Analyzing Differences Among Basic Health Units Efficiency in Sargodha
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sargodha District Sargodha
DISTRICT DISASTER MANAGEMENT PLAN 2020 DIVISION SARGODHA DISTRICT SARGODHA IDP Camp in 2009 Earthquake Flood Mock Exercise in May 2020 Corona virus Pandemic-Training to wear PPE’s Prepared by: MAZHAR SHAH, DISTRICT EMERGENCY OFFICER Approved by: DDMA Sargodha DDMP 2020 TABLE OF CONTENTS Executive Summary .................................................................................................................................................... 1 Aim and Objectives ..................................................................................................................................................... 2 District Profile .............................................................................................................................................................. 3 Coordination Mechanism ............................................................................................................................................ 9 Risk Analysis............................................................................................................................................................ 19 Mitigation Strategy ................................................................................................................................................... 25 Early Warning .......................................................................................................................................................... 28 Rescue Strategy ..................................................................................................................................................... -

Ethnomedicinal Recipes of Wild Fruits of Sargodha District, Punjab, Pakistan
J. Bio. & Env. Sci. 2019 Journal of Biodiversity and Environmental Sciences (JBES) ISSN: 2220-6663 (Print) 2222-3045 (Online) Vol. 14, No. 6, p. 262-271, 2019 http://www.innspub.net RESEARCH PAPER OPEN ACCESS Ethnomedicinal recipes of wild fruits of Sargodha District, Punjab, Pakistan Asif Abbas Shah1, Amin Shah1, Muhammad Nadeem2, Sarvat Rahim*1 1Department of Botany, University of Sargodha, Sargodha, Pakistan 2Institute of Food Science and Nutrition, University of Sargodha, Sargodha, Pakistan Article published on June 30, 2019 Key words: Wild fruit, Indigenous communities, Folklore, Curative flora. Abstract The The present study was conducted in the Sargodha district, Punjab, to underline indigenous knowledge of wild edible fruits as for therapeutic use by the local inhabitants. Folklore traditions with respect to curative flora were gathered through meetings and surveys from key informants including local residents, shepherds, herders, ranchers, traditional healers and herbalists. Rural vicinities were engaged to investigate reliable clients of wild edible fruits. Such studies not just assume a significant role in saving the native medica-ethnobotanical information yet in addition help to update the social status and economic values of the indigenous communities that consequently preserve the global heritage. 27 fruit species belonging to 15 families were recorded in the territory. All the plants were extremely compelling against various diseases and native to the area. The data about their botanical names, local names, families, part used, method of use and used for, all were recorded. The fruits and other plant samples of the investigated plants were collected, identified, preserved and deposited in the Herbarium of University of Sargodha (SARGU) for future references. -

