Anatomy of the Knee and Lower Leg
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

June 3, 2016 Karen B. Desalvo, M.D., M.P.H., M.Sc. Acting Assistant
June 3, 2016 Karen B. DeSalvo, M.D., M.P.H., M.Sc. Acting Assistant Secretary Department of Health and Human Services Office of the National Coordinator for Health Information Technology Attention: RFI Regarding Assessing Interoperability for MACRA 330 C Street, SW, Room 7025A Washington, DC 20201 Subject: Office of the National Coordinator for Health Information Technology; Medicare Access and CHIP Reauthorization Act of 2015; Request for Information Regarding Assessing Interoperability for MACRA Dear Acting Assistant Secretary DeSalvo: The American Association of Orthopaedic Surgeons (AAOS) and orthopaedic specialty societies, representing over 18,000 board-certified orthopaedic surgeons, appreciate the opportunity to provide comments on the Request for Information Regarding Assessing Interoperability for MACRA by the Office of the National Coordinator (ONC) for Health Information Technology, and published in the Federal Register on April 8, 2016. The AAOS has been committed to working with ONC in the adoption of electronic health records. As surgical specialists, we have unique Health Information Technology (HIT) needs and respectfully offer some suggestions to improve interoperability to better reflect the needs of our surgical specialists and their patients and accelerate HIT adoption in the future by orthopaedic surgeons. The AAOS thanks ONC in advance for its solicitation and consideration of the following comments and concerns. We have structured our comments in the order that ONC is soliciting public feedback in the RFI document referenced above. Scope of Measurement: Defining Interoperability and Population The focus of measurement should not be limited to “meaningful Electronic Health Records (EHR) users,” as defined (e.g., eligible professionals, eligible hospitals, and CAHs that attest to meaningful use of certified EHR technology under CMS’ Medicare and Medicaid EHR Incentive Programs), and their exchange partners. -
Bones of the Upper and Lower Limb
Bones of the Upper and Lower limb Musculoskeletal block- Anatomy-lecture 1 Editing file Objectives Color guide : important in Red ✓ Classify the bones of the three regions of the lower Doctor note in Green limb (thigh, leg and foot). Extra information in Grey ✓ Memorize the main features of the – Bones of the thigh (femur & patella) – Bones of the leg (tibia & Fibula) – Bones of the foot (tarsals, metatarsals and phalanges) ✓ Recognize the side of the bone. Note: this lecture is based on female slides since Prof abuel makarem said only things that are mentioned in the female slides will come in the exam Note : All bones picture which are described in this lecture are bones on the right side of the body Before start :Please make yourself familiar with these terms to better understand the lecture Terms Meaning Example Ridge The long and narrow upper edge, angle, or crest The supracondylar ridges (in the distal part of of something (the humerus The trochlear notch (in the proximal part of the Notch An indentation, (incision) on an edge or surface (ulna A nodule or a small rounded projection on the Tubercles (Dorsal tubercle (in the distal part of the radius bone A hollow place (The Notch is not complete but the Subscapular fossa (in the concave part of the Fossa fossa is complete and both of them act as the lock (scapula (of the joint A large prominence on a bone usually serving for Deltoid tuberosity (in the humorous) and it Tuberosity the attachment of muscles or ligaments (is a connects the deltoid muscle (bigger projection than the Tubercle -

General Introduction of Anatomy
