BRAF, MET, and Her2 Mutations in Lung Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Successful Chemotherapy Is Possible for Seemingly Inoperable Anaplastic Thyroid Cancer
® Clinical Thyroidology for the Public VOLUME 12 | ISSUE 12 | DECEMBER 2019 THYROID CANCER Successful chemotherapy is possible for seemingly inoperable anaplastic thyroid cancer BACKGROUND form of standard chemotherapy and 2 received another While the vast majority of thyroid cancers are slow tyrosine kinase inhibitor called pembrolizumab. Of the 6 growing and have an excellent prognosis, anaplastic patients that had surgery after this treatment, 4 patients thyroid cancer, which makes up <1% of all thyroid cancer, had the entire primary cancer removed and the other 2 is one of the most aggressive of all cancers, with a survival patients only had microscopic pieces of cancer left after averaging ~6 months after diagnosis. Surgery, radiation the surgery. After the surgery, 5 of 6 patients received and single drug chemotherapy is all ineffective in most standard chemotherapy and radiation to the surgical area. cases. The aim of this study is to study if combination Of the 6 patients, 4 patients had no evidence of cancer at chemotherapy will make previously inoperable anaplastic the last check, some over 2 years after surgery. The 2 other thyroid cancers safe to remove with surgery. patients did pass away from anaplastic cancer; however, there was no re-growth of cancer in the area where surgery THE FULL ARTICLE TITLE occurred. Wang JR et al 2019 Complete surgical resection following neoadjuvant dabrafenib plus trametinib in BRAFV600E- WHAT ARE THE IMPLICATIONS mutated anaplastic thyroid carcinoma. Thyroid 29:1036– OF THIS STUDY? 1043. PMID: 31319771. In selected patients with anaplastic thyroid cancer with the BRAF V600E mutation, treatment with dabrafenib SUMMARY OF THE STUDY and trametinib may increase the chance of having a In this study from the MD Anderson Cancer Center successful surgery of the primary tumor. -
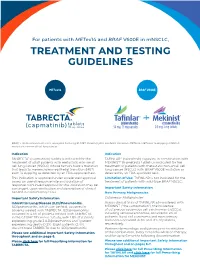
Treatment and Testing Guidelines
For patients with METex14 and BRAF V600E in mNSCLC, TREATMENT AND TESTING GUIDELINES METex14 BRAF V600E BRAF, v-raf murine sarcoma viral oncogene homolog B1; MET, mesenchymal-epithelial transition; METex14, MET exon 14 skipping; mNSCLC, metastatic non-small cell lung cancer. Indication Indication TABRECTA® (capmatinib) tablets is indicated for the TAFINLAR® (dabrafenib) capsules, in combination with treatment of adult patients with metastatic non-small MEKINIST® (trametinib) tablets, is indicated for the cell lung cancer (NSCLC) whose tumors have a mutation treatment of patients with metastatic non-small cell that leads to mesenchymal-epithelial transition (MET) lung cancer (NSCLC) with BRAF V600E mutation as exon 14 skipping as detected by an FDA-approved test. detected by an FDA-approved test. This indication is approved under accelerated approval Limitation of Use: TAFINLAR is not indicated for the based on overall response rate and duration of treatment of patients with wild-type BRAF NSCLC. response. Continued approval for this indication may be contingent upon verification and description of clinical Important Safety Information benefit in confirmatory trials. New Primary Malignancies. Important Safety Information Cutaneous Malignancies Interstitial Lung Disease (ILD)/Pneumonitis. Across clinical trials of TAFINLAR administered with ILD/pneumonitis, which can be fatal, occurred in MEKINIST (“the combination”), the incidence patients treated with TABRECTA. ILD/pneumonitis of cutaneous squamous cell carcinomas (cuSCCs), occurred in 4.5% of patients treated with TABRECTA including keratoacanthomas, occurred in 2% of in the GEOMETRY mono-1 study, with 1.8% of patients patients. Basal cell carcinoma and new primary experiencing grade 3 ILD/pneumonitis and 1 patient melanoma occurred in 3% and <1% of patients, experiencing death (0.3%). -

