New Developments in Amatoxin Poisoning
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ecology of Cirsium Vulgare and Silybum Marianum in Relation To
Plant Protection Quarterly Vol.11 Supplement 2 1996 245 International Symposium on Biological Control of Weeds, pp. 495-501. Olivieri, I., Swan, M. and Gouyon, P.H. Ecology of Cirsium vulgare and Silybum marianum (1983). Reproductive system and colo- in relation to biological control nizing strategy of two species of Carduus (Compositae). Oecologia 60, 114-7. E. Bruzzese, Keith Turnbull Research Institute, Co-operative Research Centre Shea, K. (1996). Estimating the impact of for Weed Management Systems, PO Box 48, Frankston, Victoria 3199, Australia. control efforts: models of population dynamics. Plant Protection Quarterly 11, 263-5. Summary The ecology of spear thistle Sheppard A.W. (1996) Weeds in the Spear thistle (Cirsium vulgare) and vari- Spear thistle is an annual or biennial herb, Cardueae: Biological control and pat- egated thistle (Silybum marianum) are depending on its time of germination. Al- terns of herbivory. Proceedings of the two of the most widespread thistles though seed can germinate at any time of International Compositae Conference, which infest pastures in temperate south- the year, there are two main germination Kew, 1994, Volume 2 Biology and Utili- ern Australia. A biological control pro- times in late-summer to autumn and late zation, pp. 291-306. gram targeting these thistles was com- winter to spring (Bruzzese and Heap un- Sheppard, A.W. and Woodburn, T.L. menced in 1985. No specific ecological published). Because of this, infestations (1996). Population regulation in insects studies of these thistles and their preda- can consist of plants of different size and used to control thistles: can we predict tors in the area of origin aimed at the se- ages. -

Blessed Thistle
Léo Désilets Master Herbalist 35, Victoria West, Scotstown, QC, J0B 3B0 (819) 657-4733 • leo-desilets.com IN C CA E AN IN N D A E A D A D D A A M A M • • F • F A • A A I I T A D T D A A A A U N U A N C C A BLESSED THISTLE Traditionally used in Herbal Medicine as a digestive tonic and bitter to increase appetite and aid gigestion (stomachic). Product number........................................... NPN 80004247 Dosage form ........................................... Vegetable capsule Quantity........................................................... 90 Active Ingredient ............................... Blessed Thistle - Aerial Parties Dosage ....................................................... 320 mg Product number........................................... NPN 80073494 Dosage form ........................................... Vegetable capsule Quantity........................................................... 60 Therapeutic indications Active Ingredient ............................... Blessed Thistle - Aerial Parties • Traditionally used in Herbal Dosage ....................................... 75 mg (20:1, QCE 1500 mg) Medicine as a digestive tonic and bitter to increase appetite and help digestion. Blessed Thistle can accompany the process of digestion by stimulating secretions It is recommended to take and promoting nutrient absorption. 1 capsule 3 times daily with a glass of water at mealtime. Digestive bitter : Cnicus benedictus Digestive bitters, also known as tonic herbs, or digestive herbs stimulate the Classification (USDA) -