ﺍﳌﻌﻬﺪ ﺍﻟﻄﺒﻲ ﺍﻟﺘﻘﻨﻲ / ﺑﻐﺪﺍﺩ ﻗﺴﻢ ﺍﻟﺘﺄﻫﻴﻞ ﺍﻟﻄﺒﻲ ﻭﺍﻟﻌﻼﺝ ﺍﻟﻄﺒﻴﻌﻲ ﻓﺮﻉ ﺻﻨﺎﻋﺔ ﺍﻻﻃﺮﺍﻑ ﻭﺍﳌﺴﺎﻧﺪ General introduction of Anatomy 2013 – 2014 Dr. ASHRAF Ali AL-ZUBAIDI Dr. ASHRAF Ali AL-ZUBAIDI 2013-2014 1 GENERAL INTRODUCTION Anatomy: is the science of body structures and the relationships among Structures. At first the anatomy was studied by dissection, the carful cutting apart of body structures to study their relationships, Nowadays, many imaging of anatomical (ﺗﻘﺪم) to the advancement (ﺗﺴﺎھﻢ) techniques also contribute knowledge. The Anatomy is including many of fields, which is: It is the study of different : (اﻟﻔﺤﺺ اﻟﻌﯿﻨﻲ ) Macroscopic examination 1- structures , which make up the human body . It is the study of : (اﻟﻔﺤﺺ اﻟﻤﺠﮭﺮي ) Microscopic examination 2- seen (اﻟﻜﺎﺋﻦ اﻟﺤﻲ ) microscopic different structures of an organism only by use of a microscope . It is the study of different structures as : (اﻻﺟﮭﺰة اﻟﺠﺴﻤﯿﺔ) Systemic 3- : It comprises of the followings . (ﻛﻜﯿﺎﻧﺎت ﻓﺮدﯾﺔ) individual entities .The bony system \ ( ﻋﻠﻢ اﻟﻌﻈﺎم ) Osteology • . The articular system or joint \(ﻋﻠﻢ اﻟﻤﻔﺎﺻﻞ ) Syndesmology • . The muscular system \ (ﻋﻠﻢ الﻋﻀﻼت )Myology • , Comprising the heart , blood vessels \ (ﻋﻠﻢ اﻻوﻋﯿﺔ ) Angiology • ( اﻟﻌﻘﺪ اﻟﻠﻤﻔﺎوﯾﺔ)lymph nodes & (اﻻوﻋﯿﺔ اﻟﻠﻤﻔﺎوﯾﺔ) lymph vessels .The nervous system \(ﻋﻠﻢ اﻟﺠﮭﺎز اﻟﻌﺼﺒﻲ) Neurology • , ( اﻟﻨﻈﺎم اﻟﺤﺸﻮي ) The visceral system \ (ﻋﻠﻢ اﻻﺣﺸﺎء) Splanchnology • , (ﻧﻈﺎم اﻧﺒﻮﺑﻲ – ھﻀﻤﻲ ) comprising two tubular system – digestive . (اﻟﺠﮭﺎز اﻟﺘﻨﺎﺳﻠﻲ) and genital (اﻟﺠﮭﺎز اﻟﺒﻮﻟﻲ) urinary tract The study of form and marking of those :(اﻟﺘﺸﺮﯾﺢ اﻟﺴﻄﺤﻲ) Surface 4- structures by examination through skin. .It is the study of development before birth :(ﻋﻠﻢ اﻻﺟﻨﺔ) Embryology 5- GLOSSARY OF ANATOMIC TERMINOLOGY description of location (ﯾﺴﻤﺢ) Reference position of body permitting and movements: 1- Term of Anatomical position: • Head ………. -

Compression Garments for Leg Lymphoedema
Compression garments for leg lymphoedema You have been fitted with a compression garment to help reduce the lymphoedema in your leg. Compression stockings work by limiting the amount of fluid building up in your leg. They provide firm support, enabling the muscles to pump fluid away more effectively. They provide most pressure at the foot and less at the top of the leg so fluid is pushed out of the limb where it will drain away more easily. How do I wear it? • Wear your garment every day to control the swelling in your leg. • Put your garment on as soon as possible after getting up in the morning. This is because as soon as you stand up and start to move around extra fluid goes into your leg and it begins to swell. • Take the garment off before bedtime unless otherwise instructed by your therapist. We appreciate that in hot weather garments can be uncomfortable, but unfortunately this is when it is important to wear it as the heat can increase the swelling. If you would like to leave off your garment for a special occasion please ask the clinic for advice. What should I look out for? Your garment should feel firm but not uncomfortable: • If you notice the garment is rubbing or cutting in, adjust the garment or remove it and reapply it. • If your garment feels tight during the day, try and think about what may have caused this. If you have been busy, sit down and elevate your leg and rest for at least 30 minutes. -

Sports Ankle Injuries Assessment and Management
FOCUS Sports injuries Sports ankle injuries Drew Slimmon Peter Brukner Assessment and management Background Case study Lucia is a female, 16 years of age, who plays netball with the Sports ankle injuries present commonly in the general state under 17s netball team. She presents with an ankle injury practice setting. The majority of these injuries are inversion sustained at training the previous night. She is on crutches and plantar flexion injuries that result in damage to the and is nonweight bearing. Examination raises the possibility of lateral ligament complex. a fracture, but X-ray is negative. You diagnose a severe lateral Objective ligament sprain and manage Lucia with ice, a compression The aim of this article is to review the assessment and bandage and a backslab initially. She then progresses through management of sports ankle injuries in the general practice a 6 week rehabilitation program and you recommend she wear setting. an ankle brace for at least 6 months. Discussion Assessment of an ankle injury begins with a detailed history to determine the severity, mechanism and velocity of the injury, what happened immediately after and whether there is a past history of inadequately rehabilitated ankle injury. Examination involves assessment of weight bearing, inspection, palpation, movement, and application of special examination tests. Plain X-rays may be helpful to exclude a fracture. If the diagnosis is uncertain, consider second The majority of ankle injuries are inversion and plantar line investigations including bone scan, computerised flexion injuries that result in damage to the lateral tomography or magnetic resonance imaging, and referral to a ligament complex (Figure 1). -