Combined BRAF and MEK Inhibition with Vemurafenib and Cobimetinib for Patients with Advanced Melanoma
Review Melanoma Combined BRAF and MEK Inhibition with Vemurafenib and Cobimetinib for Patients with Advanced Melanoma Antonio M Grimaldi, Ester Simeone, Lucia Festino, Vito Vanella and Paolo A Ascierto Melanoma, Cancer Immunotherapy and Innovative Therapy Unit, Istituto Nazionale Tumori Fondazione “G. Pascale”, Napoli, Italy cquired resistance is the most common cause of BRAF inhibitor monotherapy treatment failure, with the majority of patients experiencing disease progression with a median progression-free survival of 6-8 months. As such, there has been considerable A focus on combined therapy with dual BRAF and MEK inhibition as a means to improve outcomes compared with monotherapy. In the COMBI-d and COMBI-v trials, combined dabrafenib and trametinib was associated with significant improvements in outcomes compared with dabrafenib or vemurafenib monotherapy, in patients with BRAF-mutant metastatic melanoma. The combination of vemurafenib and cobimetinib has also been investigated. In the phase III CoBRIM study in patients with unresectable stage III-IV BRAF-mutant melanoma, treatment with vemurafenib and cobimetinib resulted in significantly longer progression-free survival and overall survival (OS) compared with vemurafenib alone. One-year OS was 74.5% in the vemurafenib and cobimetinib group and 63.8% in the vemurafenib group, while 2-year OS rates were 48.3% and 38.0%, respectively. The combination was also well tolerated, with a lower incidence of cutaneous squamous-cell carcinoma and keratoacanthoma compared with monotherapy. Dual inhibition of both MEK and BRAF appears to provide a more potent and durable anti-tumour effect than BRAF monotherapy, helping to prevent acquired resistance as well as decreasing adverse events related to BRAF inhibitor-induced activation of the MAPK-pathway. -

Dangerous Liaisons: Flirtations Between Oncogenic BRAF and GRP78 in Drug-Resistant Melanomas
Dangerous liaisons: flirtations between oncogenic BRAF and GRP78 in drug-resistant melanomas Shirish Shenolikar J Clin Invest. 2014;124(3):973-976. https://doi.org/10.1172/JCI74609. Commentary BRAF mutations in aggressive melanomas result in kinase activation. BRAF inhibitors reduce BRAFV600E tumors, but rapid resistance follows. In this issue of the JCI, Ma and colleagues report that vemurafenib activates ER stress and autophagy in BRAFV600E melanoma cells, through sequestration of the ER chaperone GRP78 by the mutant BRAF and subsequent PERK activation. In preclinical studies, treating vemurafenib-resistant melanoma with a combination of vemurafenib and an autophagy inhibitor reduced tumor load. Further work is needed to establish clinical relevance of this resistance mechanism and demonstrate efficacy of autophagy and kinase inhibitor combinations in melanoma treatment. Find the latest version: https://jci.me/74609/pdf commentaries F2-2012–279017) and NEUROKINE net- from the brain maintains CNS immune tolerance. 17. Benner EJ, et al. Protective astrogenesis from the J Clin Invest. 2014;124(3):1228–1241. SVZ niche after injury is controlled by Notch mod- work (EU Framework 7 ITN project). 8. Sawamoto K, et al. New neurons follow the flow ulator Thbs4. Nature. 2013;497(7449):369–373. of cerebrospinal fluid in the adult brain. Science. 18. Sabelstrom H, et al. Resident neural stem cells Address correspondence to: Gianvito Mar- 2006;311(5761):629–632. restrict tissue damage and neuronal loss after spinal tino, Neuroimmunology Unit, Institute 9. Butti E, et al. Subventricular zone neural progeni- cord injury in mice. Science. 2013;342(6158):637–640. tors protect striatal neurons from glutamatergic 19. -

Original Research Paper In-Silico FDA-Approved Drug Repurposing to Find
Original Research Paper In-silico FDA-approved drug repurposing to find the possible treatment of Coronavirus Disease-19 (COVID-19) Kumar Sharp1, Dr. Shubhangi Dange2* 12nd MBBS undergraduate student, Government Medical College and Hospital, Jalgaon 2Associate Professor, Dept. of Microbiology, Government Medical College and Hospital, Jalgaon *Corresponding author: - Dr. Shubhangi Dange, Associate Professor, Department of Microbiology, Government Medical College and Hospital, Jalgaon Email: [email protected] Abstract Identification of potential drug-target interaction for approved drugs serves as the basis of repurposing drugs. Studies have shown polypharmacology as common phenomenon. In-silico approaches help in screening large compound libraries at once which could take years in a laboratory. We screened a library of 1050 FDA-approved drugs against spike glycoprotein of SARS-CoV2 in-silico. Anti-cancer drugs have shown good binding affinity which is much better than hydroxychloroquine and arbidol. We have also introduced a hypothesis named “Bump” hypothesis which and be developed further in field of computational biology. Keywords: spike glycoprotein; FDA; drug repurposing; anti-cancer; hydroxychloroquine Introduction Identification of potential drug-target interaction for approved drugs serves as the basis of repurposing drugs. Studies have shown polypharmacology as common phenomenon [1][2]. Since the three-dimensional structures of proteins of SARS-CoV2 have been mapped it opens opportunity for in-silico approaches of either novel drug discovery or drug repurposing. In the absence of an exact cure or vaccine, coronavirus disease-19 has taken a huge toll of humanity. Our study of target specific drug docking and novel hypothesis contributes in this fight. In-silico approaches help in screening large compound libraries at once which could take years in a laboratory. -

