Original Article the Selective C-Met Inhibitor Tepotinib Can Overcome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Treatment and Testing Guidelines
For patients with METex14 and BRAF V600E in mNSCLC, TREATMENT AND TESTING GUIDELINES METex14 BRAF V600E BRAF, v-raf murine sarcoma viral oncogene homolog B1; MET, mesenchymal-epithelial transition; METex14, MET exon 14 skipping; mNSCLC, metastatic non-small cell lung cancer. Indication Indication TABRECTA® (capmatinib) tablets is indicated for the TAFINLAR® (dabrafenib) capsules, in combination with treatment of adult patients with metastatic non-small MEKINIST® (trametinib) tablets, is indicated for the cell lung cancer (NSCLC) whose tumors have a mutation treatment of patients with metastatic non-small cell that leads to mesenchymal-epithelial transition (MET) lung cancer (NSCLC) with BRAF V600E mutation as exon 14 skipping as detected by an FDA-approved test. detected by an FDA-approved test. This indication is approved under accelerated approval Limitation of Use: TAFINLAR is not indicated for the based on overall response rate and duration of treatment of patients with wild-type BRAF NSCLC. response. Continued approval for this indication may be contingent upon verification and description of clinical Important Safety Information benefit in confirmatory trials. New Primary Malignancies. Important Safety Information Cutaneous Malignancies Interstitial Lung Disease (ILD)/Pneumonitis. Across clinical trials of TAFINLAR administered with ILD/pneumonitis, which can be fatal, occurred in MEKINIST (“the combination”), the incidence patients treated with TABRECTA. ILD/pneumonitis of cutaneous squamous cell carcinomas (cuSCCs), occurred in 4.5% of patients treated with TABRECTA including keratoacanthomas, occurred in 2% of in the GEOMETRY mono-1 study, with 1.8% of patients patients. Basal cell carcinoma and new primary experiencing grade 3 ILD/pneumonitis and 1 patient melanoma occurred in 3% and <1% of patients, experiencing death (0.3%). -

Resistance Mechanisms to Osimertinib in EGFR-Mutated Non-Small Cell Lung Cancer
www.nature.com/bjc REVIEW ARTICLE Resistance mechanisms to osimertinib in EGFR-mutated non-small cell lung cancer Alessandro Leonetti1,2, Sugandhi Sharma2, Roberta Minari1, Paola Perego3, Elisa Giovannetti2,4 and Marcello Tiseo 1,5 Osimertinib is an irreversible, third-generation epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor that is highly selective for EGFR-activating mutations as well as the EGFR T790M mutation in patients with advanced non-small cell lung cancer (NSCLC) with EGFR oncogene addiction. Despite the documented efficacy of osimertinib in first- and second-line settings, patients inevitably develop resistance, with no further clear-cut therapeutic options to date other than chemotherapy and locally ablative therapy for selected individuals. On account of the high degree of tumour heterogeneity and adaptive cellular signalling pathways in NSCLC, the acquired osimertinib resistance is highly heterogeneous, encompassing EGFR-dependent as well as EGFR- independent mechanisms. Furthermore, data from repeat plasma genotyping analyses have highlighted differences in the frequency and preponderance of resistance mechanisms when osimertinib is administered in a front-line versus second-line setting, underlying the discrepancies in selection pressure and clonal evolution. This review summarises the molecular mechanisms of resistance to osimertinib in patients with advanced EGFR-mutated NSCLC, including MET/HER2 amplification, activation of the RAS–mitogen-activated protein kinase (MAPK) or RAS–phosphatidylinositol -
Crusader Q2 2020 Research Edition Download
