ιδιότητα σχετίζεται με την ανάπτυξη (σωματικό βάρος στις 35 ημέρες, ΣΒ) και η άλλη με την αναπαραγωγική -

Downloaded from Ensembl
UCSF UC San Francisco Electronic Theses and Dissertations Title Detecting genetic similarity between complex human traits by exploring their common molecular mechanism Permalink https://escholarship.org/uc/item/1k40s443 Author Gu, Jialiang Publication Date 2019 Peer reviewed|Thesis/dissertation eScholarship.org Powered by the California Digital Library University of California by Submitted in partial satisfaction of the requirements for degree of in in the GRADUATE DIVISION of the UNIVERSITY OF CALIFORNIA, SAN FRANCISCO AND UNIVERSITY OF CALIFORNIA, BERKELEY Approved: ______________________________________________________________________________ Chair ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________________________________ Committee Members ii Acknowledgement This project would not have been possible without Prof. Dr. Hao Li, Dr. Jiashun Zheng and Dr. Chris Fuller at the University of California, San Francisco (UCSF) and Caribou Bioscience. The Li lab grew into a multi-facet research group consist of both experimentalists and computational biologists covering three research areas including cellular/molecular mechanism of ageing, genetic determinants of complex human traits and structure, function, evolution of gene regulatory network. Labs like these are the pillar of global success and reputation -

A Sensitized Mutagenesis Screen in Factor V Leiden Mice Identifies Novel Thrombosis
bioRxiv preprint doi: https://doi.org/10.1101/080432; this version posted April 6, 2017. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. A sensitized mutagenesis screen in Factor V Leiden mice identifies novel thrombosis suppressor loci Randal J. Westricka,b,c,i, Kärt Tombergc,e,i, Amy E. Sieberta,i, Guojing Zhuc, Mary E. Winnd, Sarah L. Dobiesc, Sara L. Manningc, Marisa A. Brakea, Audrey C. Cleurenc, Linzi M. Hobbsa, Lena M. Mishacka, Alexander Johnstona, Emilee Kotnikc, David R. Siemieniakf, Jishu Xue, Jun Z. Lie, Thomas L. Saundersg and David Ginsburgc,e,f,h aOakland University Department of Biological Sciences bOakland University Center for Data Science and Big Data Analysis cLife Sciences Institute, University of Michigan dBioinformatics and Biostatistics Core, Van Andel Research Institute eDepartment of Human Genetics, University of Michigan fHoward Hughes Medical Institute, University of Michigan gTransgenic Animal Model Core, University of Michigan hDepartments of Internal Medicine and Pediatrics, University of Michigan iThese authors contributed equally to this work Corresponding author: David Ginsburg, MD. 5214 LSI Building, 210 Washtenaw Avenue, Ann Arbor MI 48109. E- mail: [email protected], Telephone: 734-647-4808, Fax: 734-936-2888. [48 pages, 227 words in abstract, 5,340 words, 30,327 characters not including abstract, title page, figures and references] 1 bioRxiv preprint doi: https://doi.org/10.1101/080432; this version posted April 6, 2017. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. -

