Unitedhealthcare Cancer Therapy Pathways Program Regimens
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cstone's Partner Blueprint Medicines Presented Updated Part 1 Data from PIONEER Trial of Avapritinib
Hong Kong Exchanges and Clearing Limited and The Stock Exchange of Hong Kong Limited take no responsibility for the contents of this announcement, make no representation as to its accuracy or completeness and expressly disclaim any liability whatsoever for any loss howsoever arising from or in reliance upon the whole or any part of the contents of this announcement. The forward-looking statements made in this announcement relate only to the events or information as of the date on which the statements are made in this announcement. Except as required by law, we undertake no obligation to update or revise publicly any forward-looking statements, whether as a result of new information, future events or otherwise, after the date on which the statements are made or to reflect the occurrence of unanticipated events. You should read this announcement completely and with the understanding that our actual future results or performance may be materially different from what we expect. In this announcement, statements of, or references to, our intentions or those of any of our directors and/or our Company are made as of the date of this announcement. Any of these intentions may alter in light of future development. CStone Pharmaceuticals 基 石 藥 業 (Incorporated in the Cayman Islands with limited liability) (Stock Code: 2616) VOLUNTARY ANNOUNCEMENT CSTONE’S PARTNER BLUEPRINT MEDICINES PRESENTED UPDATED PART 1 DATA FROM PIONEER TRIAL OF AVAPRITINIB SHOWING ROBUST REDUCTIONS IN CUTANEOUS DISEASE SYMPTOMS IN PATIENTS WITH INDOLENT SYSTEMIC MASTOCYTOSIS The partner of CStone Pharmaceuticals (the “Company” or “CStone”), Blueprint Medicines Corporation (NASDAQ: BPMC) (“Blueprint Medicines”), announced on June 6 updated clinical data from part 1 of the PIONEER trial showing robust and consistent clinical activity for avapritinib across multiple qualitative and quantitative measures of cutaneous disease in patients with indolent systemic mastocytosis (“ISM”). -

Clinical Response of the Novel Activating ALK-I1171T
http://www.diva-portal.org This is the published version of a paper published in Cold Spring Harbor Molecular Case Studies. Citation for the original published paper (version of record): Guan, J., Fransson, S., Siaw, J T., Treis, D., Van den Eynden, J. et al. (2018) Clinical response of the novel activating ALK-I1171T mutation in neuroblastoma o the ALK inhibitor ceritinib Cold Spring Harbor Molecular Case Studies, 4(4): a002550 https://doi.org/10.1101/mcs.a002550 Access to the published version may require subscription. N.B. When citing this work, cite the original published paper. Permanent link to this version: http://urn.kb.se/resolve?urn=urn:nbn:se:umu:diva-154087 Downloaded from molecularcasestudies.cshlp.org on December 12, 2018 - Published by Cold Spring Harbor Laboratory Press COLD SPRING HARBOR Molecular Case Studies | RESEARCH ARTICLE Clinical response of the novel activating ALK-I1171T mutation in neuroblastoma to the ALK inhibitor ceritinib Jikui Guan,1,2,12 Susanne Fransson,3,12 Joachim Tetteh Siaw,1,12 Diana Treis,4,12 Jimmy Van den Eynden,1 Damini Chand,1 Ganesh Umapathy,1 Kristina Ruuth,5 Petter Svenberg,4 Sandra Wessman,6,7 Alia Shamikh,6,7 Hans Jacobsson,8 Lena Gordon,9 Jakob Stenman,10 Pär-Johan Svensson,10 Magnus Hansson,11 Erik Larsson,1 Tommy Martinsson,3 Ruth H. Palmer,1 Per Kogner,6,7 and Bengt Hallberg1 1Department of Medical Biochemistry and Cell Biology, Institute of Biomedicine, The Sahlgrenska Academy, University of Gothenburg, Gothenburg 40530, Sweden; 2Children’s Hospital Affiliated to Zhengzhou University, -