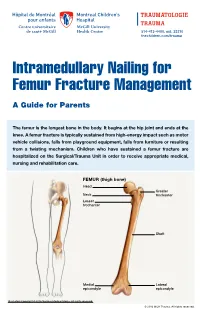
Intramedullary Nailing for Femur Fracture Management a Guide for Parents
514-412-4400, ext. 23310 thechildren.com/trauma Intramedullary Nailing for Femur Fracture Management A Guide for Parents The femur is the longest bone in the body. It begins at the hip joint and ends at the knee. A femur fracture is typically sustained from high-energy impact such as motor vehicle collisions, falls from playground equipment, falls from furniture or resulting from a twisting mechanism. Children who have sustained a femur fracture are hospitalized on the Surgical/Trauma Unit in order to receive appropriate medical, nursing and rehabilitation care. FEMUR (thigh bone) Head Greater Neck trochanter Lesser trochanter Shaft Medial Lateral epicondyle epicondyle Illustration Copyright © 2016 Nucleus Medical Media, All rights reserved. © 2016 MCH Trauma. All rights reserved. FEMUR FRACTURE MANAGEMENT The pediatric Orthopedic Surgeon will assess your child in order to determine the optimal treatment method. Treatment goals include: achieving proper bone realignment, rapid healing, and the return to normal daily activities. The treatment method chosen is primarily based on the child’s age but also taken into consideration are: fracture type, location and other injuries sustained if applicable. Prior to the surgery, your child may be placed in skin traction. This will ensure the bone is in an optimal healing position until it is surgically repaired. Occasionally, traction may be used for a longer period of time. The surgeon will determine if this management is needed based on the specific fracture type and/or location. ELASTIC/FLEXIBLE INTRAMEDULLARY NAILING This surgery is performed by the Orthopedic Surgeon in the Operating Room under general anesthesia. The surgeon will usually make two small incisions near the knee joint in order to insert two flexible titanium rods (intramedullary nails) Flexible through the femur. -

ANTERIOR KNEE PAIN Home Exercises
ANTERIOR KNEE PAIN Home Exercises Anterior knee pain is pain that occurs at the front and center of the knee. It can be caused by many different problems, including: • Weak or overused muscles • Chondromalacia of the patella (softening and breakdown of the cartilage on the underside of the kneecap) • Inflammations and tendon injury (bursitis, tendonitis) • Loose ligaments with instability of the kneecap • Articular cartilage damage (chondromalacia patella) • Swelling due to fluid buildup in the knee joint • An overload of the extensor mechanism of the knee with or without malalignment of the patella You may feel pain after exercising or when you sit too long. The pain may be a nagging ache or an occasional sharp twinge. Because the pain is around the front of your knee, treatment has traditionally focused on the knee itself and may include taping or bracing the kneecap, or patel- la, and/ or strengthening the thigh muscle—the quadriceps—that helps control your kneecap to improve the contact area between the kneecap and the thigh bone, or femur, beneath it. Howev- er, recent evidence suggests that strengthening your hip and core muscles can also help. The control of your knee from side to side comes from the glutes and core control; that is why those areas are so important in management of anterior knee pain. The exercises below will work on a combination of flexibility and strength of your knee, hip, and core. Although some soreness with exercise is expected, we do not want any sharp pain–pain that gets worse with each rep of an exercise or any increased soreness for more than 24 hours. -
