Quality of Life in Individuals Surgically Treated for Congenital
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

NEWSLETTER a Quarterly Publication of National Centre for Non-Destructive Testing
NEWSLETTER A quarterly publication of National Centre for Non-destructive Testing, Scientific and Engineering Services Dte., Pakistan Atomic Energy Commission Issue No 29 July-September,2002 Back to Main Contents Editorial Tube Plugging Criteria for Heat Exchangers, Boilers and Condensers, etc. Application of Mechanized Ultrasonic Testing in lieu of Radiographic Testing during the Construction of Pipeline for Petroleum Products Seminars on NDT o Experience of WAPDA using NDT as a Tool for Turbine Maintenance o The Role of NDT Technology in the Industrial Development of Pakistan Investiture of PASNT o PASNT Website o Training Courses Conducted o Training Courses Planned for 2003 o Happy News o Global Harmonization of NDT Certification under ISO- 9712 o Industrial NDT Services o In-service Inspection of CHASNUPP Conventional Island (CI) by NCNDT o International NDT News o Foreign Assignment o Visitors Gallery o Visit of NCNDT & CHASNUPP Officers o Private Advertisement EDITORIAL Last issue of this Newsletter was brought out in a new getup. Snaps of members of the Editorial Board were added. Table of contents was included (Previously we faced difficulty in referring to a news item that appeared in a certain issue and had to browse through the pages of many issues in order to locate a desired news). Similarly, titles like International NDT News, Visitors gallery and account of Visits of National Centre for Non-destructive Testing (NCNDT) Personnel were included. This gave new dimensions to the scope of our Newsletter. All this was possible by the contribution of ideas given by the members of newly constituted Editorial Board. It is felt that the readers would have appreciated it. -

Power Plant) 12Th November, 2012
Appendix-C15.5-8 Materials for Stakeholder meeting 1st Stakeholder meeting (Power plant) 12th November, 2012 - 1 - - 2 - gvZvievwo 2x600 †gtIt KqjvwfwËK Zvc we`¨yr †K›`ª I Avbylw½K myweavw` wbg©vY cÖKí ‡Kvj cvIqvi †Rbv‡ikb †Kvt evsjv‡`k wjt (wmwcwRwmweGj) 1 ‡÷K‡nvìvi mfv, b‡f¤^i 2012 D‡Ïk¨ cÖKí mswk−ó¯’vbxq RbMY I Ab¨vb¨ †÷K‡nvìvi‡`i g‡bvfve m¤ú‡K© Av‡jvPbv Kiv 2 - 3 - cÖK‡íi cUf~wg I cÖ‡qvRbxqZv 40,000 37,500 35,000 32,500 30,000 27,500 25,000 22,500 20,000 17,500 15,000 12,500 10,000 7,500 5,000 2,500 0 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2021 2022 2023 2024 2025 2026 2027 2028 2029 2030 Gas-Ex Gas-New Coal-D Coal-I Oil-Ex Oil-New Nuclear Hydro/RE Cross border Demand (GP-GDP7%, U) Required Supply Capacity µgea©gvb we`¨y‡Zi Pvwn`v c~i‡Yi Rb¨ A‡bK eo eo we`¨yr †K›`ª ¯’vcb `iKvi 3 cÖK‡íi cUf~wg I cÖ‡qvRbxqZv ‡`kxq Kqjv D‡Ëvjb (AvcvZZ) ¯’wMZ ‡Nvlbv Avg`vwbK…Z Kqjv wfwËK we`¨yr †K›`ª Dbœqb 4 - 4 - mgx¶vi D‡Ïk¨ cÖ¯—vweZ cÖK‡íi ev¯—evq‡bi Rb¨ KvwiMwi, cwi‡ek, B‡KvbwgK I Avw_©K w`K we‡ePbv c~e©K m¤¢ve¨Zv we‡k−lY PÆMÖvg A‡j KqjvwfwËK we`¨yr †K›`ª / mÂvjY jvBb wbg©vY 5 cÖK‡íi cwiwa . 2x600†gtIt KqjvwfwËK we`¨yr †K›`ª . -