Alectinib Provides a New Option for ALK-Positive NSCLC Patients After Progression on Crizotinib See Commentary on Page 239
Community Translations Edited by Jame Abraham, MD, FACP Alectinib provides a new option for ALK-positive NSCLC patients after progression on crizotinib See Commentary on page 239 n December 2015, alectinib became the third ALK inhibitor approved by the United States Food and What’s new, what’s important IDrug Administration for the treatment of non-small- The US Food and Drug Administration approved alectinib to cell lung cancer (NSCLC) that displays rearrangements of treat patients with metastatic ALK-positive non-small-cell lung the anaplastic lymphoma kinase (ALK) gene. Alectinib is cancer whose disease had progressed or who could not toler- a second-generation small molecule inhibitor of the ALK ate treatment with crizotinib. In clinical trials, alectinib showed a protein that joins ceritinib in providing a useful treatment partial response of 38%-44% and an average progression-free option for patients who have progressed on crizotinib, as survival of 11.2 months. In all, 61% of patients experienced a a result of its ability to target crizotinib-resistant mutant complete or partial reduction in their brain metastatic lesions, forms of the ALK protein. Alectinib also displays enhanced with a progression-free survival of of 9.1 months. The recom- penetrance of the blood-brain barrier, which improves ef- mended dose is 600 mg orally twice daily. cacy against central nervous system (CNS) metastases. The most common side effects are fatigue, constipation, swell- Te FDA awarded alectinib accelerated approval on the ing (edema), and muscle pain (myalgia). Treatment with alec- basis of 2 phase 2, single-arm clinical trials in patients tinib may cause sunburn when patients are exposed to sunlight, with ALK-positive NSCLC who had progressed on and pregnant women should be notifed of the possible risk to crizotinib therapy, a group of patients who have few avail- the fetus, and to use contraception throughout treatment and for able treatment options. -

Pharmaceutics of Oral Anticancer Agents and Stimulants
Pharmaceutics of oral anticancer agents and stimulants Maikel Herbrink The research in this thesis was performed at the Departments of Pharmacy & Pharma- cology and Medical Oncology & Clinical Pharmacology of the Netherlands Cancer Insti- tute – Antoni van Leeuwenhoek hospital, Amsterdam, the Netherlands. Printing of this thesis was financially supported by: Netherlands Cancer Institute Chipsoft BV Pfizer BV ISBN: 978-90-393-6997-5 Design, lay-out and print Gildeprint, Enschede © Maikel Herbrink, 2018 Pharmaceutics of oral anticancer agents and stimulants Farmaceutisch onderzoek naar oraal toegediende antikankermiddelen en stimulantia (met een samenvatting in het Nederlands) Proefschrift ter verkrijging van de graad van doctor aan de Universiteit Utrecht op gezag van de rector magnificus, prof. dr. H.R.B.M. Kummeling, ingevolge het besluit van het college voor promoties in het openbaar te verdedigen op woensdag 27 juni 2018 des middags te 4.15 uur door Maikel Herbrink geboren op 2 februari 1990 te Groningen Promotoren: Prof. dr. J.H. Beijnen Prof. dr. J.H.M. Schellens Copromotor: Dr. B. Nuijen Contents Preface 9 Chapter 1: Introduction 15 1.1 Variability in bioavailability of small molecular tyrosine 17 kinase inhibitors Cancer Treat Rev. 2015 May;41(5):412-422 1.2 Inherent formulation issues of kinase inhibitors 51 J Control Release. 2016 Oct;239:118-127 1.3 High-tech drugs in creaky formulations 81 Pharm Res. 2017 Sep;34(9):1751-1753 Chapter 2: Pharmaceutical analysis of oral anticancer drug substances 89 2.1. Thermal study of pazopanib hydrochloride 91 J Therm Anal Calorim. 2017 Dec;130(3):1491-1499 2.2. -

ZYKADIA (Ceritinib) RATIONALE for INCLUSION in PA PROGRAM
ZYKADIA (ceritinib) RATIONALE FOR INCLUSION IN PA PROGRAM Background Zykadia is used in patients with a certain type of late-stage (metastatic) non-small cell lung cancer (NSCLC), which is caused by a defect in a gene called anaplastic lymphoma kinase (ALK). Zykadia is a tyrosine kinase inhibitor that blocks proteins that promote the development of cancerous cells. It is intended for patients with metastatic ALK-positive NSCLC (1). Regulatory Status FDA- approved indication: Zykadia is a kinase inhibitor indicated for the treatment of patients with anaplastic lymphoma kinase (ALK)-positive metastatic non-small cell lung cancer (NSCLC) as detected by an FDA-approved test (1). Off-Label Uses: (2-3) 1. Inflammatory Myofibroblastic Tumor (IMT) with ALK translocation Zykadia can cause hepatotoxicity therefore liver function tests including AST, ALT and total bilirubin should be monitored at least monthly. Zykadia can cause interstitial lung disease (ILD) or pneumonitis. Zykadia should be permanently discontinued in patients diagnosed with treatment- related ILD/pneumonitis. Zykadia can cause QTc interval prolongation, which requires monitoring of electrocardiograms and electrolytes in patients with congestive heart failure (1). Zykadia is pregnancy category D and may cause fetal harm when administered to a pregnant woman (1). Safety and effectiveness of Zykadia in pediatric patients have not been established (1). Summary Zykadia is an anaplastic lymphoma kinase (ALK) tyrosine kinase inhibitor that blocks proteins that promote the development of cancerous cells. It is intended for patients with metastatic ALK-positive NSCLC. Safety and effectiveness of Zykadia in patients under 18 years of age have not been established (1). Zykadia FEP Clinical Rationale ZYKADIA (ceritinib) Prior approval is required to ensure the safe, clinically appropriate and cost effective use of Zykadia while maintaining optimal therapeutic outcomes. -