Audit Report on the Accounts of Tehsil Municipal Administrations District Sargodha
AUDIT REPORT ON THE ACCOUNTS OF TEHSIL MUNICIPAL ADMINISTRATIONS DISTRICT SARGODHA AUDIT YEAR 2015-16 AUDITOR GENERAL OF PAKISTAN TABLE OF CONTENTS ABBREVIATIONS & ACRONYMS ..................................................... i PREFACE .............................................................................................. ii EXECUTIVE SUMMARY ................................................................... iii SUMMARY TABLES AND CHARTS................................................ vii Table 1: Audit Work Statistics ............................................................... vii Table 2: Audit Observations regarding Financial Management ............... vii Table 3: Outcome Statistics ................................................................... viii Table 4: Irregularities Pointed Out ........................................................ viii Table 5: Cost-Benefit ............................................................................ viii CHAPTER-1 .......................................................................................... 1 1.1 TEHSIL MUNICIPAL ADMINISTRATIONS, DISTRICT SARGODHA .......................................................................................... 1 1.1.1 Introduction ................................................................................. 1 1.1.2 Comments on Budget and Accounts (Variance Analysis).............. 2 1.1.3 Brief Comments on the Status of Compliance on MFDAC Paras of Audit Year 2014-15 ..................................................................... -

Field Appraisal Report Tma Sillanwali
FIELD APPRAISAL REPORT TMA SILLANWALI Prepared by; Punjab Municipal Development Fund Company December-2008 TABLE OF CONTENTS 1. INSTITUTIONAL DEVELOPMENT 1.1 BACKGROUND 2 1.2 METHODOLOGY 2 1.3 DISTRICT PROFILE 2 1.3.1 History 2 1.3.2 Location 2 1.3.3 Area/Demography 2 1.4 TMA/TOWN PROFILE 3 1.4.1 TMA Status 3 1.4.2 Location 3 1.4.3 Area / Demography 3 1.5 TMA STAFF PROFILE 3 1.6 INSTITUTIONAL ASSESSMENT 4 1.6.1 Tehsil Nazim 4 1.6.2 Office of Tehsil Municipal Officer 4 1.7 TEHSIL OFFICER (Planning) OFFICE 8 1.8 TEHSIL OFFICER (Regulation) OFFICE 10 1.9 TEHSIL OFFICER (Finance) OFFICE 11 1.10 TEHSIL OFFICER (Infrastructure & Services) OFFICE 15 2. INFRASTRUCTURE DEVELOPMENT 2.1 ROADS 17 2.2 STREET LIGHTS 17 2.3 WATER SUPPLY 17 2.4 SEWERAGE 18 2.5 SOLID WASTE MANAGEMENT 18 2.6 FIRE FIGHTING 18 2.7 PARKS 19 1 1. INSTITUTIONAL DEVELOPMENT 1.1 BACKGROUND TMA Sillanwali has applied for funding under PMSIP. After initial desk appraisal, PMDFC field team visited the TMA for assessing its institutional and engineering capacity. 1.2 METHODOLOGY Appraisal is based on interviews with TMA staff, open-ended and close-ended questionnaires and agency record. Debriefing sessions and discussions were held with Tehsil Nazim, TMO, TOs and other TMA staff. 1.3 DISTRICT PROFILE 1.3.1 History The district derives its name from the headquarters town of Sargodha, which is a combination of the words „Sar‟ and „Godha‟. Sar, a Hindi word means a water pond while “Godha” was the name of the Hindi Faqir who lived near that pond. -

District SARGODHA Tehsil Group Batch No. Frist Name Last Name