Tafinlar, INN-Dabrafenib
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Tafinlar 50 mg hard capsules Tafinlar 75 mg hard capsules 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Tafinlar 50 mg hard capsules Each hard capsule contains dabrafenib mesilate equivalent to 50 mg of dabrafenib. Tafinlar 75 mg hard capsules Each hard capsule contains dabrafenib mesilate equivalent to 75 mg of dabrafenib. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Hard capsule (capsule). Tafinlar 50 mg hard capsules Opaque dark red capsules, approximately 18 mm long, with capsule shell imprinted with “GS TEW” and “50 mg”. Tafinlar 75 mg hard capsules Opaque dark pink capsules, approximately 19 mm long, with capsule shell imprinted with “GS LHF” and “75 mg”. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Melanoma Dabrafenib as monotherapy or in combination with trametinib is indicated for the treatment of adult patients with unresectable or metastatic melanoma with a BRAF V600 mutation (see sections 4.4 and 5.1). Adjuvant treatment of melanoma Dabrafenib in combination with trametinib is indicated for the adjuvant treatment of adult patients with Stage III melanoma with a BRAF V600 mutation, following complete resection. Non-small cell lung cancer (NSCLC) Dabrafenib in combination with trametinib is indicated for the treatment of adult patients with advanced non-small cell lung cancer with a BRAF V600 mutation. 2 4.2 Posology and method of administration Treatment with dabrafenib should be initiated and supervised by a qualified physician experienced in the use of anticancer medicinal products. Before taking dabrafenib, patients must have confirmation of tumour BRAF V600 mutation using a validated test. -

Darkening and Eruptive Nevi During Treatment with Erlotinib
CASE LETTER Darkening and Eruptive Nevi During Treatment With Erlotinib Stephen Hemperly, DO; Tanya Ermolovich, DO; Nektarios I. Lountzis, MD; Hina A. Sheikh, MD; Stephen M. Purcell, DO A 70-year-old man with NSCLCA presented with PRACTICE POINTS eruptive nevi and darkening of existing nevi 3 months after • Cutaneous side effects of erlotinib include acneform starting monotherapy with erlotinib. Physical examina- eruption, xerosis, paronychia, and pruritus. tion demonstrated the simultaneous appearance of scat- • Clinicians should monitor patients for darkening tered acneform papules and pustules; diffuse xerosis; and and/or eruptive nevi as well as melanoma during numerous dark copybrown to black nevi on the trunk, arms, treatment with erlotinib. and legs. Compared to prior clinical photographs taken in our office, darkening of existing medium brown nevi was noted, and new nevi developed in areas where no prior nevi had been visible (Figure 1). To the Editor: notThe patient’s medical history included 3 invasive mel- Erlotinib is a small-molecule selective tyrosine kinase anomas, all of which were diagnosed at least 7 years prior inhibitor that functions by blocking the intracellular por- to the initiation of erlotinib and were treated by surgical tion of the epidermal growth factor receptor (EGFR)Do1,2; excision alone. Prior treatment of NSCLCA consisted of a EGFR normally is expressed in the basal layer of the left lower lobectomy followed by docetaxel, carboplatin, epidermis, sweat glands, and hair follicles, and is over- pegfilgrastim, dexamethasone, and pemetrexed. A thor- expressed in some cancers.1,3 Normal activation of ough review of all of the patient’s medications revealed EGFR leads to signal transduction through the mitogen- no associations with changes in nevi. -