Your resource for the latest research into the MET alteration. CRUSADER NEWSLETTER Q2 2020 RESEARCH EDITION MET Crusaders is a community of Lung Cancer patients and care givers collaborating with advocates and medical professionals collectively dedicated to helping patients with a MET alteration live normal lives. Come Join Us! [email protected] In this edition Top-level MET gene copy number gain defines .................... 2 Molecular Mechanisms of Acquired Resistance ................... 5 a subtype of poorly differentiated pulmonary to MET Tyrosine Kinase Inhibitors in Patients adenocarcinomas with poor prognosis with MET Exon 14-Mutant NSCLC EDITOR Characteristics and Clinical Outcomes of ............................. 2 MET Alterations Are a Recurring and Actionable .................. 6 Jessica McKernan, PharmD Non-Small Cell Lung Cancer Patients in Korea Resistance Mechanism in ALK-Positive Lung Cancer with MET Exon 14 Skipping Atrium Health Tepotinib in Non-Small-Cell Lung Cancer with ...................... 6 Charlotte, NC Clinical and molecular correlates of PD-L1 ........................... 2 MET Exon 14 Skipping Mutations (VISION Trial) expression in patients with lung adenocarcinomas Therapeutic Efficacy of ABN401, a Highly ............................. 7 CONTRIBUTING EDITORS Efficacy and Safety of Anti-PD-1 Immunotherapy ................. 3 Potent and Selective MET Inhibitor, Based on Julia Stevens, PharmD in Patients With Advanced NSCLC With BRAF, HER2, Diagnostic Biomarker Test in MET-Addicted Cancer or MET Mutations or RET Translocation: GFPC 01-2018 Beth Israel Deaconess Erlotinib plus tivantinib versus erlotinib alone ..................... 7 Medical Center Alterations in the PI3K Pathway Drive Resistance ................ 3 in patients with previously treated stage IIIb/IV Boston, MA to MET Inhibitors in NSCLC Harboring MET non-small-cell lung cancer: A meta-analysis based Exon 14 Skipping Mutations on randomized controlled trials Laura Schmidt, PharmD Incidence and PD-L1 Expression of MET 14 ......................... -

Tepotinib) Tablets, for Oral Use Any Severity
HIGHLIGHTS OF PRESCRIBING INFORMATION ------------------------WARNINGS AND PRECAUTIONS----------------------- These highlights do not include all the information needed to use TEPMETKO safely and effectively. See full prescribing information for • Interstitial Lung Disease (ILD)/Pneumonitis: Immediately withhold TEPMETKO. TEPMETKO in patients with suspected ILD/pneumonitis. Permanently discontinue TEPMETKO in patients diagnosed with ILD/pneumonitis of TEPMETKO® (tepotinib) tablets, for oral use any severity. (2.3, 5.1) Initial U.S. Approval: 2021 • Hepatotoxicity: Monitor liver function tests. Withhold, dose reduce, or permanently discontinue TEPMETKO based on severity. (5.2) ----------------------------INDICATIONS AND USAGE--------------------------- • Embryo-fetal toxicity: TEPMETKO can cause fetal harm. Advise of potential risk to a fetus and use of effective contraception. (5.3, 8.1, 8.3) TEPMETKO is a kinase inhibitor indicated for the treatment of adult patients with metastatic non-small cell lung cancer (NSCLC) harboring mesenchymal- -------------------------------ADVERSE REACTIONS------------------------------ epithelial transition (MET) exon 14 skipping alterations. (1) Most common adverse reactions (≥ 20%) were edema, fatigue, nausea, This indication is approved under accelerated approval based on overall diarrhea, musculoskeletal pain, and dyspnea. The most common Grade 3 to 4 response rate and duration of response. Continued approval for this indication laboratory abnormalities (≥ 2%) were decreased lymphocytes, decreased may be contingent upon verification and description of clinical benefit in albumin, decreased sodium, increased gamma-glutamyltransferase, increased confirmatory trials. (1) amylase, increased ALT, increased AST, and decreased hemoglobin. (6.1) -----------------------DOSAGE AND ADMINISTRATION----------------------- To report SUSPECTED ADVERSE REACTIONS, contact EMD Serono at 1-800-283-8088 ext. 5563 or FDA at 1-800-FDA-1088 or • Select patients for treatment with TEPMETKO on the presence of METex14 www.fda.gov/medwatch. -