Zaman, in His Headquarters Near the Frontier. Col. Shams Said There Were
401 Zaman, in his headquarters near the frontier. Col. Shams said there were frequent mortar exchanges with the Indian troops over the border-always, he said, begun by the Indians. "They certainly need us here to defends them," he said. "These Bengalis don't know how to fight. Now, I come from the North- West Frontier, where fighting is in our blood. I have been using a rifle since I was ten. We've got guts. CoL. Shams directed the military operations of the past three months in this area, beginning with the "securing" of Khulna town during the period March 25-29. He told me that it was only in the past month that his troops had been able to get the upper hand all over the district from "miscreants and rebels". It appears that it was Shams who began the system of razakars by the distributing police rifles to civilians in Khulna-"good chaps, good Muslims and loyal Pakistanis" he explained. There are now, according to the military authorities, 5,000 razakars in East Pakistan, 300 of them in Khulna district. They are paid Rs 3 a day (25 pence at the official rate) and receive seven days' training which appears to consist entirely of learning how to shoot a police Lee Enfield rifle. Their work consists of "security checks'-guiding the West Pakistan troops to the homes of supporters of the Awami League. They are supposed to be under the orders of local "peace committees" which are selected by the military authorities on a similar basis of "loyalty to Pakistan". -

List of Shareholders Having Unclaimed Or Undistributed Or Unsettled Cash Dividend for the Year 2013 Nominee(S), If Amount of Dividend Sl
Mercantile Bank Limited, Share Department, Board Division, Head Office, Dhaka List of shareholders having unclaimed or undistributed or unsettled cash dividend for the year 2013 Nominee(s), if Amount of dividend Sl. # Name of Shareholder Father’s name Mother’s name Permanent & contact address Year of dividend B.O. account / Folio Number any inTk. 1 Samina Nasreen 23/2, East Nayatola Dhaka Not available 2013 00128 1,378.21 2 Md.Humayun Kabir Late Md. Mobaswer Ali Green Delta Ins.Co.Ltd., Nawabpur Road Ranch Dhaka Not available 2013 00342-1301020000172237 5,127.36 3 A. Hasib House # 53, Road # 12/A, Dhanmondi Dhaka Not available 2013 00394 123.38 4 Yusuf Saeed Late Hasan Saeed Plot # 6, Road # 137, Flat # A2, Gulshan-1 Dhaka Not available 2013 00510 2,350.24 Road # 7, House # 10, Block # Kha Pc Culture Housing, 5 Rasad Rahman Md. Atiar Rahman Not available 2013 00516 488.51 Mohammedpur Dhaka 1207 6 Faisal Alim Abdul Alim House # 378 Road # 28, New Dohs Mohakhali Dhaka Not available 2013 00565 2,350.24 7 Md. Kazi Babul Md. Hashem Kazi Plot # 13/14, Road # 06, Senpara Parbata Mirpur Dhaka Not available 2013 00639 3,633.38 8 Md.Farid Uddin Ahmmed Mohammad Faruque 55, Motijheel C/A Zarin Mansion, 2Nd Floor Dhaka 1000 Not available 2013 00655-1301020000204389 1,324.24 16/19, Ground Floor Tajmohal Rd. Block-C Mohammadpur 9 Josephine Rodrigues Not available 2013 00735 719.92 Dhaka 16/19, Ground Floor Tajmohal Rd. Block-C Mohammadpur 10 Martin Rodrigues Not available 2013 00736 1,378.21 Dhaka 11 Ratan Kumar Saha Saha Dental Clinic, Tulapatti Naogaon -
6455.Pdf, PDF, 1.27MB
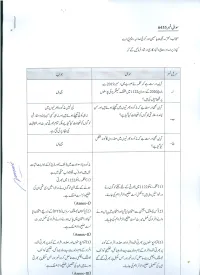
Overall List Along With Domicile and Post Name Father Name District Post Shahab Khan Siraj Khan PESHAWAR 01. Station House Incharge (BPS-16) Sana Ullah Muhammad Younas Lower Dir 01. Station House Incharge (BPS-16) Mahboob Ali Fazal Rahim Swat 01. Station House Incharge (BPS-16) Tahir Saeed Saeed Ur Rehman Kohat 01. Station House Incharge (BPS-16) Owais Qarni Raham Dil Lakki Marwat 01. Station House Incharge (BPS-16) Ashfaq Ahmad Zarif Khan Charsadda 01. Station House Incharge (BPS-16) Saud Khan Haji Minak Khan Khyber 01. Station House Incharge (BPS-16) Qamar Jan Syed Marjan Kurram 01. Station House Incharge (BPS-16) Kamil Khan Wakeel Khan PESHAWAR 01. Station House Incharge (BPS-16) Waheed Gul Muhammad Qasim Lakki Marwat 01. Station House Incharge (BPS-16) Tanveer Ahmad Mukhtiar Ahmad Mardan 01. Station House Incharge (BPS-16) Muhammad Faheem Muhammad Aslam PESHAWAR 01. Station House Incharge (BPS-16) Muslima Bibi Jan Gul Dera Ismail Khan 01. Station House Incharge (BPS-16) Muhammad Zahid Muhammad Saraf Batagram 01. Station House Incharge (BPS-16) Riaz Khan Muhammad Anwar Lower Dir 01. Station House Incharge (BPS-16) Bakht Taj Abdul Khaliq Shangla 01. Station House Incharge (BPS-16) Hidayat Ullah Fazal Ullah Swabi 01. Station House Incharge (BPS-16) Wajid Ali Malang Jan Mardan 01. Station House Incharge (BPS-16) Sahar Rashed Abdur Rasheed Mardan 01. Station House Incharge (BPS-16) Afsar Khan Afridi Ghulam Nabi PESHAWAR 01. Station House Incharge (BPS-16) Adnan Khan Manazir Khan Mardan 01. Station House Incharge (BPS-16) Liaqat Ali Malik Aman Charsadda 01. Station House Incharge (BPS-16) Adnan Iqbal Parvaiz Khan Mardan 01. -