07052020 MR ASCO20 Curtain Raiser
Media Release New data at the ASCO20 Virtual Scientific Program reflects Roche’s commitment to accelerating progress in cancer care First clinical data from tiragolumab, Roche’s novel anti-TIGIT cancer immunotherapy, in combination with Tecentriq® (atezolizumab) in patients with PD-L1-positive metastatic non- small cell lung cancer (NSCLC) Updated overall survival data for Alecensa® (alectinib), in people living with anaplastic lymphoma kinase (ALK)-positive metastatic NSCLC Key highlights to be shared on Roche’s ASCO virtual newsroom, 29 May 2020, 08:00 CEST Basel, 7 May 2020 - Roche (SIX: RO, ROG; OTCQX: RHHBY) today announced that new data from clinical trials of 19 approved and investigational medicines across 21 cancer types, will be presented at the ASCO20 Virtual Scientific Program organised by the American Society of Clinical Oncology (ASCO), which will be held 29-31 May, 2020. A total of 120 abstracts that include a Roche medicine will be presented at this year's meeting. "At ASCO, we will present new data from many investigational and approved medicines across our broad oncology portfolio," said Levi Garraway, M.D., Ph.D., Roche's Chief Medical Officer and Head of Global Product Development. “These efforts exemplify our long-standing commitment to improving outcomes for people with cancer, even during these unprecedented times. By integrating our medicines and diagnostics together with advanced insights and novel platforms, Roche is uniquely positioned to deliver the healthcare solutions of the future." Together with its partners, Roche is pioneering a comprehensive approach to cancer care, combining new diagnostics and treatments with innovative, integrated data and access solutions for approved medicines that will both personalise and transform the outcomes of people affected by this deadly disease. -
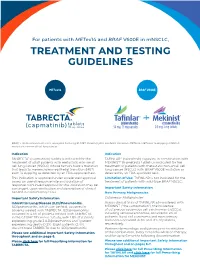
Treatment and Testing Guidelines
For patients with METex14 and BRAF V600E in mNSCLC, TREATMENT AND TESTING GUIDELINES METex14 BRAF V600E BRAF, v-raf murine sarcoma viral oncogene homolog B1; MET, mesenchymal-epithelial transition; METex14, MET exon 14 skipping; mNSCLC, metastatic non-small cell lung cancer. Indication Indication TABRECTA® (capmatinib) tablets is indicated for the TAFINLAR® (dabrafenib) capsules, in combination with treatment of adult patients with metastatic non-small MEKINIST® (trametinib) tablets, is indicated for the cell lung cancer (NSCLC) whose tumors have a mutation treatment of patients with metastatic non-small cell that leads to mesenchymal-epithelial transition (MET) lung cancer (NSCLC) with BRAF V600E mutation as exon 14 skipping as detected by an FDA-approved test. detected by an FDA-approved test. This indication is approved under accelerated approval Limitation of Use: TAFINLAR is not indicated for the based on overall response rate and duration of treatment of patients with wild-type BRAF NSCLC. response. Continued approval for this indication may be contingent upon verification and description of clinical Important Safety Information benefit in confirmatory trials. New Primary Malignancies. Important Safety Information Cutaneous Malignancies Interstitial Lung Disease (ILD)/Pneumonitis. Across clinical trials of TAFINLAR administered with ILD/pneumonitis, which can be fatal, occurred in MEKINIST (“the combination”), the incidence patients treated with TABRECTA. ILD/pneumonitis of cutaneous squamous cell carcinomas (cuSCCs), occurred in 4.5% of patients treated with TABRECTA including keratoacanthomas, occurred in 2% of in the GEOMETRY mono-1 study, with 1.8% of patients patients. Basal cell carcinoma and new primary experiencing grade 3 ILD/pneumonitis and 1 patient melanoma occurred in 3% and <1% of patients, experiencing death (0.3%). -