Resistance Mechanisms to Osimertinib in EGFR-Mutated Non-Small Cell Lung Cancer
www.nature.com/bjc REVIEW ARTICLE Resistance mechanisms to osimertinib in EGFR-mutated non-small cell lung cancer Alessandro Leonetti1,2, Sugandhi Sharma2, Roberta Minari1, Paola Perego3, Elisa Giovannetti2,4 and Marcello Tiseo 1,5 Osimertinib is an irreversible, third-generation epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor that is highly selective for EGFR-activating mutations as well as the EGFR T790M mutation in patients with advanced non-small cell lung cancer (NSCLC) with EGFR oncogene addiction. Despite the documented efficacy of osimertinib in first- and second-line settings, patients inevitably develop resistance, with no further clear-cut therapeutic options to date other than chemotherapy and locally ablative therapy for selected individuals. On account of the high degree of tumour heterogeneity and adaptive cellular signalling pathways in NSCLC, the acquired osimertinib resistance is highly heterogeneous, encompassing EGFR-dependent as well as EGFR- independent mechanisms. Furthermore, data from repeat plasma genotyping analyses have highlighted differences in the frequency and preponderance of resistance mechanisms when osimertinib is administered in a front-line versus second-line setting, underlying the discrepancies in selection pressure and clonal evolution. This review summarises the molecular mechanisms of resistance to osimertinib in patients with advanced EGFR-mutated NSCLC, including MET/HER2 amplification, activation of the RAS–mitogen-activated protein kinase (MAPK) or RAS–phosphatidylinositol -

FOI Reference: FOI 414 - 2021
FOI Reference: FOI 414 - 2021 Title: Researching the Incidence and Treatment of Melanoma and Breast Cancer Date: February 2021 FOI Category: Pharmacy FOI Request: 1. How many patients are currently (in the past 3 months) undergoing treatment for melanoma, and how many of these are BRAF+? 2. In the past 3 months, how many melanoma patients (any stage) were treated with the following: • Cobimetinib • Dabrafenib • Dabrafenib AND Trametinib • Encorafenib AND Binimetinib • Ipilimumab • Ipilimumab AND Nivolumab • Nivolumab • Pembrolizumab • Trametinib • Vemurafenib • Vemurafenib AND Cobimetinib • Other active systemic anti-cancer therapy • Palliative care only 3. If possible, could you please provide the patients treated in the past 3 months with the following therapies for metastatic melanoma ONLY: • Ipilimumab • Ipilimumab AND Nivolumab • Nivolumab • Pembrolizumab • Any other therapies 4. In the past 3 months how many patients were treated with the following for breast cancer? • Abemaciclib + Anastrozole/Exemestane/Letrozole • Abemaciclib + Fulvestrant • Alpelisib + Fulvestrant • Atezolizumab • Bevacizumab [Type text] • Eribulin • Everolimus + Exemestane • Fulvestrant as a single agent • Gemcitabine + Paclitaxel • Lapatinib • Neratinib • Olaparib • Palbociclib + Anastrozole/Exemestane/Letrozole • Palbociclib + Fulvestrant • Pertuzumab + Trastuzumab + Docetaxel • Ribociclib + Anastrozole/Exemestane/Letrozole • Ribociclib + Fulvestrant • Talazoparib • Transtuzumab + Paclitaxel • Transtuzumab as a single agent • Trastuzumab emtansine • Any other -