District SARGODHA Tehsil Group Batch No. Frist Name Last Name Gender Teacher Type Cell No. Email EMIS Code School Name BHALWAL Arts Batch 1 Aamir Hayat Male Public 3016946997 [email protected] 38410151 GPS SULTAN PUR NOON BHALWAL Arts Batch 1 Aasia Sultan Female Public 3044644508 [email protected] 38410042 GGHSS LALLIANI BHALWAL Arts Batch 1 Aasma Javed Female Public 3069607018 [email protected] 38410503 GGES CHAK NO.16 NB BHALWAL Arts Batch 1 Abdur Rehman Male Public 3075332038 [email protected] 38410013 GHS CHAK NO.22 NB BHALWAL Arts Batch 1 Abida Mumtaz Female Public 3474800449 [email protected] 38410040 GGHSS CHAK NO.10 ML BHALWAL Arts Batch 1 Abida Naseem Female Private 0303-4247331 [email protected] 384107406 GHAZALI MODEL HIGH SCHOOL BOYS PHULARWAN BHALWAL Arts Batch 1 Abida Rani Female Public 3447475290 [email protected] 38410068 GES PHULARWAN BHALWAL Arts Batch 1 Abida Tasneem Female Public 3434346283 [email protected] 38410187 GMPS CHAK NO.14 SB PATHAN WALA BHALWAL Arts Batch 1 Adeeba Javaid Female Public 3414300718 [email protected] 38410331 GMPS PHULARWAN KOHNA BHALWAL Arts Batch 1 Adeela Nawaz Female Private 0301-6792573 [email protected] other other BHALWAL Arts Batch 1 Afsana Kanwal Female Public 3327546064 [email protected] 38410681 GGPS AHLI DAKHLI 4 NB BHALWAL Arts Batch 1 Afshan Batool Female Public 3417977817 [email protected] 38410505 GGPS DERA BACHIAN WALA BHALWAL Arts Batch 1 Afshan Noreen Female Private 0306-8604984 [email protected] -

SARGODHA-Reg4d5.Pdf
New Registration List S/NO REG# / NAME FATHER'S NAME PRESENT ADDRESS DATE OF ACADEMIC REG BIRTH QUALIFICATION DATE 1 143736 FARAH BATOOL JAWAD HUSSAIN H NO 641 BLOCK A MOHALLAH SATTELITE 5/12/1964 MATRIC 28/8/2014 TOWN SARGHODA, SARGODHA, PUNJAB 2 143737 ASIFA RAM RANA MUHAMMAD RUND RONI KAMRI GATE NOORI MASJID 3/3/1987 MATRIC 28/8/2014 IQBAL SAHIWAL , SARGODHA, PUNJAB 3 143773 MUHAMMAD MUHAMMAD ASHRAF OLD CIVIL LINES H NO 349 ST 2 QASIM PURA 24/4/1985 MATRIC 29/8/2014 TARIQ , SARGODHA, PUNJAB 4 143802 MUHAMMAD AHMAD KHAN MOHALLAH QUDARTABAD ST 11 NEAR 11/10/1990 FA 2/9/2014 GHAFOOR SHAHEEN CHOK SARGODH, SARGODHA, AHMAD Q PUNJAB 5 143875 TARIQ MUHAMMAD SADIQ ST 18 MOHALLAH SULMAN PURA 5/4/1976 MATRIC 4/9/2014 MEHMOOD BHALWALDISTT SARGHDA , SARGODHA, PUNJAB 6 144023 MUHAMMAD MUHAMMAD GALI NO 2 MOHALLAH MUSTAFABADFAROKA 15/9/1970 MATRIC 10/11/2014 MAQSOOD SHAH SIDDIQUE SHAH ROAD DISTT , SARGODHA, PUNJAB 7 147572 AMJID FAROOQ MUHAMMAD SADIQ KOT SHER KHAN CHAK 20 SB TEH KOT 13/8/1982 MATRIC 21/1/2015 MUMIN DISTT, SARGODHA, PUNJAB 8 144334 SAMINA ANJUM ISLAM DIN BHERA BHALWAL DISTT , SARGODHA, 1/4/1978 MATRIC 4/2/2015 PUNJAB 9 144431 HAFIZ BILAL HAFIZ MUHAMMAD VILLAGE VARIGOWAL DHARAIMA 1/4/1976 MATRIC 12/3/2015 AHMAD AZEEM TEHSHAHPUR, SARGODHA, PUNJAB 10 144473 GHULAM KHADIM HUSSAIN H NO 164 ST E 2 MOH NEW SATTELITE TOWN 4/4/1987 MATRIIC 17/3/2015 HUSSAIN BLOK 2 , SARGODHA, PUNJAB 11 144561 MUHAMMAD MUHAMMAD ASLAM FALEON WELFAIR HOSPITAL CHAWAYWAL 1/1/1982 MATRIC 19/3/2015 ASHRAF ATEH TEH SAHIWAL DISTT, SARGODHA, PUNJAB 12 144662 SANILA ZAFAR ZAFAR HUSSAIN GALI NO. -
(Iswm) in Sahiwal-Sargodha Pasrur