Bur¯Aq Depicted As Amanita Muscaria in a 15Th Century Timurid-Illuminated Manuscript?
ORIGINAL ARTICLE Journal of Psychedelic Studies 3(2), pp. 133–141 (2019) DOI: 10.1556/2054.2019.023 First published online September 24, 2019 Bur¯aq depicted as Amanita muscaria in a 15th century Timurid-illuminated manuscript? ALAN PIPER* Independent Scholar, Newham, London, UK (Received: May 8, 2019; accepted: August 2, 2019) A series of illustrations in a 15th century Timurid manuscript record the mi’raj, the ascent through the seven heavens by Mohammed, the Prophet of Islam. Several of the illustrations depict Bur¯aq, the fabulous creature by means of which Mohammed achieves his ascent, with distinctive features of the Amanita muscaria mushroom. A. muscaria or “fly agaric” is a psychoactive mushroom used by Siberian shamans to enter the spirit world for the purposes of conversing with spirits or diagnosing and curing disease. Using an interdisciplinary approach, the author explores the routes by which Bur¯aq could have come to be depicted in this manuscript with the characteristics of a psychoactive fungus, when any suggestion that the Prophet might have had recourse to a drug to accomplish his spirit journey would be anathema to orthodox Islam. There is no suggestion that Mohammad’s night journey (isra) or ascent (mi’raj) was accomplished under the influence of a psychoactive mushroom or plant. Keywords: Mi’raj, Timurid, Central Asia, shamanism, Siberia, Amanita muscaria CULTURAL CONTEXT Bur¯aq depicted as Amanita muscaria in the mi’raj manscript The mi’raj manuscript In the Muslim tradition, the mi’raj was preceded by the isra or “Night Journey” during which Mohammed traveled An illustrated manuscript depicting, in a series of miniatures, overnight from Mecca to Jerusalem by means of a fabulous thesuccessivestagesofthemi’raj, the miraculous ascent of beast called Bur¯aq. -
Field Guide to Common Macrofungi in Eastern Forests and Their Ecosystem Functions
United States Department of Field Guide to Agriculture Common Macrofungi Forest Service in Eastern Forests Northern Research Station and Their Ecosystem General Technical Report NRS-79 Functions Michael E. Ostry Neil A. Anderson Joseph G. O’Brien Cover Photos Front: Morel, Morchella esculenta. Photo by Neil A. Anderson, University of Minnesota. Back: Bear’s Head Tooth, Hericium coralloides. Photo by Michael E. Ostry, U.S. Forest Service. The Authors MICHAEL E. OSTRY, research plant pathologist, U.S. Forest Service, Northern Research Station, St. Paul, MN NEIL A. ANDERSON, professor emeritus, University of Minnesota, Department of Plant Pathology, St. Paul, MN JOSEPH G. O’BRIEN, plant pathologist, U.S. Forest Service, Forest Health Protection, St. Paul, MN Manuscript received for publication 23 April 2010 Published by: For additional copies: U.S. FOREST SERVICE U.S. Forest Service 11 CAMPUS BLVD SUITE 200 Publications Distribution NEWTOWN SQUARE PA 19073 359 Main Road Delaware, OH 43015-8640 April 2011 Fax: (740)368-0152 Visit our homepage at: http://www.nrs.fs.fed.us/ CONTENTS Introduction: About this Guide 1 Mushroom Basics 2 Aspen-Birch Ecosystem Mycorrhizal On the ground associated with tree roots Fly Agaric Amanita muscaria 8 Destroying Angel Amanita virosa, A. verna, A. bisporigera 9 The Omnipresent Laccaria Laccaria bicolor 10 Aspen Bolete Leccinum aurantiacum, L. insigne 11 Birch Bolete Leccinum scabrum 12 Saprophytic Litter and Wood Decay On wood Oyster Mushroom Pleurotus populinus (P. ostreatus) 13 Artist’s Conk Ganoderma applanatum -

Elemental Analysis of Some Medicinal Plants By
Journal of Medicinal Plants Research Vol. 4(19), pp. 1987-1990, 4 October, 2010 Available online at http://www.academicjournals.org/JMPR DOI: 10.5897/JMPR10.081 ISSN 1996-0875 ©2010 Academic Journals Full Length Research Paper Elemental analysis of some medicinal plants used in traditional medicine by atomic absorption spectrophotometer (AAS) Muhammad Zafar1*, Mir Ajab Khan1, Mushtaq Ahmad1, Gul Jan1, Shazia Sultana1, Kifayat Ullah1, Sarfaraz Khan Marwat1, Farooq Ahmad2, Asma Jabeen3, Abdul Nazir1, Arshad Mehmood Abbasi1, Zia ur Rehman1 and Zahid Ullah1 1Department of Plant Sciences, Quaid-i-Azam University Islamabad Pakistan. 2Department of Botany, Pir Mehr Ali Shah Arid Agriculture University, Murree Road, Rawalpindi, Pakistan. 3Environmental Sciences Department, Fatima Jinnah Women University, Rawalpindi, Pakistan. Accepted 10 September, 2010 Different elemental constituents at trace levels of plants play an effective role in the medicines prepared. Elemental composition of different parts including leaves, seeds and fruits have been determined by using Atomic Absorption Spectrophotometer (AAS). A total of 14 elements K+, Mg+2, Ca+2, Na+, Fe+2, Co+3, Mn+2, Cu+3, Cr+3, Zn+2, Ni+3, Li+1, Pb+4 and Cd+2 have been measured. Their concentrations were found to vary in different samples. Medicinal properties of these plant samples and their elemental distribution have been correlated. Key words: Elemental analysis, medicinal plants and atomic absorption spectrophotometer. INTRODUCTION Herbal drugs are being used as remedies for various the second dist heat pathological symptoms can be diseases across the world from ancient time. In recent relieved by replacing the element. To be pharmacolo- years, increasing interest has been focused on phyto- gically effective or essential, the trace element may need medicines as safer and more congenial to the human to be combining or chelated with some ligand, in order to body. -