Download Download
REVIEWERS FOR KMUJ 1. Aakif Ullah Khan, Nuclear 26. Alaptagin Khan, Psychiatry, USA 52. Apoorva Pallam Reddy, Obstetrics/ Medicine, Swat Gynaecology, India 27. Alam Ibrahim Siddiqui, Neurology, 2. Aamer Shehzad, Internal Medicine, Larkana 53. Arshad Hussain, Endocrinology, Rawalpindi Peshawar 28. Alay Ahmad, Psychology, Peshawar 3. Aamir Bilal, Cardiothoracic 54. Arshad Iqbal, Ophthalmology, Swat 29. Alia Hisam, Community Medicine, Surgery, Peshawar Islamabad 55. Arshad Javaid, Pulmonology, 4. Aamir Ghafoor Khan, Peshawar 30. Ali Hassan Rajput, Neurology, Gastroenterology, Peshawar Saudi Arabia 56. Arshad Khushdil, Pediatrics, Skardu 5. Aasim Rehman, Rheumatology, 31. Ali Jawa, Endocrinology, Islamabad 57. Asaad Javaid, Operative Dentistry, USA Karachi 32. Ali Madeeh Hashmi, Psychiatry, 6. Aatik Arsh, Physiotherapy, Lahore 58. Asad Tamizuddin Nizami, Peshawar Psychiatry, Rawalpindi 33. Ali Zulqernain, Psychiatry, 7. Abdul Baseer, Cardiovascular Sargodha 59. Asadullah Kundi, Cardiology, Surgery, Peshawar Karachi 34. Aliya Ahmed, Anaesthesiology, 8. Abdul Jabbar, Medicine/ Karachi 60. Asghar H. Asghar, Oncology, Endocrinology, UAE Karachi 35. Aman Ullah Pathan, Internal 9. Abdul Kareem A. Mahmood, Medicine, USA 61. Asher Ahmed Mashhood, Derma- Community Medicine, Iraq tology, Peshawar 36. Aman Ullah, Microbiology, 10. Abdul Malik, Cardiovascular Peshawar 62. Asif Ali, Histopathology, Peshawar Surgery, Peshawar 37. Amanat Khan, Anaesthesiology, 63. Asif Ullah Khan, Biochemistry/ 11. Abdul Malik, Neurology, Karachi Rawalpindi Bioinformatics, Peshawar 12. Abdul Rehman Arshad, Medicine, 38. Amber Ashraf, Cardiology/ 64. Asif Ullah, Cardiology, Kohat Azad Kashmir Medicine, Peshawar 65. Asifa Majeed, Biochemistry, 13. Abdul Sahib Khan, Anatomy/ 39. Ambreen Kazi, Community Rawalpindi General Surgery, Kohat Medicine, Karachi 66. Asma Shaukat, Chemical 14. Abdur Rahim Khan, Dermatology, 40. Ameena Saba Awan, Pediatrics, Pathology, Bahawalpur Peshawar Kohat 67. -