How to Self-Bandage Your Leg(S) and Feet to Reduce Lymphedema (Swelling)
Form: D-8519 How to Self-Bandage Your Leg(s) and Feet to Reduce Lymphedema (Swelling) For patients with lower body lymphedema who have had treatment for cancer, including: • Removal of lymph nodes in the pelvis • Removal of lymph nodes in the groin, or • Radiation to the pelvis Read this resource to learn: • Who needs self-bandaging • Why self-bandaging is important • How to do self-bandaging Disclaimer: This pamphlet is for patients with lymphedema. It is a guide to help patients manage leg swelling with bandages. It is only to be used after the patient has been taught bandaging by a clinician at the Cancer Rehabilitation and Survivorship (CRS) Clinic at Princess Margaret Cancer Centre. Do not self-bandage if you have an infection in your abdomen, leg(s) or feet. Signs of an infection may include: • Swelling in these areas and redness of the skin (this redness can quickly spread) • Pain in your leg(s) or feet • Tenderness and/or warmth in your leg(s) or feet • Fever, chills or feeling unwell If you have an infection or think you have an infection, go to: • Your Family Doctor • Walk-in Clinic • Urgent Care Clinic If no Walk-in clinic is open, go to the closest hospital Emergency Department. 2 What is the lymphatic system? Your lymphatic system removes extra fluid and waste from your body. It plays an important role in how your immune system works. Your lymphatic system is made up of lymph nodes that are linked by lymph vessels. Your lymph nodes are bean-shaped organs that are found all over your body. -

Parts of the Body 1) Head – Caput, Capitus 2) Skull- Cranium Cephalic- Toward the Skull Caudal- Toward the Tail Rostral- Toward the Nose 3) Collum (Pl
BIO 3330 Advanced Human Cadaver Anatomy Instructor: Dr. Jeff Simpson Department of Biology Metropolitan State College of Denver 1 PARTS OF THE BODY 1) HEAD – CAPUT, CAPITUS 2) SKULL- CRANIUM CEPHALIC- TOWARD THE SKULL CAUDAL- TOWARD THE TAIL ROSTRAL- TOWARD THE NOSE 3) COLLUM (PL. COLLI), CERVIX 4) TRUNK- THORAX, CHEST 5) ABDOMEN- AREA BETWEEN THE DIAPHRAGM AND THE HIP BONES 6) PELVIS- AREA BETWEEN OS COXAS EXTREMITIES -UPPER 1) SHOULDER GIRDLE - SCAPULA, CLAVICLE 2) BRACHIUM - ARM 3) ANTEBRACHIUM -FOREARM 4) CUBITAL FOSSA 6) METACARPALS 7) PHALANGES 2 Lower Extremities Pelvis Os Coxae (2) Inominant Bones Sacrum Coccyx Terms of Position and Direction Anatomical Position Body Erect, head, eyes and toes facing forward. Limbs at side, palms facing forward Anterior-ventral Posterior-dorsal Superficial Deep Internal/external Vertical & horizontal- refer to the body in the standing position Lateral/ medial Superior/inferior Ipsilateral Contralateral Planes of the Body Median-cuts the body into left and right halves Sagittal- parallel to median Frontal (Coronal)- divides the body into front and back halves 3 Horizontal(transverse)- cuts the body into upper and lower portions Positions of the Body Proximal Distal Limbs Radial Ulnar Tibial Fibular Foot Dorsum Plantar Hallicus HAND Dorsum- back of hand Palmar (volar)- palm side Pollicus Index finger Middle finger Ring finger Pinky finger TERMS OF MOVEMENT 1) FLEXION: DECREASE ANGLE BETWEEN TWO BONES OF A JOINT 2) EXTENSION: INCREASE ANGLE BETWEEN TWO BONES OF A JOINT 3) ADDUCTION: TOWARDS MIDLINE -

Back of Leg I
Back of Leg I Dr. Garima Sehgal Associate Professor “Only those who risk going too far, can possibly find King George’s Medical University out how far one can go.” UP, Lucknow — T.S. Elliot DISCLAIMER Presentation has been made only for educational purpose Images and data used in the presentation have been taken from various textbooks and other online resources Author of the presentation claims no ownership for this material Learning Objectives By the end of this teaching session on Back of leg – I all the MBBS 1st year students must be able to: • Enumerate the contents of superficial fascia of back of leg • Write a short note on small saphenous vein • Describe cutaneous innervation in the back of leg • Write a short note on sural nerve • Enumerate the boundaries of posterior compartment