Advances in Anticancer Antibody-Drug Conjugates and Immunotoxins
Send Orders for Reprints to [email protected] Recent Patents on Anti-Cancer Drug Discovery, 2014, 9, 35-65 35 Advances in Anticancer Antibody-Drug Conjugates and Immunotoxins Franco Dosio1,*, Barbara Stella1, Sofia Cerioni1, Daniela Gastaldi2 and Silvia Arpicco1 1Dipartimento di Scienza e Tecnologia del Farmaco, University of Torino, Torino, I-10125, Italy; 2Dipartimento di Bio- tecnologie Molecolari e Scienze per la Salute, University of Torino, Torino, I-10125, Italy Received: December 13, 2012; Accepted: February 21, 2013; Revised: March 7, 2013 Abstract: Antibody-delivered drugs and toxins are poised to become important classes of cancer therapeutics. These bio- pharmaceuticals have potential in this field, as they can selectively direct highly potent cytotoxic agents to cancer cells that present tumor-associated surface markers, thereby minimizing systemic toxicity. The activity of some conjugates is of particular interest receiving increasing attention, thanks to very promising clinical trial results in hematologic cancers. Over twenty antibody-drug conjugates and eight immunotoxins in clinical trials as well as some recently approved drugs, support the maturity of this approach. This review focuses on recent advances in the development of these two classes of biopharmaceuticals: conventional toxins and anticancer drugs, together with their mechanisms of action. The processes of conjugation and purification, as reported in the literature and in several patents, are discussed and the most relevant results in clinical trials are listed. Innovative technologies and preliminary results on novel drugs and toxins, as reported in the literature and in recently-published patents (up to February 2013) are lastly examined. Keywords: Antibody drug conjugate, anticancer agents, auristatins immunotoxin, calicheamicins, cross-linkers, duocarmycins, maytansinoids. -

Italian Thistle (Carduus Pycnocephalus)
Thistles: Identification and Management Rebecca Ozeran 1 May 2018 Common thistles in the San Joaquin Valley Carduus Centaurea Cirsium Silybum Onopordum Italian thistle Yellow starthistle Bull thistle (Blessed) milkthistle Scotch thistle Tocalote Canada thistle (Malta starthistle) All of these species are found at least one of Fresno, Kern, Kings, Madera, or Tulare Counties Identification • Many species start as a basal rosette in fall • Mature plants can have dense & bushy or tall & stemmy appearance • Purple/pink or yellow-flowered Identification • Why does thistle species matter? • Varying levels of risk to animals • Varying competition with forage • Varying susceptibility to control options Identification – 1. Italian thistle • Carduus pycnocephalus • narrow, spiky flower heads • winged, spiny stems branching above the base • found in Fresno, Kern, Madera, Tulare Identification – 2. Centaurea thistles • YELLOW STARTHISTLE (C. solstitialis) • long, yellow/white spines on phyllaries • can get a bushy structure • found in Fresno, Kern, Madera, Tulare • TOCALOTE (MALTA STARTHISTLE, C. melitensis) • stouter flower heads and shorter, redder spines on phyllaries • found in all 5 counties Identification – 3. Cirsium thistles • Canada thistle (C. arvense) • smooth stems, non-spiny flowerheads • flowers Jun-Oct • found in Fresno, Kern, Tulare • Bull thistle (C. vulgare) • large spiky looking flowerheads • lots of branching, dense plant • flowers Jun-Oct • found in all 5 counties Identification – 4. Blessed milk thistle • Silybum marianum • Distinct, -