Awareness, Use and Perceptions About E-Cigarettes Among Adult Smokers in Karachi, Pakistan
eCommons@AKU Section of Pulmonary & Critical Care Department of Medicine January 2018 Awareness, use and perceptions about E-cigarettes among adult smokers in Karachi, Pakistan. Maryam Sarfraz Aga Khan University Hamza Abdur Rahim Khan Aga Khan University Amna Urooba Aga Khan University Zainab Manan Aga Khan University Omar Irfan Aga Khan University See next page for additional authors Follow this and additional works at: https://ecommons.aku.edu/ pakistan_fhs_mc_med_pulm_critcare Part of the Critical Care Commons, and the Pulmonology Commons Recommended Citation Sarfraz, M., Khan, H. A., Urooba, A., Manan, Z., Irfan, O., Nadeem, R., Baqir, H., Farooq, S., Khan, Z., Khan, J., saleem, S. (2018). Awareness, use and perceptions about E-cigarettes among adult smokers in Karachi, Pakistan.. JPMA. The Journal of the Pakistan Medical Association, 68(1), 147-153. Available at: https://ecommons.aku.edu/pakistan_fhs_mc_med_pulm_critcare/53 Authors Maryam Sarfraz, Hamza Abdur Rahim Khan, Amna Urooba, Zainab Manan, Omar Irfan, Ramlah Nadeem, Huma Baqir, Saad Farooq, Zarrar Khan, Javaid Khan, and Sarah saleem This article is available at eCommons@AKU: https://ecommons.aku.edu/pakistan_fhs_mc_med_pulm_critcare/53 147 STUDENTS CORNER KAP STUDY Awareness, use and perceptions about E-cigarettes among adult smokers in Karachi, Pakistan Maryam Sarfraz, 1 Hamza Abdur Rahim Khan, 2 Amna Urooba, 3 Zainab Manan, 4 Omar Irfan, 5 Ramlah Nadeem, 6 Huma Baqir, 7 Saad Farooq, 8 Zarrar Khan, 9 Javaid Ahmed Khan, 10 Sarah Saleem 11 Abstract Objective: To estimate the prevalence of awareness, current use and intention to use of e-cigarettes among adult smokers. Methods: This cross-sectional survey was carried out at the Aga Khan University Hospital, Karachi, from July to August 2016, and comprised people aged above 18 years who had smoked more than 100 cigarettes in their lifetime. -

THE SENATE of PAKISTAN DEBATES OFFICIAL REPORT Monday, September 27, 2010 (64 Th Session) Volume VIII No
THE SENATE OF PAKISTAN DEBATES OFFICIAL REPORT Monday, September 27, 2010 (64 th Session) Volume VIII No. 06 (Nos. 01-10) CONTENTS Pages 1. Recitation from the Holy Quran ……………....……….. 1 2. Leave of Absence.……………………………………… 2-5 3. Presentation of the Reports ……………………………. 6 4. Discussion on Law and Order Situation in the country... 7-10 points of order: a) By Senator Zafar Ali Shah regarding territorial violation by the NATO Forces……. 11-12 b) By Senator Abdul Nabi Bangesh about official authentic report on Target Killing.----- 13-52 Printed and Published by the Senate Secretariat, Islamabad. Volume VIII SP. VIII ( 06 )/2010 No.06 130 SENATE OF PAKISTAN SENATE DEBATES Monday, September 27, 2010 The Senate of Pakistan met in the Senate Hall (Parliament House) Islamabad, at thirty minutes past four in the evening with Mr. Chairman (Mr. Farooq Hamid Naek) in the Chair. ---------------- Recitation from the Holy Quran -.. ! ª "#$% // - & ' (" ! () *#+$ $,% 0 ; 2( >? )% @ A - +"= ) 9:% - 123 45 %(6$% 78$ < ‹ G H( IJ 5% G 2(#$% >B$ CD EF$ ! / OPH 3 %6Q $, O#$% A - NK L 3 IM3 45 H( IJ A T R H S()$% >B$ 7*$ ! 7& - / G . 2 @$ N = ; ; :U ! / Q, 3 G ! / Q, ) =& :U% +ª $, G R=#A 8 D 8 R R 8 D 8 =3SH C )=KO 6J =C<;=?PI ;L=CB=B=M;=?E Q Q =4=NQ E;<= >FG = ?H = @;= ABI = B6 J C<; : 3567 4 9 8 O O X 9fg O kl e m R 8 =[bc =C<;=?\P L=4Q =] =BQ =^;=?_ dEP =VL=`hi -