Horizon Scanning Status Report June 2019
Statement of Funding and Purpose This report incorporates data collected during implementation of the Patient-Centered Outcomes Research Institute (PCORI) Health Care Horizon Scanning System, operated by ECRI Institute under contract to PCORI, Washington, DC (Contract No. MSA-HORIZSCAN-ECRI-ENG- 2018.7.12). The findings and conclusions in this document are those of the authors, who are responsible for its content. No statement in this report should be construed as an official position of PCORI. An intervention that potentially meets inclusion criteria might not appear in this report simply because the horizon scanning system has not yet detected it or it does not yet meet inclusion criteria outlined in the PCORI Health Care Horizon Scanning System: Horizon Scanning Protocol and Operations Manual. Inclusion or absence of interventions in the horizon scanning reports will change over time as new information is collected; therefore, inclusion or absence should not be construed as either an endorsement or rejection of specific interventions. A representative from PCORI served as a contracting officer’s technical representative and provided input during the implementation of the horizon scanning system. PCORI does not directly participate in horizon scanning or assessing leads or topics and did not provide opinions regarding potential impact of interventions. Financial Disclosure Statement None of the individuals compiling this information have any affiliations or financial involvement that conflicts with the material presented in this report. Public Domain Notice This document is in the public domain and may be used and reprinted without special permission. Citation of the source is appreciated. All statements, findings, and conclusions in this publication are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI) or its Board of Governors. -

Lenvatinib in Advanced, Radioactive Iodine– Refractory, Differentiated Thyroid Carcinoma Kay T
Published OnlineFirst October 20, 2015; DOI: 10.1158/1078-0432.CCR-15-0923 CCR Drug Updates Clinical Cancer Research Lenvatinib in Advanced, Radioactive Iodine– Refractory, Differentiated Thyroid Carcinoma Kay T. Yeung1 and Ezra E.W. Cohen2 Abstract Management options are limited for patients with radioactive therapy for these patients. Median PFS of 18.3 months in the iodine refractory, locally advanced, or metastatic differentiated lenvatinib group was significantly improved from 3.6 months in thyroid carcinoma. Prior to 2015, sorafenib, a multitargeted the placebo group, with an HR of 0.21 (95% confidence interval, tyrosine kinase inhibitor, was the only approved treatment and 0.4–0.31; P < 0.0001). ORR was also significantly increased in the was associated with a median progression-free survival (PFS) of lenvatinib arm (64.7%) compared with placebo (1.5%). In this 11 months and overall response rate (ORR) of 12% in a phase III article, we will review the molecular mechanisms of lenvatinib, trial. Lenvatinib, a multikinase inhibitor with high potency the data from preclinical studies to the recent phase III clinical against VEGFR and FGFR demonstrated encouraging results in trial, and the biomarkers being studied to further guide patient phase II trials. Recently, the pivotal SELECT trial provided the selection and predict treatment response. Clin Cancer Res; 21(24); basis for the FDA approval of lenvatinib as a second targeted 5420–6. Ó2015 AACR. Introduction PI3K–mTOR pathways (reviewed in ref. 3). The signals ultimately converge in the nucleus, influencing transcription of oncogenic Thyroid carcinoma is the most common endocrine malignan- proteins including, but not limited to, NF-kB), hypoxia-induced cy, with an estimated incidence rate of 13.5 per 100,000 people factor 1 alpha unit (HIF1a), TGFb, VEGF, and FGF. -