AMATOXIN MUSHROOM POISONING in NORTH AMERICA 2015-2016 by Michael W
VOLUME 57: 4 JULY-AUGUST 2017 www.namyco.org AMATOXIN MUSHROOM POISONING IN NORTH AMERICA 2015-2016 By Michael W. Beug: Chair, NAMA Toxicology Committee Assessing the degree of amatoxin mushroom poisoning in North America is very challenging. Understanding the potential for various treatment practices is even more daunting. Although I have been studying mushroom poisoning for 45 years now, my own views on potential best treatment practices are still evolving. While my training in enzyme kinetics helps me understand the literature about amatoxin poisoning treatments, my lack of medical training limits me. Fortunately, critical comments from six different medical doctors have been incorporated in this article. All six, each concerned about different aspects in early drafts, returned me to the peer reviewed scientific literature for additional reading. There remains no known specific antidote for amatoxin poisoning. There have not been any gold standard double-blind placebo controlled studies. There never can be. When dealing with a potentially deadly poisoning (where in many non-western countries the amatoxin fatality rate exceeds 50%) treating of half of all poisoning patients with a placebo would be unethical. Using amatoxins on large animals to test new treatments (theoretically a great alternative) has ethical constraints on the experimental design that would most likely obscure the answers researchers sought. We must thus make our best judgement based on analysis of past cases. Although that number is now large enough that we can make some good assumptions, differences of interpretation will continue. Nonetheless, we may be on the cusp of reaching some agreement. Towards that end, I have contacted several Poison Centers and NAMA will be working with the Centers for Disease Control (CDC). -
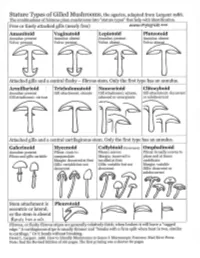
Agarics-Stature-Types.Pdf
Gilled Mushroom Genera of Chicago Region, by stature type and spore print color. Patrick Leacock – June 2016 Pale spores = white, buff, cream, pale green to Pinkish spores Brown spores = orange, Dark spores = dark olive, pale lilac, pale pink, yellow to pale = salmon, yellowish brown, rust purplish brown, orange pinkish brown brown, cinnamon, clay chocolate brown, Stature Type brown smoky, black Amanitoid Amanita [Agaricus] Vaginatoid Amanita Volvariella, [Agaricus, Coprinus+] Volvopluteus Lepiotoid Amanita, Lepiota+, Limacella Agaricus, Coprinus+ Pluteotoid [Amanita, Lepiota+] Limacella Pluteus, Bolbitius [Agaricus], Coprinus+ [Volvariella] Armillarioid [Amanita], Armillaria, Hygrophorus, Limacella, Agrocybe, Cortinarius, Coprinus+, Hypholoma, Neolentinus, Pleurotus, Tricholoma Cyclocybe, Gymnopilus Lacrymaria, Stropharia Hebeloma, Hemipholiota, Hemistropharia, Inocybe, Pholiota Tricholomatoid Clitocybe, Hygrophorus, Laccaria, Lactarius, Entoloma Cortinarius, Hebeloma, Lyophyllum, Megacollybia, Melanoleuca, Inocybe, Pholiota Russula, Tricholoma, Tricholomopsis Naucorioid Clitocybe, Hygrophorus, Hypsizygus, Laccaria, Entoloma Agrocybe, Cortinarius, Hypholoma Lactarius, Rhodocollybia, Rugosomyces, Hebeloma, Gymnopilus, Russula, Tricholoma Pholiota, Simocybe Clitocyboid Ampulloclitocybe, Armillaria, Cantharellus, Clitopilus Paxillus, [Pholiota], Clitocybe, Hygrophoropsis, Hygrophorus, Phylloporus, Tapinella Laccaria, Lactarius, Lactifluus, Lentinus, Leucopaxillus, Lyophyllum, Omphalotus, Panus, Russula Galerinoid Galerina, Pholiotina, Coprinus+, -