List of Mbbs Graduates for the Year 1997
KING EDWARD MEDICAL UNIVERSITY, LAHORE LIST OF MBBS GRADATES 1865 – 1996 1865 1873 65. Jallal Oddeen 1. John Andrews 31. Thakur Das 2. Brij Lal Ghose 32. Ghulam Nabi 1878 3. Cheytun Shah 33. Nihal Singh 66. Jagandro Nath Mukerji 4. Radha Kishan 34. Ganga Singh 67. Bishan Das 5. Muhammad Ali 35. Ammel Shah 68. Hira Lal 6. Muhammad Hussain 36. Brij Lal 69. Bhagat Ram 7. Sahib Ditta 37. Dari Mal 70. Atar Chand 8. Bhowani Das 38. Fazi Qodeen 71. Nathu Mal 9. Jaswant Roy 39. Sobha Ram 72. Kishan Chandra 10. Haran Chander Banerji 73. Duni Chand Raj 1874 74. Ata Muhammad 1868 40. Sobhan Ali 75. Charan Singh 76. Manohar Parshad 11. Fateh Singh 41. Jowahir Singh 12. Natha Mal 42. Lachman Das 1879 13. Ram Rich Pall 43. Dooni Chand 14. Bhagwan Das 44. Kali Nath Roy 77. Sada Nand 15. Mul Chand 45. Booray Khan 78. Mohandro Nath Ohdidar 16. Mehtab singh 46. Jodh Singh 79. Jai Singh 47. Munna Lal 80. Khazan Chand 48. Mehr Chand 81. Dowlat Ram 1869 49. Jowala Sahai 82. Jai Krishan Das 17. Taboo Singh 50. Gangi Ram 83. Perama Nand 18. Utum Singh 52. Devi Datta 84. Ralia Singh 19. Chany Mal 85. Jagan Nath 20. Esur Das 1875 86. Manohar Lal 21. Chunnoo Lal 53. Ram Kishan 87. Jawala Prasad 54. Kashi Ram 1870 55. Alla Ditta 1880 22. Gokal Chand 56. Bhagat Ram 88. Rasray Bhatacharji 57. Gobind Ram 89. Hira Lal Chatterji 90. Iktadar-ud-Din 1871 1876 91. Nanak Chand 23. Urjan Das 58. -

Composition and Role of the Nobility (1739-1761)
COMPOSITION AND ROLE OF THE NOBILITY (1739-1761) ABSTRACT OF THE THESIS SUBMITTED FOR THE AWARD OF THE DEGREE OF Boctor of ^l)iIo^op}|p IN HISTORY BY MD. SHAKIL AKHTAR Under the Supervision of DR. S. LIYAQAT H. MOINI (Reader) CENTRE OF ADVANCED STUDY DEPARTMENT OF HISTORY ALIGARH MUSLIM UNIVERSITY ALIGARH (INDIA) 2008 ABSTRACT Foregoing study ' composition and role of the Nobility (1739- 1761)', explore the importance of Nobility in Political, administrative, Sicio-cultural and economic spheres. Nobility , 'Arkan-i-Daullat' (Pillars of Empire) generally indicates'the'class of people, who were holding hi^h position and were the officers of the king as well as of the state. This ruling elite constituting of various ethnic group based on class, political sphere. In Indian sub-continent they served the empire/state most loyally and obediently specially under the Great Mughals. They not only helped in the expansion of the Empire by leading campaign and crushing revolt for the consolidation of the empire, but also made remarkable and laudable contribution in the smooth running of the state machinery and played key role in the development of social life and composite culture. Mughal Emperor Akbar had organized the nobility based on mgnsabdari system and kept a watchful eye over the various groups, by introducing local forces. He had tried to keep a check and balance over the activities, which was carried by his able successors till the death of Aurangzeb. During the period of Later Mughals over ambitious, self centered and greedy nobles, kept their interest above state and the king and had started to monopolies power and privileges under their own authority either at the court or in the far off provinces. -