Sahiwal-Sargodha [Type text] SITUATION ANALYSIS REPORT FOR INTEGRATED SOLID WASTE MANAGEMENT (ISWM) IN SAHIWAL-SARGODHA PASRUR TABLE OF CONTENTS 1.0 INTRODUCTION 1.1 Objective ………………………………………………….. 1 1.2 Background ………………………………………………. 1 1.3 Scope of the Assignment .………………………………. 2 1.4 Approach & Methodology ………………………………... 2 2.0 General Description of City 2.1 Location …………………………………………..………... 4 2.2 General Information …………………………………..…... 4 2.3 Population …………………………………..…................... 4 3.0 SITUATION ANALYSIS 3.1 Solid Waste Generation ………………………………….. 6 3.2 Primary Collection ………………………………………… 7 3.3 Secondary Collection …………………………………….. 8 3.4 Final Disposal ……………………………………………… 9 3.5 Safety and Environment ………………………………….. 10 3.6 Operation & Maintenance ……………………………….. 11 3.7 Financial Analysis ………………………………………….. 12 3.8 Human Resource Management …………………………… 13 3.9 Citizen Complaints Registration & Resolution …………… 14 3.10 General Public Opinion …………………………………….. 16 4.0 RECOMMENDATIONAS & WAY FORWARD ………………………….. 18 ANNEXURE – I SWM GIS Map 2 SOLID WASTE MANAGEMENT – SAHIWAL-SARGODHA SOLID WASTE MANAGEMENT – INTRODUCTION 1.1 Objective Punjab Chief Minister Mian Shahbaz Sharif is very conscious about the proper solid waste management system and is keen to see "litter free Punjab" in the forthcoming years. In this connection, the Government of Punjab is going to implement a solid waste management initiative in certain group of TMAs. The Purpose of this initiative is to develop effective solid waste management plans for TMAs which have adequate machinery to a certain extent. In the regard, it has been decided to gather the information regarding resource availability with TMAs for conducting detailed situation analysis in solid waste management sector. 1.2 Background Solid Waste Management is a major environment and health hazard in the urban areas of Pakistan. -
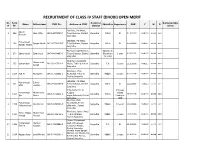
(Dhobi) Open Merit
RECRUITMENT OF CLASS-IV STAFF (DHOBI) OPEN MERIT Sr. Form Domicile/ Remarks/Obje Name Father name CNIC No. Address on CNIC Education Experience DOB Y M D # No District ctions Jala Bala, PO Khass, Aqeed 1 264 Allah Ditta 38402-9979330-7 Tehsil Sahiwal, District Sargodha Matric Nil 01.10.2002 #VALUE! #### ### Hussain Sargodha Jala Bala, PO Khass, Muhammad 2 258 Faryad Masih 38404-7732209-7 Tehsil Sahiwal, District Sargodha Matric Nil 05.04.1999 #VALUE! #### ### Rizwan Haider Sargodha PO Khass Aqil Shahpur, Diploma in 3 207 Samar Iqbal Zafar Iqbal 38404-4834890-3 Tehsil Shahpur, District Sargodha Electrician 1 year 01.05.1992 #VALUE! #### ### Sargodha 02 years Chak No.102/S.B,PO Muhammad 4 232 Usman Gani 38403-1107314-1 Khass, Tehsil & District Sargodha F.A 3 years 11.11.1996 #VALUE! #### ### Ashraf Sargodha PO Khass, Chak 5 1334 Asif Ali Ahmad Ali 38403-7036592-1 No.51/NB, Tehsil & Sargodha Middle 5 years 01.01.1996 #VALUE! #### ### District Sargodha Jala Bala, PO Khass, Muhammad Zahoor 6 261 38402-5856653-9 Tehsil Sahiwal, District Sargodha Matric Nil 02.04.1995 #VALUE! #### ### Irfan Hussain Sargodha H No.6/15-7/7, St 2.5 years Muhammad Muhammad A,Islam Crystal 7 1355 38405-8718402-5 Sargodha Matric 26.06.1996 #VALUE! #### ### Ijaz Akram nagar,Sillanwali, District Landry in Sargodha UAE PO Khas, Chak Muhammad No.135/SB, Teshil 8 1359 Mukhtar Ali 38405-0895861-5 Sargodha Middle 1.5 years 15.03.1999 #VALUE! #### ### Mahran Faisal Sillanwali , District Sargodha PO Khass, Jahan Abad Prince Waqas Muhammad 9 1317 38404-1766726-5 , Tehsil Shahpur, Sargodha Middle 5 years 19.05.2000 #VALUE! #### ### Ahmad Ahmad District Sargodha Channi Muhammad Muhammad Manzoor Qazi, PO Lakseen, 10 1398 38401-3989998-3 Sargodha F.A Nil 30.12.1995 #VALUE! #### ### Farooq Hussain Tehsil Kot Momin, District Sargodha Mohalla Imam Bargah Markazi, Kot Momin, PO 11 1416 Hassan Raza Syed Ahmad 38406-0489385-7 Sargodha Middle 3 years 05.10.1995 #VALUE! #### ### & Tehsil Kot Momin, District Sargodha Sr. -