First-Line Treatment Options for Patients with Stage IV Non-Small Cell Lung Cancer with Driver Alterations
First-Line Treatment Options for Patients with Stage IV Non-Small Cell Lung Cancer with Driver Alterations Patients with stage IV non-small cell lung cancer Nonsquamous cell carcinoma and squamous cell carcinoma Activating EGFR mutation other Sensitizing (L858R/exon 19 MET exon 14 skipping than exon 20 insertion mutations, EGFR exon 20 mutation ALK rearrangement ROS1 rearrangement BRAF V600E mutation RET rearrangement NTRK rearrangement mutations KRAS alterations HER2 alterations NRG1 alterations deletion) EGFR mutation T790M, L858R or Ex19Del PS 0-2 Treatment Options PS 0-2 Treatment Options PS 0-2 Treatment Options PS 0-2 Treatment Options PS 0-2 Treatment Options Treatment Options PS 0-2 Treatment Options PS 0-2 Treatment Options PS 0-2 Treatment Options Emerging target; no Emerging target; no Emerging target; no Platinum doublet † † † Osimertinib monotherapy S Afatinib monotherapy M M Alectinib S Entrectinib M Dabrafenib/trametinib M Capmatinib M Selpercatinib M Entrectinib M conclusions available conclusions available conclusions available chemotherapy ± bevacizumab Gefitinib with doublet Standard treatment based on Standard treatment based on Standard treatment based on M M M Brigatinib S Crizotinib M M Tepotinib M Pralsetinib* W Larotrectinib M chemotherapy non-driver mutation guideline non-driver mutation guideline non-driver mutation guideline If alectinib or brigatinib are not available If entrectinib or crizotinib are not available Standard treatment based on Standard treatment based on Standard treatment based on Dacomitinib monotherapy M Osimertinib W M M M Ceritinib S Ceritinib W non-driver mutation guideline non-driver mutation guideline non-driver mutation guideline Monotherapy with afatinib M Crizotinib S Lortlatinib W Standard treatment based on Erlotinib/ramucirumab M M non-driver mutation guideline Erlotinib/bevacizumab M Monotherapy with erlotinib M Strength of Recommendation Monotherapy with gefitinib M S Strong M Moderate W Weak Monotherapy with icotinib M Notes. -

Issue 18, July 2020 Newsletter
Issue 18: July 2020 (Covering Dec 2019-Apr 2020 news) Special Update: COVID-19 and IBC Research Program and Clinic Operations The COVID-19 pandemic has had significant effects on the operations of our program and clinic. Starting in mid-March 2020, research and administrative staff began working 100% remotely to limit the on-site footprint and ensure the wellbeing of employees and patients. Physicians came to the hospital for their clinics and inpatient rotations, but otherwise worked remotely on their normal responsibilities in patient-care, research and administration. Meetings were all switched to Zoom, and we all learned how to function as remote teams. Clinical research required substantial changes to normal practices. Patients already enrolled on clinical trials continued to see physicians and receive treatment, however, new enrollments to our entire research portfolio were halted for 2+ months. Some patients had to receive infusions locally rather than traveling ot MD Anderson. Gradually, as the institutional restrictions opened up, as of July 2, we have now begun screening and enrolling new patients on all active IBC clinical trials, mindful of the need to push forward with providing the best treatment choices for patients diagnosed with this aggressive subtype of breast cancer. Throughout the pandemic, new IBC patients were seen in the IBC Multi-Team clinic on Wednesdays, and local new patients were also seen by the medical oncologists if they did not fit the multi-team criteria. Second-opinion (previously treated) patients from out of state were unable to be seen during the early part of the pandemic, but as of now, these patients are being accommodated due to the Breast Center being approved as a strategic service line for the institution. -