A Meta-Analysis of the Effects of High-LET Ionizing Radiations in Human Gene Expression
Supplementary Materials A Meta-Analysis of the Effects of High-LET Ionizing Radiations in Human Gene Expression Table S1. Statistically significant DEGs (Adj. p-value < 0.01) derived from meta-analysis for samples irradiated with high doses of HZE particles, collected 6-24 h post-IR not common with any other meta- analysis group. This meta-analysis group consists of 3 DEG lists obtained from DGEA, using a total of 11 control and 11 irradiated samples [Data Series: E-MTAB-5761 and E-MTAB-5754]. Ensembl ID Gene Symbol Gene Description Up-Regulated Genes ↑ (2425) ENSG00000000938 FGR FGR proto-oncogene, Src family tyrosine kinase ENSG00000001036 FUCA2 alpha-L-fucosidase 2 ENSG00000001084 GCLC glutamate-cysteine ligase catalytic subunit ENSG00000001631 KRIT1 KRIT1 ankyrin repeat containing ENSG00000002079 MYH16 myosin heavy chain 16 pseudogene ENSG00000002587 HS3ST1 heparan sulfate-glucosamine 3-sulfotransferase 1 ENSG00000003056 M6PR mannose-6-phosphate receptor, cation dependent ENSG00000004059 ARF5 ADP ribosylation factor 5 ENSG00000004777 ARHGAP33 Rho GTPase activating protein 33 ENSG00000004799 PDK4 pyruvate dehydrogenase kinase 4 ENSG00000004848 ARX aristaless related homeobox ENSG00000005022 SLC25A5 solute carrier family 25 member 5 ENSG00000005108 THSD7A thrombospondin type 1 domain containing 7A ENSG00000005194 CIAPIN1 cytokine induced apoptosis inhibitor 1 ENSG00000005381 MPO myeloperoxidase ENSG00000005486 RHBDD2 rhomboid domain containing 2 ENSG00000005884 ITGA3 integrin subunit alpha 3 ENSG00000006016 CRLF1 cytokine receptor like -

Unveiling Comparative Genomic Trajectories of Selection and Key Candidate Genes in Egg-Type Russian White and Meat-Type White Cornish Chickens
biology Article Unveiling Comparative Genomic Trajectories of Selection and Key Candidate Genes in Egg-Type Russian White and Meat-Type White Cornish Chickens Alexandra S. Abdelmanova 1, Arsen V. Dotsev 1 , Michael N. Romanov 2,3,* , Olga I. Stanishevskaya 4, Elena A. Gladyr 1 , Andrey N. Rodionov 1, Anastasia N. Vetokh 1 , Natalia A. Volkova 1 , Elena S. Fedorova 4, Igor V. Gusev 1, Darren K. Griffin 2 , Gottfried Brem 5 and Natalia A. Zinovieva 1,* 1 L.K. Ernst Federal Research Center for Animal Husbandry, 142132 Podolsk, Russia; [email protected] (A.S.A.); [email protected] (A.V.D.); [email protected] (E.A.G.); [email protected] (A.N.R.); [email protected] (A.N.V.); [email protected] (N.A.V.); [email protected] (I.V.G.) 2 School of Biosciences, University of Kent, Canterbury, Kent CT2 7NJ, UK; D.K.Griffi[email protected] 3 K.I. Skryabin Moscow State Academy of Veterinary Medicine and Biotechnology, 23 Akademika Skryabina St., 109472 Moscow, Russia 4 Russian Research Institute of Farm Animal Genetics and Breeding—Branch of the L.K. Ernst Federal Research Center for Animal Husbandry, Pushkin, 196601 St. Petersburg, Russia; [email protected] (O.I.S.); [email protected] (E.S.F.) 5 Institute of Animal Breeding and Genetics, University of Veterinary Medicine, 1210 Vienna, Austria; [email protected] * Correspondence: [email protected] (M.N.R.); [email protected] (N.A.Z.); Tel.: +798-57154351 (M.N.R.); +749-67651163 (N.A.Z.) Citation: Abdelmanova, A.S.; Dotsev, A.V.; Romanov, M.N.; Stanishevskaya, Simple Summary: The search for genomic regions of putative selective signaling is instrumental in O.I.; Gladyr, E.A.; Rodionov, A.N.; obtaining information about selection history in various species and populations. -