A Look at the Spatial Inequality in Pakistan:Case Study of District Sargodha
UC Santa Cruz Mapping Global Inequalities Title A look at the Spatial Inequality in Pakistan:Case study of District Sargodha Permalink https://escholarship.org/uc/item/4hd5n6pr Author Ali Asjad Naqvi, Syed Publication Date 2007-12-04 eScholarship.org Powered by the California Digital Library University of California A look at the Spatial Inequality in Pakistan: Case study of District Sargodha Working paper submitted for the conference on Mapping Global Inequalities - Beyond Income Inequality University of California, Santa Cruz Second Draft: 4th December, 2007 Syed Ali Asjad Naqvi1 New School for Social Research 1 Currently enrolled in the first year Ph.D. Economics program at New School for Social Research (New York). A large part of the information was collected while working at Lahore University of Management Sciences (LUMS), Pakistan as a Research Fellow/Data Coordinator in the Economics Department (2005- 2007). Please send comments and feedback at [email protected]) 1 Acknowledgements This paper draws heavily on the research work conducted by Dr. Ali Cheema (Associate Professor and Head of Economics Department, LUMS) and Shandana Khan Mohmand (Teaching Fellow, Social Sciences Department) on the District of Sargodha in the past three years. Dr. Ali Cheema has been a constant source of inspiration throughout my research career at LUMS and has been an integral part for developing the research framework for the overall project. This paper would not have been possible without his support. I would like to acknowledge funding support received from the DRC on the Future State, Institute of Development Studies, University of Sussex; CIDA funded LUMS-McGill Social Enterprise Development Centre; and the Punjab Planning and Development Department for the “LUMS Sargodha Informal Institutions Project”. -

Annual Minimum Temperature Variations in Early 21St Century in Punjab, Pakistan
Journal of Atmospheric and Solar-Terrestrial Physics 137 (2016) 1–9 Contents lists available at ScienceDirect Journal of Atmospheric and Solar-Terrestrial Physics journal homepage: www.elsevier.com/locate/jastp Annual minimum temperature variations in early 21st century in Punjab, Pakistan Misbah Jahangir n, Syeda Maria Ali, Bushra Khalid Department of Environmental Science, International Islamic University Islamabad, Pakistan article info abstract Article history: Climate change is a key emerging threat to the global environment. It imposes long lasting impacts both Received 19 August 2015 at regional and national level. In the recent era, global warming and extreme temperatures have drawn Received in revised form great interest to the scientific community. As in a past century considerable increase in global surface 26 October 2015 temperatures have been observed and predictions revealed that it will continue in the future. In this Accepted 29 October 2015 regard, current study mainly focused on analysis of regional climatic change (annual minimum tem- Available online 30 October 2015 perature trends and its correlation with land surface temperatures in the early 21st century in Punjab) for Keywords: a period of 1979–2013. The projected model data European Centre for Medium-Range Weather Forecasts