Daily List for Tuesday, 28 November, 2017 Motion
_ 1 _ PESHAWAR HIGH COURT, PESHAWAR DAILY LIST FOR TUESDAY, 28 NOVEMBER, 2017 MR. JUSTICE QAISER RASHID KHAN & Court No: 3 BEFORE:- JUSTICE MS. MUSARRAT HILALI MOTION CASES 1. CM Rest 200/2017 Manzoor Hussain Abdul Rauf Rohaila With C.M V/s 325/2017(in FAB United Bank Limited 17/2014) 2. W.P 547/2015 Abdur Rasheed Shahzada Irfan Zia, Javed Iqbal (Services)(Promot V/s (Date By Court) Gulbela ion) Secretary to Govt of Pakistan, Ministry of Interior and others Umar Zafran, A.G, Muhammad Hayat Khan 3. W.P 1122/2015 Ismail and others Javed Ali Muhammadzai (Services)(Promot V/s (Date By Court) ion Vacant Post) Secretary, LGE & RDD KPK and A.A.G, Kashif Jan others 4. W.P 758/2016 The Sub Inspectors through Khushdil Khan (Services)(Upgrad General Secretary ation) V/s Asghar Khan Kundi, A.G The Govt of KPK through Chief Secretary and others i W.P 759/2016 The Inspector through General Khushdil Khan V/s Upgradation Secretary Asghar Khan Kundi The Govt of KPK through Chief Secretary and others ii W.P 760/2016 Assistant Registrars through Khushdil Khan V/s Upgradation General Secretary Asghar Khan Kundi The Govt of KPK through Chief Secretary and others 5. W.P 1444/2016 Hazrat Ali Ghulam Nabi (Services)(Upgrad V/s ation BPS-11) Govt of KPK through Secretary Sabahuddin Khattak Local Govt and others MIS Branch,Peshawar High Court Page 1 of 54 Report Generated By: C f m i s _ 2 _ DAILY LIST FOR TUESDAY, 28 NOVEMBER, 2017 MR. -

Pakistan Journal of Library & Information Science
Pakistan Journal of Library & Information Science, 12 (2011) Available at http://pu.edu.pk/home/journal/8 Pakistan Journal of Library & Information Science ISSN 1680-4465 Abdur Rahim Khan Corner Abdur Rahim Khan as I knew hhhimhimimim (1) MumtMumtazaz A. Anwar Department of Library and Information Science, University of the Punjab, Lahore, Pakistan Email: [email protected] I was lucky to have met three top leaders of the profession and, in time, developed very close relationship with them – amounting to almost friendship. They were: Abdur Rahim Khan (ARK), Anis Khurshid, and Abdus Subuh Qasimi. The first one who I knew the most has been the last to depart. The situations, circumstances and the time-span in which I interacted with these seniors were different in each case but we spent hours together discussing, apart from personal interaction, the past, contemporary and future issues of Pakistani librarianship. Each one of them was deeply involved in professional activities and was part of the history of the profession. During these interactions and the discussions that followed, I learned a great deal about many unrecorded events of our professional history (2). My entry into the profession was accidental. I had planned to study for the master’s degree in Economics. A nasty fever delayed my visit to Lahore to apply for admission on time. It seemed that I had lost my chance to pursue the studies that I had planned for. I tried to think of some other options. I discovered that even the admission to the B. Ed. class in the Central Training College was closed.