Cotellic, INN-Cobimetinib
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Cotellic 20 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each film-coated tablet contains cobimetinib hemifumarate equivalent to 20 mg cobimetinib. Excipient with known effect Each film-coated tablet contains 36 mg lactose monohydrate. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet. White, round film-coated tablets of approximately 6.6 mm diameter, with “COB” debossed on one side. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Cotellic is indicated for use in combination with vemurafenib for the treatment of adult patients with unresectable or metastatic melanoma with a BRAF V600 mutation (see sections 4.4 and 5.1). 4.2 Posology and method of administration Treatment with Cotellic in combination with vemurafenib should only be initiated and supervised by a qualified physician experienced in the use of anticancer medicinal products. Before starting this treatment, patients must have BRAF V600 mutation-positive melanoma tumour status confirmed by a validated test (see sections 4.4 and 5.1). Posology The recommended dose of Cotellic is 60 mg (3 tablets of 20 mg) once daily. Cotellic is taken on a 28 day cycle. Each dose consists of three 20 mg tablets (60 mg) and should be taken once daily for 21 consecutive days (Days 1 to 21-treatment period); followed by a 7-day break (Days 22 to 28-treatment break). Each subsequent Cotellic treatment cycle should start after the 7-day treatment break has elapsed. For information on the posology of vemurafenib, please refer to its SmPC. -
Crusader Q2 2020 Research Edition Download
Your resource for the latest research into the MET alteration. CRUSADER NEWSLETTER Q2 2020 RESEARCH EDITION MET Crusaders is a community of Lung Cancer patients and care givers collaborating with advocates and medical professionals collectively dedicated to helping patients with a MET alteration live normal lives. Come Join Us! [email protected] In this edition Top-level MET gene copy number gain defines .................... 2 Molecular Mechanisms of Acquired Resistance ................... 5 a subtype of poorly differentiated pulmonary to MET Tyrosine Kinase Inhibitors in Patients adenocarcinomas with poor prognosis with MET Exon 14-Mutant NSCLC EDITOR Characteristics and Clinical Outcomes of ............................. 2 MET Alterations Are a Recurring and Actionable .................. 6 Jessica McKernan, PharmD Non-Small Cell Lung Cancer Patients in Korea Resistance Mechanism in ALK-Positive Lung Cancer with MET Exon 14 Skipping Atrium Health Tepotinib in Non-Small-Cell Lung Cancer with ...................... 6 Charlotte, NC Clinical and molecular correlates of PD-L1 ........................... 2 MET Exon 14 Skipping Mutations (VISION Trial) expression in patients with lung adenocarcinomas Therapeutic Efficacy of ABN401, a Highly ............................. 7 CONTRIBUTING EDITORS Efficacy and Safety of Anti-PD-1 Immunotherapy ................. 3 Potent and Selective MET Inhibitor, Based on Julia Stevens, PharmD in Patients With Advanced NSCLC With BRAF, HER2, Diagnostic Biomarker Test in MET-Addicted Cancer or MET Mutations or RET Translocation: GFPC 01-2018 Beth Israel Deaconess Erlotinib plus tivantinib versus erlotinib alone ..................... 7 Medical Center Alterations in the PI3K Pathway Drive Resistance ................ 3 in patients with previously treated stage IIIb/IV Boston, MA to MET Inhibitors in NSCLC Harboring MET non-small-cell lung cancer: A meta-analysis based Exon 14 Skipping Mutations on randomized controlled trials Laura Schmidt, PharmD Incidence and PD-L1 Expression of MET 14 ......................... -

Tepotinib) Tablets, for Oral Use Any Severity
HIGHLIGHTS OF PRESCRIBING INFORMATION ------------------------WARNINGS AND PRECAUTIONS----------------------- These highlights do not include all the information needed to use TEPMETKO safely and effectively. See full prescribing information for • Interstitial Lung Disease (ILD)/Pneumonitis: Immediately withhold TEPMETKO. TEPMETKO in patients with suspected ILD/pneumonitis. Permanently discontinue TEPMETKO in patients diagnosed with ILD/pneumonitis of TEPMETKO® (tepotinib) tablets, for oral use any severity. (2.3, 5.1) Initial U.S. Approval: 2021 • Hepatotoxicity: Monitor liver function tests. Withhold, dose reduce, or permanently discontinue TEPMETKO based on severity. (5.2) ----------------------------INDICATIONS AND USAGE--------------------------- • Embryo-fetal toxicity: TEPMETKO can cause fetal harm. Advise of potential risk to a fetus and use of effective contraception. (5.3, 8.1, 8.3) TEPMETKO is a kinase inhibitor indicated for the treatment of adult patients with metastatic non-small cell lung cancer (NSCLC) harboring mesenchymal- -------------------------------ADVERSE REACTIONS------------------------------ epithelial transition (MET) exon 14 skipping alterations. (1) Most common adverse reactions (≥ 20%) were edema, fatigue, nausea, This indication is approved under accelerated approval based on overall diarrhea, musculoskeletal pain, and dyspnea. The most common Grade 3 to 4 response rate and duration of response. Continued approval for this indication laboratory abnormalities (≥ 2%) were decreased lymphocytes, decreased may be contingent upon verification and description of clinical benefit in albumin, decreased sodium, increased gamma-glutamyltransferase, increased confirmatory trials. (1) amylase, increased ALT, increased AST, and decreased hemoglobin. (6.1) -----------------------DOSAGE AND ADMINISTRATION----------------------- To report SUSPECTED ADVERSE REACTIONS, contact EMD Serono at 1-800-283-8088 ext. 5563 or FDA at 1-800-FDA-1088 or • Select patients for treatment with TEPMETKO on the presence of METex14 www.fda.gov/medwatch.