Entrectinib in Patients with Advanced Or Metastatic NTRK Fusion-Positive
■ INFLUENTIAL PAPERS Lancet Oncol. 2020 Feb;21(2):271-282. Entrectinib in patients with advanced or metastatic NTRK fusion-positive solid tumours: integrated analysis of three phase 1-2 trials Robert C Doebele, Alexander Drilon, Luis Paz-Ares, Salvatore Siena, Alice T Shaw, Anna F Farago, Collin M Blakely, Takashi Seto, Byung Chul Cho, Diego Tosi, Benjamin Besse, Sant P Chawla, Lyudmila Bazhenova, John C Krauss, Young Kwang Chae, MinalBarve, Ignacio Garrido-Laguna, Stephen V Liu, Paul Conkling, Thomas John, Marwan Fakih, Darren Sigal, Herbert H Loong, Gary L Buchschacher Jr, Pilar Garrido, Jorge Nieva, Conor Steuer, Tobias R Overbeck, Daniel W Bowles, Elizabeth Fox, Todd Riehl, Edna Chow-Maneval, Brian Simmons, Na Cui, Ann Johnson, Susan Eng, Timothy R Wilson, George D Demetri, trial investigators BACKGROUND: Entrectinib is a potent inhibitor of tropomyosin receptor kinase (TRK) A, B, and C, which has been shown to have anti-tumour activity against NTRK gene fusion-positive solid tumours, including CNS activity due to its ability to penetrate the blood-brain barrier. We present an integrated efficacy and safety analysis of patients with metastatic or locally advanced solid tumours harbouring oncogenic NTRK1, NTRK2, and NTRK3 gene fusions treated in three ongoing, early-phase trials. METHODS: An integrated database comprised the pivotal datasets of three, ongoing phase 1 or 2 clinical trials (ALKA-372-001, STARTRK-1, and STARTRK-2), which enrolled patients aged 18 years or older with metastatic or locally advanced NTRK fusion-positive solid tumours who received entrectinib orally at a dose of at least 600 mg once per day in a capsule. -
Presentación De Powerpoint
Molecular Tumor Board in Non-Small Cell Lung Cancer Jordi Remon Masip CIOCC Barcelona – HM Delfos @JordiRemon #SEOM20 Disclosure Information I do not have COI related to this specific presentation Why do we need a MTB in NSCLC? • Introduction • To understand the genomic profile from NGS reports • To prioritize the druggable genomic alteration: baseline / resistant • Increasing the detection of potential druggable genomic alterations • To include patients in basket trials • NGS is a reality but MTB and precision approach have challenges MTB is included in one equation MOLECULAR TUMOR BOARD Y MTB is included in one equation GENOMIC MOLECULAR TUMOR PROFILE BOARD X + Y MTB is included in one equation GENOMIC MOLECULAR TUMOR PERSONALISED PROFILE BOARD TREATMENT X + Y = Z Precision oncology in practice EGFR TKI Find actionable gens with ALK/ROS1 TKI approved therapy BRAF TKI Find actionable genes for RET / NTRK TKI clinical trials MET TKI Precision oncology in practice EGFR TKI Find actionable gens with ALK/ROS1 TKI approved therapy BRAF TKI Find actionable genes for RET / NTRK TKI clinical trials MET TKI Additional information about non-actionable gene mutations prognostic markers of sensitivity Two major steps in NSCLC outcome Immunotherapy Personalised treatment, ALK+: 5-y OS, KEYNOTE 024 Trial 5-y OS, ALEX trial Median OS, HR, (95%CI) 5-Year OS Rate, Median OS, HR, (95%CI) 5-Year OS Rate, mo % mo % 26.3 0.62 31.9 Not reached 0.67 63 13.4 (0.48-0.81) 16.7 57.4 (0.46-0.98) 46 Alectinib 26.4% Crizotinib Pembrolizumab Chemotherapy Brahmer – ESMO 2020 Mok – Annls of Oncology 2020 Number of oncogenes increases over time NTRK rearrangement Figure from Garrido – CTO 2019 (modified based on updated ESMO guidelines 2020 by Planchard et al.) Number of oncogenes increases over time NRG1 KRAS RET MET HER2 UN NTRK rearrangement Coming Future…. -