Cogent Biosciences Announces Creation of Cogent Research Team
Cogent Biosciences Announces Creation of Cogent Research Team April 6, 2021 Names industry veteran John Robinson, PhD as Chief Scientific Officer New Boulder-based team with exceptional track record of drug discovery and development focused on creating novel small molecule therapies for rare, genetically driven diseases Strong year-end cash position of $242.2 million supports company goals into 2024, including three CGT9486 clinical trials on-track to start this year, beginning with ASM in 1H21 BOULDER, Colo. and CAMBRIDGE, Mass., April 6, 2021 /PRNewswire/ -- Cogent Biosciences, Inc. (Nasdaq: COGT), a biotechnology company focused on developing precision therapies for genetically defined diseases, today announced the formation of the Cogent Research Team led by newly appointed Chief Scientific Officer, John Robinson, PhD. "Today marks an important step forward for Cogent Biosciences as we announce the formation of the Cogent Research Team with a focus on discovering and developing new small molecule therapies for patients fighting rare, genetically driven diseases," said Andrew Robbins, President and Chief Executive Officer of Cogent Biosciences. "I am thrilled to welcome John onboard as Cogent Biosciences' Chief Scientific Officer. John's expertise and seasoned leadership make him ideally suited to lead this new team of world class scientists. Given the team's impressive experience and accomplishments, we are excited for Cogent Biosciences' future and the opportunity to expand our pipeline and deliver novel precision therapies for patients." With an exceptional track record of innovation, the Cogent Research Team will focus on pioneering best-in-class, small molecule therapeutics to both improve upon existing drugs with clear limitations, as well as create new breakthroughs for diseases where others have been unable to find solutions. -

(Rituxan®), Rituximab-Abbs (Truxima®), Rituximab-Pvvr (Ruxience®) Prior Authorization Drug Coverage Policy
1 Rituximab Products: Rituximab (Rituxan®), Rituximab-abbs (Truxima®), Rituximab-pvvr (Ruxience®) Prior Authorization Drug Coverage Policy Effective Date: 2/1/2021 Revision Date: n/a Review Date: 7/2/20 Lines of Business: Commercial Policy type: Prior Authorization This Drug Coverage Policy provides parameters for the coverage of rituximab (Rituxan®), rituximab-abbs (Truxima®), and rituximab-pvvr (Ruxience®). Consideration of medically necessary indications are based upon U.S. Food and Drug Administration (FDA) indications, recommended uses within the Centers of Medicare & Medicaid Services (CMS) five recognized compendia, including the National Comprehensive Cancer Network (NCCN) Drugs & Biologics Compendium (Category 1 or 2A recommendations), and peer-reviewed scientific literature eligible for coverage according to the CMS, Medicare Benefit Policy Manual, Chapter 15, section 50.4.5 titled, “Off- Label Use of Anti-Cancer Drugs and Biologics.” This policy evaluates whether the drug therapy is proven to be effective based on published evidence-based medicine. Drug Description1-3 Rituximab (Rituxan®), rituximab-abbs (Truxima®), and rituximab-pvvr (Ruxience®) are monoclonal antibodies that target the CD20 antigen expressed on the surface of pre-B and mature B- lymphocytes. Upon binding to cluster of differentiation (CD) 20, rituximab mediates B-cell lysis. Possible mechanisms of cell lysis include complement dependent cytotoxicity (CDC) and antibody dependent cell mediated cytotoxicity (ADCC). B cells are believed to play a role in the pathogenesis of rheumatoid arthritis (RA) and associated chronic synovitis. In this setting, B cells may be acting at multiple sites in the autoimmune/inflammatory process, including through production of rheumatoid factor (RF) and other autoantibodies, antigen presentation, T-cell activation, and/or proinflammatory cytokine production. -

Resistance Mechanisms to Osimertinib in EGFR-Mutated Non-Small Cell Lung Cancer
www.nature.com/bjc REVIEW ARTICLE Resistance mechanisms to osimertinib in EGFR-mutated non-small cell lung cancer Alessandro Leonetti1,2, Sugandhi Sharma2, Roberta Minari1, Paola Perego3, Elisa Giovannetti2,4 and Marcello Tiseo 1,5 Osimertinib is an irreversible, third-generation epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor that is highly selective for EGFR-activating mutations as well as the EGFR T790M mutation in patients with advanced non-small cell lung cancer (NSCLC) with EGFR oncogene addiction. Despite the documented efficacy of osimertinib in first- and second-line settings, patients inevitably develop resistance, with no further clear-cut therapeutic options to date other than chemotherapy and locally ablative therapy for selected individuals. On account of the high degree of tumour heterogeneity and adaptive cellular signalling pathways in NSCLC, the acquired osimertinib resistance is highly heterogeneous, encompassing EGFR-dependent as well as EGFR- independent mechanisms. Furthermore, data from repeat plasma genotyping analyses have highlighted differences in the frequency and preponderance of resistance mechanisms when osimertinib is administered in a front-line versus second-line setting, underlying the discrepancies in selection pressure and clonal evolution. This review summarises the molecular mechanisms of resistance to osimertinib in patients with advanced EGFR-mutated NSCLC, including MET/HER2 amplification, activation of the RAS–mitogen-activated protein kinase (MAPK) or RAS–phosphatidylinositol