Toxicological and Pharmacological Profile of Amanita Muscaria (L.) Lam
Pharmacia 67(4): 317–323 DOI 10.3897/pharmacia.67.e56112 Review Article Toxicological and pharmacological profile of Amanita muscaria (L.) Lam. – a new rising opportunity for biomedicine Maria Voynova1, Aleksandar Shkondrov2, Magdalena Kondeva-Burdina1, Ilina Krasteva2 1 Laboratory of Drug metabolism and drug toxicity, Department “Pharmacology, Pharmacotherapy and Toxicology”, Faculty of Pharmacy, Medical University of Sofia, Bulgaria 2 Department of Pharmacognosy, Faculty of Pharmacy, Medical University of Sofia, Bulgaria Corresponding author: Magdalena Kondeva-Burdina ([email protected]) Received 2 July 2020 ♦ Accepted 19 August 2020 ♦ Published 26 November 2020 Citation: Voynova M, Shkondrov A, Kondeva-Burdina M, Krasteva I (2020) Toxicological and pharmacological profile of Amanita muscaria (L.) Lam. – a new rising opportunity for biomedicine. Pharmacia 67(4): 317–323. https://doi.org/10.3897/pharmacia.67. e56112 Abstract Amanita muscaria, commonly known as fly agaric, is a basidiomycete. Its main psychoactive constituents are ibotenic acid and mus- cimol, both involved in ‘pantherina-muscaria’ poisoning syndrome. The rising pharmacological and toxicological interest based on lots of contradictive opinions concerning the use of Amanita muscaria extracts’ neuroprotective role against some neurodegenerative diseases such as Parkinson’s and Alzheimer’s, its potent role in the treatment of cerebral ischaemia and other socially significant health conditions gave the basis for this review. Facts about Amanita muscaria’s morphology, chemical content, toxicological and pharmacological characteristics and usage from ancient times to present-day’s opportunities in modern medicine are presented. Keywords Amanita muscaria, muscimol, ibotenic acid Introduction rica, the genus had an ancestral origin in the Siberian-Be- ringian region in the Tertiary period (Geml et al. -

Peptide Chemistry up to Its Present State
Appendix In this Appendix biographical sketches are compiled of many scientists who have made notable contributions to the development of peptide chemistry up to its present state. We have tried to consider names mainly connected with important events during the earlier periods of peptide history, but could not include all authors mentioned in the text of this book. This is particularly true for the more recent decades when the number of peptide chemists and biologists increased to such an extent that their enumeration would have gone beyond the scope of this Appendix. 250 Appendix Plate 8. Emil Abderhalden (1877-1950), Photo Plate 9. S. Akabori Leopoldina, Halle J Plate 10. Ernst Bayer Plate 11. Karel Blaha (1926-1988) Appendix 251 Plate 12. Max Brenner Plate 13. Hans Brockmann (1903-1988) Plate 14. Victor Bruckner (1900- 1980) Plate 15. Pehr V. Edman (1916- 1977) 252 Appendix Plate 16. Lyman C. Craig (1906-1974) Plate 17. Vittorio Erspamer Plate 18. Joseph S. Fruton, Biochemist and Historian Appendix 253 Plate 19. Rolf Geiger (1923-1988) Plate 20. Wolfgang Konig Plate 21. Dorothy Hodgkins Plate. 22. Franz Hofmeister (1850-1922), (Fischer, biograph. Lexikon) 254 Appendix Plate 23. The picture shows the late Professor 1.E. Jorpes (r.j and Professor V. Mutt during their favorite pastime in the archipelago on the Baltic near Stockholm Plate 24. Ephraim Katchalski (Katzir) Plate 25. Abraham Patchornik Appendix 255 Plate 26. P.G. Katsoyannis Plate 27. George W. Kenner (1922-1978) Plate 28. Edger Lederer (1908- 1988) Plate 29. Hennann Leuchs (1879-1945) 256 Appendix Plate 30. Choh Hao Li (1913-1987) Plate 31. -

Forest Fungi in Ireland
FOREST FUNGI IN IRELAND PAUL DOWDING and LOUIS SMITH COFORD, National Council for Forest Research and Development Arena House Arena Road Sandyford Dublin 18 Ireland Tel: + 353 1 2130725 Fax: + 353 1 2130611 © COFORD 2008 First published in 2008 by COFORD, National Council for Forest Research and Development, Dublin, Ireland. All rights reserved. No part of this publication may be reproduced, or stored in a retrieval system or transmitted in any form or by any means, electronic, electrostatic, magnetic tape, mechanical, photocopying recording or otherwise, without prior permission in writing from COFORD. All photographs and illustrations are the copyright of the authors unless otherwise indicated. ISBN 1 902696 62 X Title: Forest fungi in Ireland. Authors: Paul Dowding and Louis Smith Citation: Dowding, P. and Smith, L. 2008. Forest fungi in Ireland. COFORD, Dublin. The views and opinions expressed in this publication belong to the authors alone and do not necessarily reflect those of COFORD. i CONTENTS Foreword..................................................................................................................v Réamhfhocal...........................................................................................................vi Preface ....................................................................................................................vii Réamhrá................................................................................................................viii Acknowledgements...............................................................................................ix