(FDA) Approved Bristol Myers Squibb's (Bms.Com) Br
tools Approved Drugs (cemiplimab-rwlc) for patients with • On Dec. 18, 2020, the FDA approved locally advanced basal cell carcinoma Tagrisso® (osimertinib) (AstraZeneca, • On Feb. 5, 2021, the U.S. Food and Drug previously treated with a hedgehog astrazeneca.com) for adjuvant therapy Administration (FDA) approved Bristol pathway inhibitor (HHI) or for whom an after tumor resection in patients with ® Myers Squibb’s (bms.com) Breyanzi HHI is not appropriate and accelerated non-small cell lung cancer (NSCLC) whose (lisocabtagene maraleucel), a CD19- approval to Libtayo for patients with tumors have epidermal growth factor directed chimeric antigen receptor T-cell metastatic basal cell carcinoma previ- receptor exon 19 deletions or exon 21 therapy for the treatment of adult ously treated with an HHI or for whom an L858R mutations, as detected by an patients with relapsed or refractory large HHI is not appropriate. FDA-approved test. B-cell lymphoma after two or more lines • On Dec. 16, 2020, the FDA approved On Feb. 3, 2021, the FDA granted of systemic therapy, including diffuse ™ • Margenza (margetuximab-cmkb) ® large B-cell lymphoma not otherwise accelerated approval to Tepmetko (MacroGenics, macrogenics.com) in specified (including diffuse large B-cell (tepotinib) (EMD Serono, combination with chemotherapy for the lymphoma arising from indolent emdserono.com/us-en) for adult patients treatment of adult patients with with metastatic NSCLC harboring lymphoma), high-grade B-cell lymphoma, metastatic HER2-positive breast cancer primary mediastinal large B-cell mesenchymal-epithelial transition exon who have received two or more prior 14 skipping alterations. lymphoma, and follicular lymphoma anti-HER2 regimens, at least one of which grade 3B. -
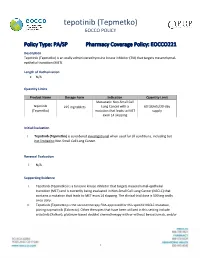
Tepotinib (Tepmetko) EOCCO POLICY
tepotinib (Tepmetko) EOCCO POLICY Policy Type: PA/SP Pharmacy Coverage Policy: EOCCO221 Description Tepotinib (Tepmetko) is an orally administered tyrosine kinase inhibitor (TKI) that targets mesenchymal- epithelial transition (MET). Length of Authorization N/A Quantity Limits Product Name Dosage Form Indication Quantity Limit Metastatic Non -Small Cell tepotinib 225 mg tablets Lung Cancer with a 60 tablets/30-day (Tepmetko) mutation that leads to MET supply exon 14 skipping Initial Evaluation I. Tepotinib (Tepmetko) is considered investigational when used for all conditions, including but not limited to Non-Small Cell Lung Cancer. Renewal Evaluation I. N/A Supporting Evidence I. Tepotinib (Tepmetko) is a tyrosine kinase inhibitor that targets mesenchymal-epithelial transition (MET) and is currently being evaluated in Non-Small Cell Lung Cancer (NSCLC) that contains a mutation that leads to MET exon 14 skipping. The clinical trial dose is 500 mg orally once daily. II. Tepotinib (Tepmetko) is the second therapy FDA-approved for this specific NSCLC mutation, joining capmatinib (Tabrecta). Other therapies that have been utilized in this setting include crizotinib (Xalkori), platinum-based doublet chemotherapy with or without bevacizumab, and/or 1 tepotinib (Tepmetko) EOCCO POLICY immunotherapy (e.g., pembrolizumab); however, available data to support efficacy in this population is limited, and response to therapy is generally poor. III. Place in therapy is likely to be in the advanced or metastatic setting based on the population being evaluated in the clinical trial, and may be utilized as first-line in these stages; however, given the limited safety and efficacy data to support its use, other therapies may be considered prior to tepotinib (Tepmetko). -