of leg • Enumerate the fascial compartments in back of leg & their contents • Write a short note on flexor retinaculum of leg- its attachments & structures passing underneath • Describe the origin, insertion nerve supply and actions of superficial muscles of the posterior compartment of leg Introduction- Back of Leg / Calf • Powerful superficial antigravity muscles • (gastrocnemius, soleus) • Muscles are large in size • Inserted into the heel • Raise the heel during walking Superficial fascia of Back of leg • Contains superficial veins- • small saphenous vein with its tributaries • part of course of great saphenous vein • Cutaneous nerves in the back of leg- 1. Saphenous nerve 2. Posterior division of medial cutaneous nerve of thigh 3. Posterior cutaneous -

Bones of the Skeletal System
BIOLOGY 211: HUMAN ANATOMY & PHYSIOLOGY ********************************************************************************************************* BONES OF THE SKELETAL SYSTEM ********************************************************************************************************** Reference: Saladin, KS: Anatomy & Physiology, The Unity of Form and Function, 6th ed. (2012) or 7th ed. (2015) Please review Chapters 7 & 8 before beginning this lab. INTRODUCTION The skeletal system has a number of important functions in the human body. It is the framework around which the body is organized, it provides levers for muscles to pull against, and it surrounds and protects many soft organs. Equally important, bones serve as a "buffer" in which calcium and other ions can be deposited and withdrawn according to the changing needs of the body, and they are the site of almost all blood cell production. Contrary to our popular conceptions, bones are not rigid, inflexible structures: they are constantly changing, and can have a remarkable degree of flexibility before they break. The organs of the skeletal system are the bones and joints, and like all organs are composed of different types of tissue. Although we tend to classify them into "types" such as "long bones", "flat bones", etc., each is in fact unique and ideally suited to its particular location and function. We classify bones as belonging to either: a) the axial skeleton (head and trunk) b) the appendicular skeleton (arms and legs), However, you should always bear in mind that the entire skeletal system functions as a unit. If you look at any bone, you will see that it is rarely flat or smooth. Bones have a variety of bumps, grooves, holes, etc. which allow them to serve their specific functions. -
Getting a Leg up on Land
GETTING A LEG UP in the almost four billion years since life on earth oozed into existence, evolution has generated some marvelous metamorphoses. One of the most spectacular is surely that which produced terrestrial creatures ON bearing limbs, fingers and toes from water-bound fish with fins. Today this group, the tetrapods, encompasses everything from birds and their dinosaur ancestors to lizards, snakes, turtles, frogs and mammals, in- cluding us. Some of these animals have modified or lost their limbs, but their common ancestor had them—two in front and two in back, where LAND fins once flicked instead. Recent fossil discoveries cast The replacement of fins with limbs was a crucial step in this transfor- mation, but it was by no means the only one. As tetrapods ventured onto light on the evolution of shore, they encountered challenges that no vertebrate had ever faced be- four-limbed animals from fish fore—it was not just a matter of developing legs and walking away. Land is a radically different medium from water, and to conquer it, tetrapods BY JENNIFER A. CLACK had to evolve novel ways to breathe, hear, and contend with gravity—the list goes on. Once this extreme makeover reached completion, however, the land was theirs to exploit. Until about 15 years ago, paleontologists understood very little about the sequence of events that made up the transition from fish to tetrapod. We knew that tetrapods had evolved from fish with fleshy fins akin to today’s lungfish and coelacanth, a relation first proposed by American paleontologist Edward D.