Identification of Thrombosis Modifier Genes Using ENU Mutagenesis in the Mouse
Identification of Thrombosis Modifier Genes Using ENU Mutagenesis in the Mouse by Kärt Tomberg A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Human Genetics) in the University of Michigan 2016 Doctoral Committee: Professor David Ginsburg, Chair Associate Professor Patrick J. Hu Associate Professor Catherine E. H. Keegan Associate Professor Jun Li Assistant Professor Ryan E. Mills © Kärt Tomberg 2016 ACKNOWLEDGEMENTS First and foremost, I would like to thank my thesis mentor David Ginsburg. David has always been there for me throughout this process, either by challenging or encour- aging me, pushing or holding me back, all in good proportion. He sets a great example as a scientist, a mentor, and a human being, which I will strive to follow. Thank you to my dissertation committee (Patrick Hu, Katy Keegan, Jun Li, and Ryan Mills) for your time, great suggestions, intellectual input, encouraging support, and many helpful discussions. I would especially like to thank Ryan for letting me barge into his office, on several occasions, for advice ranging from data analysis to networking. I always left with new ideas! A special thank you to all the members of the Ginsburg lab. Each and every one of you has helped me at some point along the way. You are such great colleagues, good friends, and have provided me with a kind home away from home. I hope distance and time will not stop us from collaborating and supporting each other. A special shout-out to the amazing undergraduates that trained with me over the years. -
Generation of CRISPR Engineered Prostate Cancer Cell Line Models to Study Androgen Receptor Signalling in Advanced Prostate Cancer
Generation of CRISPR engineered prostate cancer cell line models to study androgen receptor signalling in advanced prostate cancer Thesis submitted in partial fulfilment of the requirement of the degree of Doctor of Philosophy Evangelia Eirini Kounatidou Northern Institute for Cancer Research Faculty of Medical Sciences Newcastle University September 2019 Abstract Prostate cancer resistance to AR targeted therapies due to the emergence of AR point mutations and AR splice variants that cannot be targeted by the currently available agents comprise a major clinical challenge. There is paucity of models that accurately reflect the mechanisms of AR regulation in advanced disease. This highlights the high demand of generating novel disease relevant models. A CRISPR pipeline was developed to generate cell line models which harbour specific point mutations in the LBD of AR as well as stop codons in AR exon 5 which resulted in AR-FL knock-out so that the remaining endogenous AR-Vs could be studied discriminately of interfering AR-FL. Using a streptavidin-tagged Cas9 in conjugation with a biotinylated donor template resulted in high donor template knock-in efficiencies and yielded (i) an ARW741L CWR22Rv1 cell line derivative and (ii) an AR-FL knock-out cell line derivative called CWR22Rv1-AR-EK (Exon Knock-out). CWR22Rv1-AR-EK cells retained all endogenous AR-Vs following AR gene editing. AR-Vs acted unhindered following AR-FL deletion to drive cell growth and expression of androgenic genes. Global transcriptomics demonstrated that AR-Vs drive expression of a cohort of cell cycle and DNA damage response genes and depletion of AR-Vs sensitised cells to ionising radiation. -

Genomic Analysis of Human Spinal Deformity and Characterization of a Zebrafish Disease Model Jillian Gwen Buchan Washington University in St
Washington University in St. Louis Washington University Open Scholarship All Theses and Dissertations (ETDs) Spring 4-22-2014 Genomic Analysis of Human Spinal Deformity and Characterization of a Zebrafish Disease Model Jillian Gwen Buchan Washington University in St. Louis Follow this and additional works at: https://openscholarship.wustl.edu/etd Recommended Citation Buchan, Jillian Gwen, "Genomic Analysis of Human Spinal Deformity and Characterization of a Zebrafish Disease Model" (2014). All Theses and Dissertations (ETDs). 1223. https://openscholarship.wustl.edu/etd/1223 This Dissertation is brought to you for free and open access by Washington University Open Scholarship. It has been accepted for inclusion in All Theses and Dissertations (ETDs) by an authorized administrator of Washington University Open Scholarship. For more information, please contact [email protected]. WASHINGTON UNIVERSITY IN ST. LOUIS Division of Biology & Biomedical Sciences Molecular Genetics and Genomics Dissertation Examination Committee: Christina A. Gurnett, Chair Carlos Cruchaga Alison M. Goate Matthew I. Goldsmith Kelly R. Monk Lilianna Solnica-Krezel Genomic Analysis of Human Spinal Deformity and Characterization of a Zebrafish Disease Model by Jillian Gwen Buchan A dissertation presented to the Graduate School of Arts and Sciences of Washington University in partial fulfillment of the requirements for the degree of Doctor of Philosophy May 2014 St. Louis, Missouri TABLE OF CONTENTS List of Figures ….………………………………………………………………………… iv List of Tables