Tyrosine Kinase Inhibitors for Solid Tumors in the Past 20 Years (2001–2020) Liling Huang†, Shiyu Jiang† and Yuankai Shi*
Huang et al. J Hematol Oncol (2020) 13:143 https://doi.org/10.1186/s13045-020-00977-0 REVIEW Open Access Tyrosine kinase inhibitors for solid tumors in the past 20 years (2001–2020) Liling Huang†, Shiyu Jiang† and Yuankai Shi* Abstract Tyrosine kinases are implicated in tumorigenesis and progression, and have emerged as major targets for drug discovery. Tyrosine kinase inhibitors (TKIs) inhibit corresponding kinases from phosphorylating tyrosine residues of their substrates and then block the activation of downstream signaling pathways. Over the past 20 years, multiple robust and well-tolerated TKIs with single or multiple targets including EGFR, ALK, ROS1, HER2, NTRK, VEGFR, RET, MET, MEK, FGFR, PDGFR, and KIT have been developed, contributing to the realization of precision cancer medicine based on individual patient’s genetic alteration features. TKIs have dramatically improved patients’ survival and quality of life, and shifted treatment paradigm of various solid tumors. In this article, we summarized the developing history of TKIs for treatment of solid tumors, aiming to provide up-to-date evidence for clinical decision-making and insight for future studies. Keywords: Tyrosine kinase inhibitors, Solid tumors, Targeted therapy Introduction activation of tyrosine kinases due to mutations, translo- According to GLOBOCAN 2018, an estimated 18.1 cations, or amplifcations is implicated in tumorigenesis, million new cancer cases and 9.6 million cancer deaths progression, invasion, and metastasis of malignancies. occurred in 2018 worldwide [1]. Targeted agents are In addition, wild-type tyrosine kinases can also func- superior to traditional chemotherapeutic ones in selec- tion as critical nodes for pathway activation in cancer. -

BRAF, MET, and Her2 Mutations in Lung Cancer
BRAF, MET, and Her2 mutations in lung cancer David Planchard, MD, PhD Head of Thoracic Unit Department of Cancer Medicine Gustave Roussy – Villejuif, France DISCLOSURE SLIDE Consulting, advisory role or lectures: AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Celgene, Daiichi Sankyo, Eli Lilly, Merck, Novartis, Pfizer, prIME Oncology, Peer CME, Roche Honoraria: AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Celgene, Eli Lilly, Merck, Novartis, Pfizer, prIME Oncology, Peer CME, Roche Clinical trials research as principal or co-investigator (Institutional financial interests): AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Eli Lilly, Merck, Novartis, Pfizer, Roche, Medimmun, Sanofi-Aventis, Taiho Pharma, Novocure, Daiichi Sankyo Travel, Accommodations, Expenses: AstraZeneca, Roche, Novartis, prIME Oncology, Pfizer Great advances have been made in lung cancer therapy: targeting of oncogenic drivers EGFR sensitizing Gefitinib; Erlotinib; Afatinib; Osimertinib; Dacomitinib ALK Crizotinib; Alectinib; Ceritinib; Lorlatinib; Brigatinib ALK (7%) ROS1 EGFR other (4%) Crizotinib; Cabozantinib;Ceritinib; Lorlatinib; Entrectinib; Ropotrectinib, DS-6051b MET (3%) BRAF >1 mutation (3%) Vemurafenib;Dabrafenib;Dabrafenib + Trametinib HER2 (2%) MET Crizotinib; Cabozantinib; Capmatinib; Savolitinib; Tepotinib; Merestinib; Glesatinib ROS1 (2%) BRAF (2%) HER2 Trastuzumab emtansine;Afatinib; Neratinib-temsirolimus; Dacomitinib; Poziotinib; RET (2%) XMT-1522; TAK-788; DS-8201a, NTRK1 (1%) RET Cabozantinib; Alectinib; Apatinib;