Minimum temperature (ECMWF) Re-Analysis (ERA-Interim) has been used for eight Tehsils of Punjab i.e., annual minimum Land surface temperature temperatures and annual seasonal temperatures. Trend analysis of annual minimum and annual seasonal Landsat temperature in (Khushab, Noorpur, Sargodha, Bhalwal, Sahiwal, Shahpur, Sillanwali and Chinoit) tehsils Punjab – Pakistan of Punjab was carried out by Regression analysis and Mann Kendall test. Landsat 5 Thematic Mapper (TM) data was used in comparison with Model data for the month of May from the years 2000, 2009 and 2010. -

Mali Sargodha District.Pdf
1 LIST OF CANDIDATES FOR THE POST OF MALI DISTRICT SARGODHA APPLICATI AGE AS ON Mark Mark Total NEW SR. NO. FORM NO. NAME FATHER NAME GENDER RELEG: CNIC NO. DOB 7 Apr 2021 ADDRESS DOMICILE DISTRICT EDU: MOB NO QUOTA EXPERIENCE DOCUMENT STATUS REMARKS Merit ON ID NO. Y M D Obtain Obtain Marks 1 1 98 M. Riaz Male Islam 38403-8185100-5 9-Apr-01 19 11 28 Faisal Town, Streeet No. 4 Sargodha Sargodha Matric Open Nil REJECTED Affidavit & Experience Not ed in ed in M. Zeeshan 0301-1478924 Attached Test Intervi 2 2 49 M. Riaz Male Islam 38403-9309144-3 26-Sep-98 22 6 11 Chak No. 53, Janoobi Sargodha Sargodha Matric Open Nil REJECTED Affidavit & Experience Not Mohsin Riaz ew 0343-8012791 Attached 3 3 50 M. Ramzan Male Islam 38402-0120365-1 28-Feb-93 28 1 9 Asar Sarkharo, P.O Dharwal, Sargodha Sargodha Matric Open Nil REJECTED Affidavit & Experience Not M. Shakeel 0304-9120648 Attached 4 4 61 Akram Masih Male Christian 38403-5606473-5 10-Jan-00 21 2 27 Chak No. 43, Giyanwala P.O Sargodha Sargodha Middle Open Nil REJECTED Affidavit & Experience Not Shehroon Masih Nil Attached 5 5 80 Nasir Hameed Male Islam 38403-7925256-1 25-Aug-98 22 7 12 House No. 9, P.T.S Sargodha Sargodha Middle Open Nil REJECTED Affidavit & Experience Not Sheraz Baloch 0308-1209491 Attached 6 6 104 M.aslam Male Islam 38403-7222978-5 22-Oct-00 20 5 15 Johar Colony House no. 2 Mohallah Sargodha Matric Open Nil REJECTED Affidavit & Experience Not M. -

Government of the Punjab Primary & Secondary
GOVERNMENT OF THE PUNJAB PRIMARY & SECONDARY HEALTHCARE DEPARTMENT Dated Lahore, the 11th, August 2021 O R D E R No.SO(North)5-6/2021(Adhoc Sargodha), The following doctors are hereby appointed as Medical Officers (BS-17) on adhoc basis and posted at place mentioned against their names with immediate effect, for a period of one year or till the availability of regular incumbents/selectees of the Punjab Public Service Commission, whichever is earlier: - Sr. No. Name of candidate Place of posting 1. Dr. Ali Ameer S/O Abdul Majeed BHU Mela 2. Dr. Hafiz Ijaz Ali S/O Faryad Ali BHU Koray Kot 3. Dr. Ansar Ali S/O Khizer Hayat BHU Jalal Pur Jadeed 4. Dr. Zeeshan Zafar S/O Zafar Iqbal BHU Talibwala Dr. Hafiz Aaqib Mehboob S/O Mehboob Elahi 5. BHU 147-148/NB Akhtar Dr. Shah Hasan Waseem S/O Syed Waseem 6. BHU 131/SB Jafri Dr. Muhammad Imran Khan S/O Muhammad 7. BHU Chak Mubarik Nawaz Khan Dr. Abdul Wahab Nawaz S/O Muhammad 8. BHU Hazoor Pur Nawaz 9. Dr. Ammad Mazhar S/O Mazhar Rashid BHU Hathiwind 10. Dr. Zahoor Ahmed S/O Noor Ahmed BHU 15/SB 11. Dr. Muhammad Muzamil S/O Makhdoomzada BHU 10/NB Powered by: Health Information and Service Delivery Unit (HISDU) 12. Dr Ahmad Ilyas S/O Ilyas Anjum BHU Havali Majoka Dr. Muhammad Sabeen Ahsan S/O Ghulam 13. BHU Jhania Shah Hussain 14. Dr. Muhammad Shah Zaib S/O Khalid Yousaf RHC 71/SB 15. Dr. Saad Masood S/O Masood Ahmad RHC 104/NB 16.